Understanding the Challenge of Building Endurance with a Weak Heart
Living with a weak heart doesn’t mean surrendering your health or sidelining your ambitions for an active lifestyle. In fact, medical experts increasingly recognize that strategic endurance training can be safe and highly beneficial for individuals with cardiovascular challenges, provided the approach is carefully tailored. A weak heart may struggle to pump blood efficiently, but structured and medically guided activity can help improve circulation, strengthen the heart muscle, and reduce the risk of heart failure. The key lies in understanding the boundaries of safe exertion and implementing gradual, supportive routines.

While the question “can heart conditions and endurance training safely coexist?” may seem daunting, research shows that with proper supervision and individualized plans, they often can. Heart patients, especially those with mild to moderate impairment, can improve both stamina and quality of life through targeted exercise. This effort, however, requires a deep understanding of the underlying condition, attention to warning signs, and coordination with cardiologists and physical therapists who specialize in cardiovascular rehabilitation. The goal is not to push beyond limits, but rather to intelligently expand them in a way that supports healing and function.
In the case of congestive heart failure and age-related decline, building endurance is not just a luxury but a crucial strategy to maintain independence. Recognizing the early symptoms of heart failure in elderly individuals, such as persistent fatigue, swelling in the lower limbs, and shortness of breath during light exertion, is essential. These symptoms are not signs to give up but rather signals that the body needs structured intervention. Left unaddressed, they can escalate, increasing the overall risk of heart failure. Thus, a proactive approach involving exercise, medical heart monitoring, and lifestyle modification is often recommended.
The reality is that the risk of heart failure increases significantly with age, particularly in those with underlying cardiovascular conditions. For a person with heart dysfunction, even small improvements in circulation and muscular strength can have substantial impacts. Studies suggest that consistent low- to moderate-intensity activity helps to lower blood pressure, improve cholesterol levels, and regulate blood sugar—all of which reduce the risk for CHF. Therefore, endurance training, when combined with weak heart treatment protocols, becomes a pillar of both prevention and therapy.
It is important to dispel the myth that those asking, “Do I have heart disease?” must completely avoid physical strain. While intense, unsupervised workouts are discouraged, intelligently designed movement can serve as a diagnostic and therapeutic tool. Feeling short of breath too soon, for example, may uncover hidden heart disease elderly symptoms, prompting earlier interventions. With proper education, even vulnerable individuals can use endurance training to reclaim strength and vitality.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice
The Science Behind Cardiovascular Training and Heart Function
To understand how endurance training benefits individuals with compromised heart function, it’s helpful to explore the physiological mechanisms involved. A strong heart pumps more blood with each beat, a measurement known as stroke volume. When the heart is weak, this volume decreases, limiting oxygen delivery to muscles and organs. Endurance training, when performed safely, can encourage the heart to adapt over time. These adaptations include improved vascular tone, increased capillary density, and more efficient oxygen use at the cellular level.
Training does not magically fix a weak heart, but it provides a meaningful pathway toward functional improvement. This is particularly relevant in cases involving congestive heart failure risk factors such as hypertension, diabetes, obesity, and a sedentary lifestyle. Addressing these factors through endurance work offers a comprehensive treatment benefit that often exceeds the power of medication alone. Moreover, endurance training helps counteract the deconditioning spiral that often follows diagnosis. As physical strength wanes, activity decreases, which in turn weakens the cardiovascular system further.
