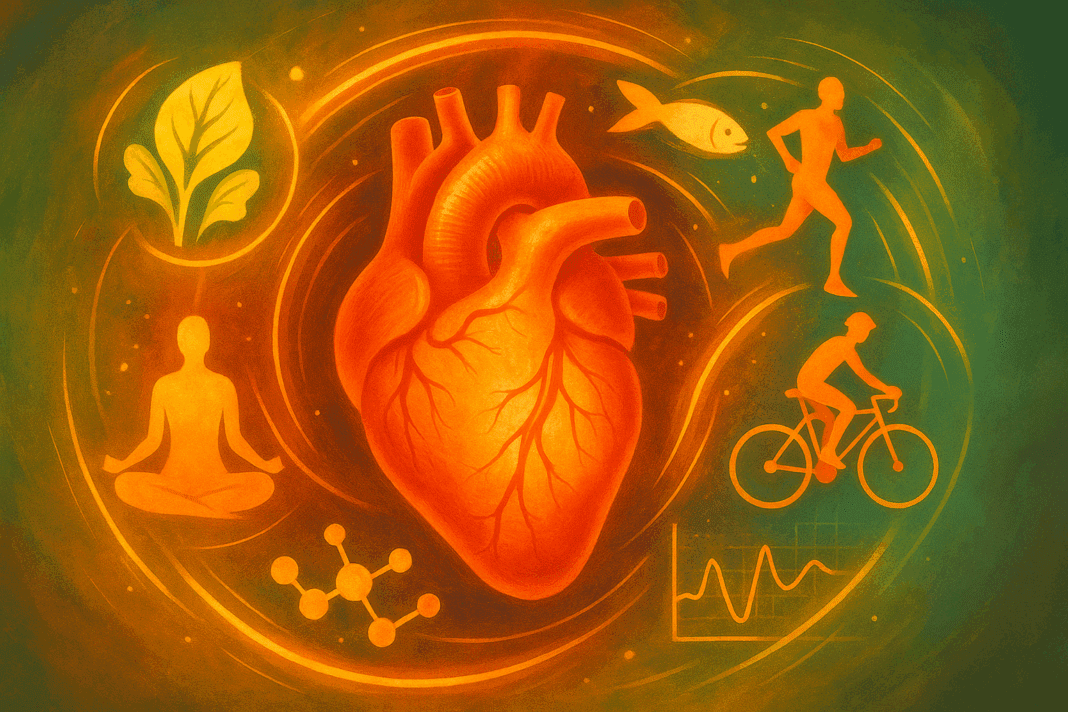
In the modern era of rising chronic disease rates, cardiovascular health remains a cornerstone of long-term vitality and physical performance. For individuals seeking to enhance endurance and maintain robust heart function, the question is not only how to boost fitness but also how to protect the cardiovascular system in a sustainable and natural way. A growing body of scientific research supports a variety of cardiovascular disease interventions that not only prevent complications but also actively support endurance capacity, circulation, and metabolic health. These heart disease interventions are more than just treatment strategies—they are holistic approaches designed to prevent decline, enhance resilience, and empower individuals to take proactive control of their well-being.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice
Understanding the Science Behind Cardiovascular Disease and Endurance
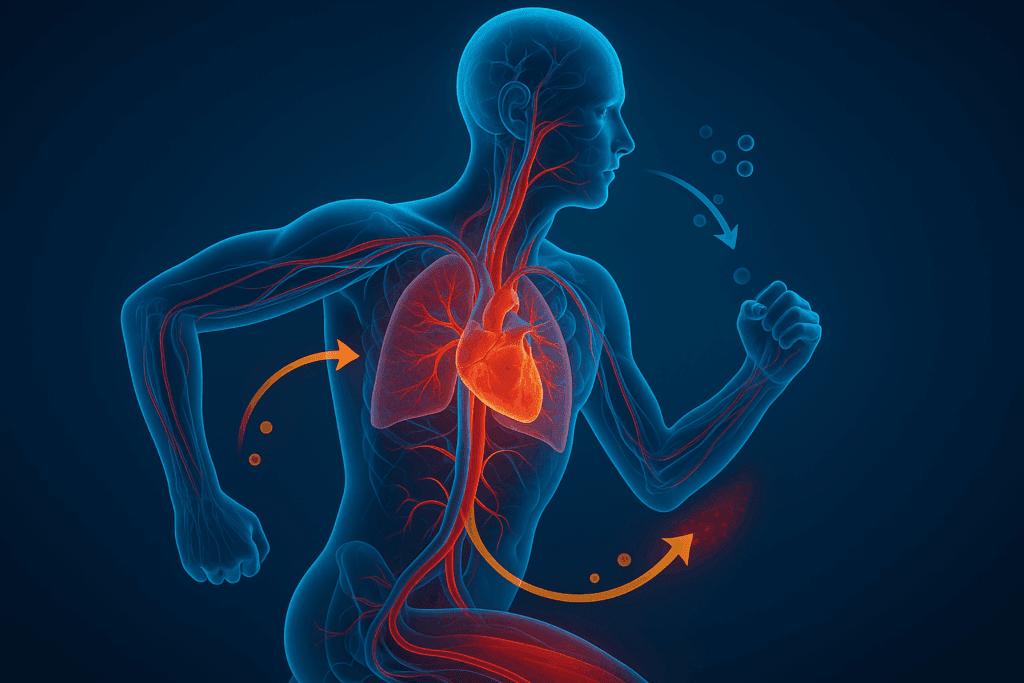
At the heart of every physical activity lies the cardiovascular system. The heart, arteries, veins, and lungs work in harmony to deliver oxygen and nutrients to muscles during exertion. When the cardiovascular system is compromised, endurance suffers, and the risk of fatigue, injury, and long-term health issues rises. This underscores the vital connection between endurance performance and cardiovascular disease prevention. Cardiovascular disease (CVD) is not a singular condition but an umbrella term that encompasses a range of disorders affecting the heart and blood vessels, including coronary artery disease, heart failure, arrhythmias, and stroke. Understanding how CVD interventions impact not just disease prevention but also stamina and athletic performance is crucial for those pursuing both health and high function.
Scientific data has consistently shown that targeted heart disease interventions—particularly those grounded in lifestyle changes—can lead to measurable improvements in both cardiovascular biomarkers and endurance capacity. Lowering blood pressure, improving lipid profiles, stabilizing blood sugar, and reducing arterial inflammation all contribute to a heart that can pump more efficiently and recover faster. These benefits directly translate to increased stamina, improved oxygen delivery, and greater resilience during physical activity. Importantly, such improvements are not only achievable through medications but also through evidence-based lifestyle and nutritional strategies that are accessible and sustainable.
How Disease Prevention Programs Try to Reduce Cardiovascular Disease
The foundation of most modern disease prevention programs lies in education, behavior change, and community-based intervention. But beyond these broad strategies, there are specific mechanisms through which these programs try to reduce cardiovascular disease at both the individual and population levels. First and foremost, these initiatives promote risk awareness and early detection. By helping individuals recognize early warning signs, such as elevated cholesterol or hypertension, prevention programs empower them to take action before damage becomes irreversible.
In practice, this often means supporting smoking cessation, facilitating dietary improvements, encouraging physical activity, and providing stress management tools. These approaches may sound simple, but they are deeply rooted in research and tailored to the individual’s unique risk profile. For example, someone with a family history of heart disease may benefit from earlier cholesterol screening and more aggressive lifestyle changes, even if they are asymptomatic. Disease prevention programs also often include access to coaching, peer support, and tools like fitness trackers or meal planning apps—all of which increase engagement and accountability. Ultimately, how disease prevention programs try to reduce cardiovascular disease is by enabling people to modify the drivers of CVD before they escalate into life-threatening conditions.
Moreover, these programs are increasingly integrated into workplaces, schools, and public policy. From walking initiatives to healthy cafeteria options, environments are being reshaped to support heart-healthy behaviors. Digital health platforms now allow for remote monitoring of blood pressure and activity levels, helping participants remain connected to their goals. These technological advancements reflect a broader shift toward preventive healthcare, where proactive measures are seen not as optional extras but as essential components of long-term cardiovascular care.

Nutrition as a Core Component of Heart Disease Interventions
Among all the lifestyle factors that influence cardiovascular health, nutrition stands out as both a risk factor and a solution. The role of diet in CVD interventions is well-documented, with substantial evidence supporting the adoption of heart-healthy dietary patterns such as the Mediterranean diet, the DASH diet, and plant-forward whole food approaches. These dietary strategies are characterized by high intakes of vegetables, fruits, whole grains, legumes, nuts, seeds, and healthy fats, such as those from olive oil and fatty fish. They also emphasize the reduction of saturated fats, trans fats, added sugars, and sodium.