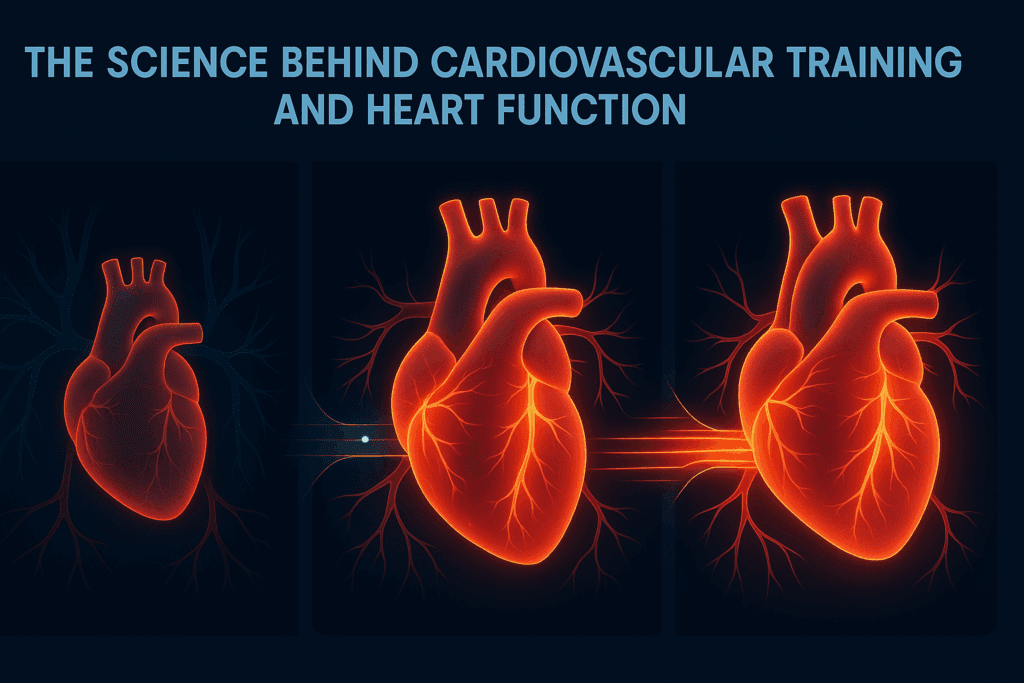
One of the most promising aspects of endurance training for heart patients lies in its anti-inflammatory effects. Chronic inflammation is both a contributor to and a result of cardiovascular disease. Moderate-intensity aerobic exercise has been shown to reduce inflammatory markers in the blood, which helps stabilize blood vessels and support overall heart health. For those at risk for CHF, incorporating regular movement is one of the most evidence-backed interventions available.
Understanding how to fix a weak heart goes beyond surgical interventions or pharmacology. While those treatments play a vital role, they are often more effective when combined with daily habits that support heart function. Endurance exercise stimulates nitric oxide production, which relaxes blood vessels and improves circulation. It also encourages the release of beneficial hormones like endorphins and brain-derived neurotrophic factor (BDNF), which not only elevate mood but also support neurological and cardiovascular resilience.
Finally, training provides a powerful psychological benefit. The emotional burden of being a heart patient can be profound, often marked by fear, anxiety, and a sense of limitation. Regular exercise, even at low intensity, helps rebuild confidence and autonomy. It shifts the narrative from one of illness to one of empowerment. And in this way, the heart effects of endurance training go beyond the physical—they nourish the mind as well.
Tailoring Endurance Training for Individuals at Risk for CHF
When developing an endurance program for someone with a weak heart, customization is everything. No two people experience cardiovascular disease in exactly the same way, and a one-size-fits-all approach can do more harm than good. The first step in tailoring an exercise plan is identifying the individual’s congestive heart failure risk factors. These can include not just physical markers like high blood pressure or abnormal heart rhythms, but also lifestyle habits such as diet, stress management, and sleep quality.
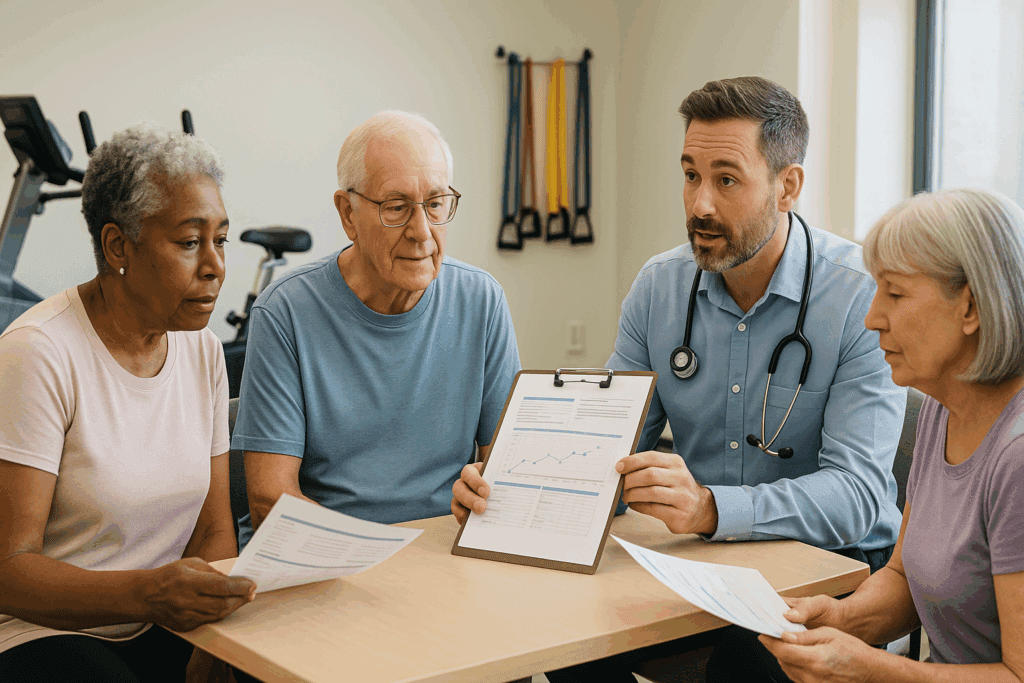
A person with heart disease must begin with a comprehensive medical assessment. This often includes imaging tests, blood work, and an exercise stress test to determine safe exertion levels. Once baseline metrics are established, the individual can begin a supervised program. Cardiac rehabilitation centers provide an ideal setting, as they are staffed by professionals who understand how to adapt routines based on a person’s capacity and progression. From walking programs and resistance band routines to stationary cycling, each component is chosen to minimize strain while maximizing cardiovascular benefit.