Such nutrition-based heart disease interventions are not merely theoretical. Numerous randomized controlled trials have shown that individuals who follow these eating patterns experience reductions in blood pressure, LDL cholesterol, triglycerides, and systemic inflammation—all of which contribute to lower cardiovascular risk. At the same time, these diets support improved energy metabolism, more stable blood glucose levels, and enhanced recovery from exercise. This means they also play a critical role in supporting athletic performance and long-duration endurance efforts.
For instance, athletes who adopt a Mediterranean-style eating plan often report better stamina, quicker recovery, and more consistent performance. This is not surprising, given that such diets provide antioxidants, micronutrients, and anti-inflammatory compounds that enhance vascular function and mitochondrial efficiency. In this way, cardiovascular disease interventions rooted in nutrition serve a dual purpose: they protect the heart and optimize the body’s ability to perform under physical stress.

The Power of Physical Activity in CVD Interventions
Exercise is perhaps the most potent of all cardiovascular disease interventions. Its benefits are immediate and cumulative, affecting nearly every system in the body. For individuals focused on building endurance, consistent physical activity improves heart rate variability, increases cardiac output, and enhances VO2 max—the maximal oxygen uptake that directly correlates with endurance capacity. The physiological adaptations to exercise make the heart stronger and more efficient, enabling it to pump more blood with each beat and reduce the overall strain on the circulatory system.
From a preventative standpoint, regular physical activity also reduces the risk of obesity, type 2 diabetes, and hypertension—three major contributors to cardiovascular disease. It improves lipid profiles, supports better blood sugar control, and enhances endothelial function, which keeps arteries flexible and responsive. Importantly, the most effective CVD interventions recognize that not all exercise must be high-intensity or long-duration to be beneficial. Walking, resistance training, yoga, and moderate cycling can all contribute to cardiovascular improvement when practiced consistently.
For individuals recovering from cardiac events or managing existing risk factors, structured cardiac rehabilitation programs provide a safe and effective environment to regain strength and improve outcomes. These medically supervised programs combine monitored exercise with education, nutritional guidance, and psychological support. They demonstrate how exercise can be tailored to the needs of the individual and integrated into a broader strategy for long-term heart health and endurance performance.
Stress Reduction and Its Role in Heart Health
The role of psychological stress in cardiovascular disease is often underestimated, yet chronic stress can be a silent driver of long-term cardiovascular dysfunction. Elevated stress hormones such as cortisol and adrenaline contribute to higher blood pressure, increased heart rate, and systemic inflammation—all of which increase the burden on the cardiovascular system. This makes stress management an essential, though sometimes overlooked, part of heart disease interventions.
Effective cardiovascular disease interventions often incorporate mind-body strategies such as meditation, deep breathing, biofeedback, and progressive muscle relaxation. These practices have been shown to activate the parasympathetic nervous system, promoting a state of rest and recovery that directly benefits heart rate variability and blood pressure regulation. Over time, individuals who regularly engage in stress-reducing practices tend to report not only improved mental well-being but also better endurance, fewer cardiovascular symptoms, and enhanced recovery after exercise.
Additionally, social support plays a key role in mitigating stress and improving cardiovascular outcomes. Studies have found that individuals with strong social connections are less likely to experience adverse cardiovascular events and tend to recover more quickly from illness. Whether through group fitness classes, community health programs, or virtual support networks, fostering connection is a powerful component of CVD interventions that promote both resilience and motivation.

Emerging Supplements and Natural Therapies for Cardiovascular Support
While lifestyle changes remain the gold standard in preventing and managing heart disease, emerging evidence suggests that certain natural supplements may provide additional support. These interventions should never replace medical care but can be complementary tools when used appropriately and under the guidance of a healthcare provider. Among the most well-researched supplements are omega-3 fatty acids, Coenzyme Q10 (CoQ10), magnesium, and plant-based antioxidants such as resveratrol and quercetin.
Omega-3s from fish oil or algae have been shown to lower triglycerides, reduce inflammation, and support overall heart rhythm stability. CoQ10, a compound involved in mitochondrial energy production, has demonstrated benefits in improving endothelial function and reducing blood pressure, particularly in individuals taking statins. Magnesium, often depleted in modern diets, plays a crucial role in vascular tone and insulin sensitivity. These supplements are increasingly being integrated into cardiovascular disease interventions aimed at enhancing heart function and overall metabolic health.
Botanical extracts like hawthorn berry, garlic, and green tea catechins have also shown promise in early studies for supporting circulation and reducing arterial stiffness. However, the evidence for these natural therapies is still developing, and it is essential to evaluate both the safety and efficacy before incorporating them. When chosen wisely and combined with foundational lifestyle changes, these interventions may offer an additional layer of protection for individuals pursuing endurance goals while safeguarding cardiovascular health.
Personalizing CVD Interventions for Optimal Results
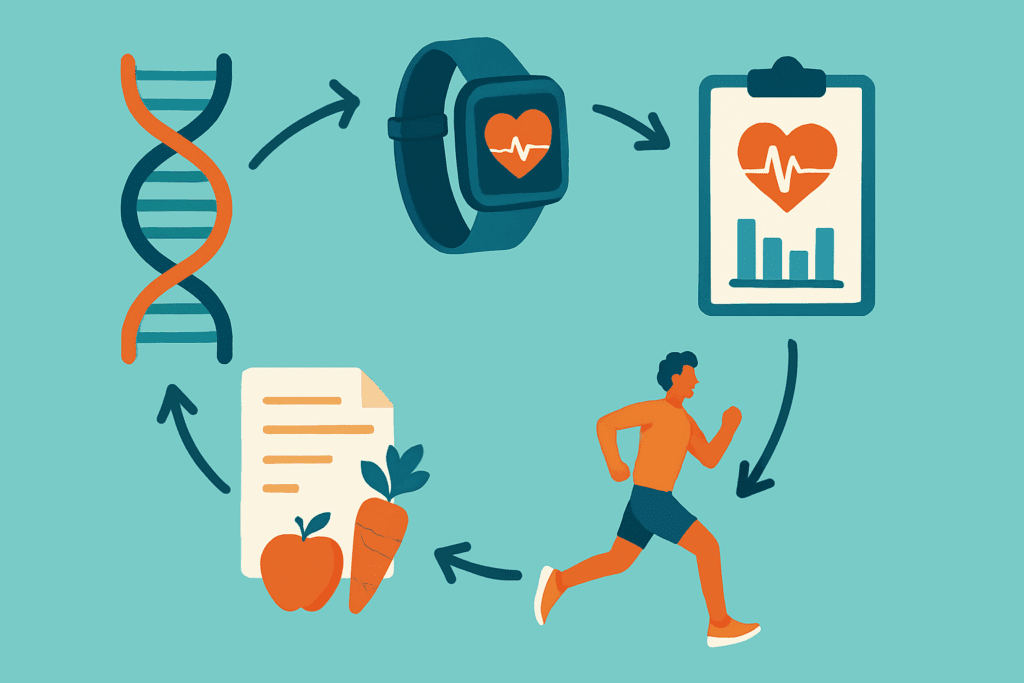
One of the key insights emerging from the latest research is that effective heart disease interventions must be personalized. There is no one-size-fits-all approach when it comes to cardiovascular prevention, particularly for those balancing athletic goals with long-term health. Genetic factors, lifestyle habits, environmental exposures, and even gut microbiota all influence how an individual responds to different interventions. This makes individualized care—often guided by advanced diagnostics and biomarkers—an essential part of successful prevention.
Modern cardiovascular risk assessments go beyond basic cholesterol and blood pressure measurements. They may include coronary calcium scoring, advanced lipid profiling, inflammatory markers like hs-CRP, and even genetic screening for inherited cardiac conditions. By using these tools, clinicians can design targeted prevention strategies that maximize both safety and efficacy. For an endurance athlete, this may mean adjusting training intensity, optimizing micronutrient intake, or addressing subclinical inflammation before it impairs performance.
Personalized CVD interventions also involve careful monitoring and regular reassessment. As the body changes with age, activity, and external factors, so too must the strategies used to protect the heart. Wearable technology, home testing kits, and digital coaching platforms are making it easier than ever to track key metrics and stay engaged in a heart-healthy lifestyle. The result is a more dynamic, responsive, and effective approach to endurance and cardiovascular protection.