It is also crucial to educate patients on how to monitor their responses to training. Warning signs such as unusual fatigue, dizziness, or chest discomfort should never be ignored. Understanding these symptoms allows for early intervention and adjustments to the program. For those managing symptoms of heart failure in elderly populations, involving caregivers or family members in this monitoring process can offer additional safety and support.
Training routines for individuals at risk of heart failure must include both aerobic and strength components, though the balance may differ. Aerobic activities improve endurance and cardiovascular capacity, while resistance work supports muscular strength and metabolism. Both are essential for maintaining functional independence and reducing the burden on the heart. The frequency, intensity, and duration of these sessions should be gradually increased, with regular re-evaluations by healthcare providers.
Incorporating flexibility and balance exercises can further support aging individuals managing heart disease elderly symptoms. Falls and injuries can lead to periods of inactivity, during which deconditioning can occur rapidly. Maintaining a diverse training portfolio helps reduce this risk while offering the psychological benefit of variety and progress. Every element of the plan is chosen not only for its physical benefit but also for its role in sustaining motivation and long-term adherence.
Medical Heart Treatments That Complement Endurance Training
While exercise plays a central role in heart rehabilitation, it must be integrated with appropriate medical treatments to deliver full benefit. Pharmacological therapies such as beta-blockers, ACE inhibitors, and diuretics are commonly prescribed to support heart function and reduce fluid retention. These medications help stabilize the individual so they can tolerate physical training without undue risk. In some cases, devices such as pacemakers or implantable cardioverter defibrillators (ICDs) may be necessary, especially when irregular rhythms pose a threat.
Integrating these medical heart treatments with training requires open communication between the patient and their healthcare team. Adjusting medication timing or dosage may be necessary depending on how the body responds to exercise. For instance, some heart medications can lower blood pressure or heart rate to the point that they affect exercise tolerance. Monitoring these parameters allows clinicians to fine-tune the balance between safety and effectiveness.
Nutritional support is another pillar of a holistic treatment plan. A diet rich in whole grains, lean protein, healthy fats, and abundant vegetables helps regulate blood pressure, cholesterol, and glucose levels. These dietary shifts also support energy production, making endurance training more manageable and effective. Nutrition can also reduce inflammation and improve body composition, directly addressing several congestive heart failure risk factors.
Sleep quality is frequently overlooked but plays a pivotal role in cardiovascular recovery. Individuals with heart disease or symptoms of heart failure in elderly adults often experience disrupted sleep due to discomfort, anxiety, or medication effects. Prioritizing sleep hygiene, possibly with the support of a sleep specialist, can significantly improve heart function and endurance capacity. When combined with exercise, proper sleep becomes a performance enhancer as much as a health essential.
Finally, the role of mental health cannot be understated. Depression and anxiety are common in heart patients and can reduce motivation to engage in exercise or follow treatment plans. Cognitive behavioral therapy (CBT), mindfulness practices, and support groups offer valuable tools to overcome these hurdles. By addressing emotional and psychological needs alongside physical ones, the individual is far more likely to sustain both medical treatments and endurance efforts over the long term.
Frequently Asked Questions: Boosting Endurance with a Weak Heart
1. Can heart patients safely pursue endurance training without increasing health risks? Yes, heart patients can safely pursue endurance training, but the key is individualized planning and professional supervision. While concerns often arise about whether increased activity can cause heart risks, numerous clinical studies confirm that moderate, structured exercise often improves cardiovascular efficiency. For someone managing a weak heart treatment protocol, supervised movement helps reduce sedentary complications like blood clots, muscle loss, and poor circulation. The right training program should include heart rate monitoring, symptom tracking, and clear recovery protocols. Over time, this approach reduces the overall risk of heart failure by improving both physical and emotional resilience.