The Link Between Cardiovascular Fitness and Cognitive Resilience
An often-overlooked benefit of cardiovascular disease interventions is their impact on brain health. Research continues to show a strong link between heart health and cognitive function, especially as people age. Vascular health directly influences cerebral blood flow, and chronic conditions like hypertension or atherosclerosis are associated with increased risk of cognitive decline, dementia, and stroke. As such, CVD interventions that improve cardiovascular function often carry secondary benefits for mental acuity and emotional stability.
Regular aerobic exercise, in particular, enhances neuroplasticity, supports the growth of new brain cells, and improves memory and executive function. Nutrition plays a role here as well, with heart-healthy diets rich in omega-3s, antioxidants, and polyphenols contributing to reduced neuroinflammation and improved neuronal function. This brain-body connection adds another layer of urgency and motivation for individuals seeking comprehensive lifestyle changes—not only will they protect their heart, but they will also support their long-term cognitive performance and emotional health.
FAQ: Cardiovascular Disease Interventions That Enhance Endurance and Heart Health
1. Can cardiovascular disease interventions also benefit younger individuals with no symptoms? Absolutely. Cardiovascular disease interventions are not solely for those with diagnosed conditions or older adults. In fact, implementing heart disease interventions early in life can significantly reduce the lifetime risk of heart complications. These strategies, when introduced preventively, can enhance vascular elasticity, improve metabolic function, and even boost athletic performance. Younger individuals often overlook early warning signs like elevated stress, irregular lipid profiles, or insulin resistance, which are precursors to more serious issues. By adopting proactive CVD interventions early, such as stress management techniques or dietary improvements, younger people can improve endurance outcomes and build long-term cardiovascular resilience.
2. How do disease prevention programs try to reduce cardiovascular disease in underserved communities? Disease prevention programs play a critical role in bridging health equity gaps, particularly in underserved populations. How disease prevention programs try to reduce cardiovascular disease in these contexts often involves mobile clinics, community health workers, culturally tailored education, and subsidized screenings. These programs address social determinants of health such as food insecurity, lack of access to fitness spaces, and healthcare affordability. By offering multilingual resources and community-based support systems, they foster trust and improve compliance with CVD interventions. Importantly, they also aim to influence policy and infrastructure—like safe walking paths and fresh food markets—which indirectly support heart disease interventions in these populations.
3. What role does sleep quality play in cardiovascular disease interventions? Sleep is often an overlooked element in cardiovascular health, yet it’s a crucial component of any comprehensive intervention plan. Poor sleep has been linked to elevated blood pressure, arterial inflammation, and impaired glucose metabolism, all of which increase cardiovascular risk. Integrating sleep hygiene strategies into heart disease interventions—such as establishing consistent sleep routines, managing light exposure, and limiting stimulants—can drastically improve cardiovascular metrics. High-quality sleep also enhances endurance by supporting muscle recovery, hormonal balance, and immune function. Therefore, innovative CVD interventions increasingly recognize the importance of circadian health as part of their holistic approach.
4. Are there any technological innovations being used in cardiovascular disease interventions today? Yes, technology is transforming how we approach cardiovascular disease interventions across all stages—from prevention to post-recovery. Wearables now track metrics like heart rate variability, oxygen saturation, and even atrial fibrillation in real time, offering early warning signals for cardiac stress. Telehealth platforms allow patients to consult cardiologists remotely and maintain consistent monitoring without geographical constraints. AI-driven analytics can now personalize heart disease interventions by predicting an individual’s response to different lifestyle modifications or medications. These innovations are especially helpful in CVD interventions aimed at improving endurance training, as they help users optimize heart rate zones and recovery patterns with precision.
5. How do psychological factors influence the effectiveness of CVD interventions? Psychological health plays a vital yet often understated role in the success of cardiovascular disease interventions. Chronic anxiety, depression, and even loneliness can contribute to systemic inflammation and hormonal imbalances that worsen heart function. Integrating mental health support into heart disease interventions—through cognitive behavioral therapy, group counseling, or mindfulness-based programs—can enhance both adherence and outcomes. For endurance-focused individuals, managing psychological stress ensures more consistent energy levels and improved recovery times. Therefore, how disease prevention programs try to reduce cardiovascular disease often includes addressing the emotional well-being of patients as a critical part of the intervention process.
6. What is the connection between gut health and heart disease interventions? Emerging research reveals a compelling link between gut microbiota and cardiovascular health. The balance of bacteria in the gut influences lipid metabolism, systemic inflammation, and even blood pressure regulation. Certain cardiovascular disease interventions now include probiotics, prebiotic-rich foods, and fermented products as tools for improving heart function. These dietary shifts not only support digestion but also help lower the risk of atherosclerosis and hypertension. As our understanding of this gut-heart axis expands, more advanced heart disease interventions are expected to personalize nutrition based on microbiome profiles to optimize cardiovascular and endurance outcomes.
7. Can heart disease interventions be tailored for endurance athletes without compromising performance? Definitely. While some CVD interventions are focused on clinical recovery, others are specifically designed to support high-performance individuals like endurance athletes. These may include nutrient timing strategies, inflammation-modulating supplements, and adaptive training regimens that reduce cardiac strain. Cardiovascular disease interventions for athletes often focus on arterial flexibility, oxygen utilization, and recovery metrics rather than disease reversal alone. Monitoring cardiac biomarkers post-exercise and integrating periodized rest cycles are among the nuanced approaches used. Tailoring interventions to athletic needs ensures that the benefits of heart disease prevention are achieved without undermining stamina or peak output.
8. How do disease prevention programs try to reduce cardiovascular disease at the policy level? Policy is a powerful lever in shaping the landscape of cardiovascular health. How disease prevention programs try to reduce cardiovascular disease on a policy level often includes advocating for tobacco control laws, subsidies for healthy food options, and urban planning that supports active transportation. Public health campaigns also promote transparency in food labeling, workplace wellness initiatives, and school-based physical education reforms. These population-level strategies create environments where cardiovascular disease interventions can flourish, making heart-healthy choices more accessible and affordable. When combined with individualized care, these policy shifts significantly improve the long-term success of CVD interventions.
9. What barriers do patients face when engaging with cardiovascular disease interventions, and how can they be overcome? Common barriers include time constraints, misinformation, financial limitations, and a lack of perceived urgency—especially when symptoms are absent. To improve uptake, CVD interventions must be culturally sensitive, affordable, and adaptable to individual lifestyles. Incorporating digital health tools, offering low-cost group programs, and educating through trusted community leaders can enhance engagement. It’s also critical to combat misinformation by ensuring that heart disease interventions are backed by credible sources and explained clearly to patients. When these barriers are addressed proactively, the success rate of cardiovascular disease interventions rises significantly, improving both endurance and health outcomes.
10. What does the future of heart disease interventions look like in the next decade? The future of heart disease interventions is highly personalized, tech-integrated, and prevention-focused. Advances in genetic testing and biomarker analysis will allow clinicians to craft individualized CVD interventions based on predictive risk modeling. Meanwhile, wearable biosensors will continue to provide real-time data on cardiovascular strain, sleep, and recovery, enhancing endurance training protocols. Pharmaceutical developments may also include more targeted therapies with fewer side effects, while plant-based bioactives and adaptogens gain prominence in natural cardiovascular support. As disease prevention programs try to reduce cardiovascular disease and become more integrated with digital ecosystems and behavioral science, the line between medical care and daily lifestyle will increasingly blur—ushering in a new era of proactive heart health management.
Conclusion: Embracing Natural Cardiovascular Disease Interventions for Endurance and Lifelong Heart Health
Ultimately, the path to greater endurance and stronger cardiovascular function is paved with informed, intentional choices. By embracing evidence-based cardiovascular disease interventions—ranging from nutrient-dense diets and consistent exercise to stress reduction and personalized assessments—individuals can significantly reduce their risk of heart disease while enhancing their stamina and overall performance. These strategies reflect a shift away from reactive medicine toward proactive wellness, where prevention is not merely a suggestion but a central tenet of optimal health.
Understanding how disease prevention programs try to reduce cardiovascular disease also highlights the role of community, education, and personalized support in long-term success. Rather than relying solely on pharmacologic solutions, these programs empower individuals to take control of the many modifiable risk factors that influence heart health. From reducing inflammation to optimizing blood flow, the best heart disease interventions are those that align with the body’s natural rhythms and capacities.
Whether you are an athlete striving to extend your endurance or simply someone seeking to protect your heart, integrating these holistic CVD interventions into daily life offers a powerful foundation for lasting wellness. By committing to these natural, scientifically supported practices, you not only safeguard your heart but also unlock your body’s potential for greater energy, resilience, and longevity.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Impact of Lifestyle Modifications on Cardiovascular Health: A Narrative Review
10 Effective Ways to Prevent Heart Disease and Boost Heart Health