2. What are lesser-known congestive heart failure risk factors that people often overlook? While high blood pressure and coronary artery disease are well-known, lesser-known congestive heart failure risk factors include sleep apnea, chronic kidney disease, and prolonged stress exposure. These secondary contributors can significantly increase the risk for CHF, especially when combined with poor lifestyle habits. For instance, obstructive sleep apnea causes intermittent drops in oxygen levels, placing pressure on a heart already weakened by other medical conditions. Similarly, undiagnosed insulin resistance or thyroid disorders may quietly undermine heart function. By identifying and treating these hidden factors early, a person with heart concerns can create a more effective prevention plan.
3. How do endurance strategies differ for those seeking weak heart treatment versus general cardiac rehab? For individuals undergoing weak heart treatment, endurance strategies must account for reduced cardiac output and heightened sensitivity to fatigue. Unlike general cardiac rehab, which often assumes stable baseline function, these protocols must prioritize energy conservation and interval pacing. For instance, a heart patient may benefit more from short bouts of walking alternated with rest rather than continuous activity. Additionally, breathwork and posture training can significantly improve oxygenation and reduce cardiovascular strain. Tailoring routines in this way addresses both the physical and psychological demands of endurance-building while reducing the overall risk of heart failure.
4. What are some early psychological signs that may indicate a heart patient is overexerting during training? Increased irritability, anxiety, and emotional withdrawal can all signal overtraining in a heart patient. These psychological responses may appear before physical symptoms like chest tightness or dizziness, offering early clues that the current regimen is too intense. The link between mental fatigue and medical heart health is often underappreciated. Elevated cortisol and disrupted sleep cycles can impair cardiac recovery, even if heart rate and blood pressure appear stable. Recognizing these subtle shifts is critical in minimizing long-term heart effects and ensuring a sustainable training routine.
5. How do symptoms of heart failure in elderly individuals change the way we approach training and monitoring? Symptoms of heart failure in elderly adults often manifest differently than in younger populations. Instead of overt shortness of breath, an older person with heart concerns may simply feel weak, confused, or excessively tired after light activity. These subtler signs demand careful observation, especially when adjusting endurance plans. Seniors with heart disease elderly symptoms should have frequent health check-ins and use tools like step counters or fatigue diaries to document their progress. By tracking these less obvious symptoms, medical teams can prevent small issues from escalating into serious cardiac events.
6. What emerging technologies are helping people reduce the risk for CHF while staying active? Wearable fitness technology has made it easier than ever to reduce the risk for CHF through real-time health feedback. Devices now track metrics beyond heart rate, such as heart rate variability (HRV), blood oxygen saturation, and even early arrhythmia detection. These tools empower a person with heart conditions to make data-driven decisions about training intensity and recovery needs. Additionally, AI-assisted coaching platforms use this data to personalize exercise recommendations and alert users when their metrics deviate from safe ranges. As digital health tools evolve, they offer promising new avenues for improving endurance safely while managing the underlying risk of heart failure.
7. Do I have heart disease if I often feel lightheaded or tired after walking short distances? Frequent lightheadedness or fatigue after mild exertion can be a red flag but doesn’t automatically mean you have heart disease. These symptoms, especially if recurring, warrant a thorough cardiovascular assessment. Asking “Do I have heart disease?” is not about self-diagnosing but about recognizing when the body is sending distress signals. For some, the issue may stem from anemia, medication side effects, or dehydration rather than a medical heart condition. However, because these symptoms also align with congestive heart failure and age-related decline, early evaluation is the best course of action.
8. What long-term lifestyle changes have the biggest impact on how to fix a weak heart naturally? Fixing a weak heart naturally involves consistent habits across physical, mental, and nutritional domains. Beyond exercise, key strategies include prioritizing deep, restorative sleep, managing blood sugar levels through diet, and cultivating supportive social relationships. Nutritionally, potassium-rich foods and anti-inflammatory fats like those in olive oil or flaxseeds can improve vascular function. Psychologically, practices like journaling or group therapy can ease the stress that often worsens cardiac symptoms. These holistic lifestyle changes, when maintained, reduce long-term heart effects and empower heart patients to regain strength without relying solely on medication.
9. How does congestive heart failure and age interact to complicate recovery timelines for endurance training? As people age, muscle mass, hormonal balance, and circulatory efficiency all decline, complicating recovery for those with congestive heart failure and age-related vulnerabilities. Healing and adaptation from exercise take longer in older adults, and this must be factored into any endurance plan. For instance, a younger heart patient may tolerate a four-day-per-week routine, whereas an older person with heart symptoms may need twice the rest and half the volume. In these cases, progress should be measured not in speed but in consistency and function—such as reduced fall risk or the ability to walk longer without stopping. Recognizing these physiological constraints helps reduce frustration and improve adherence.
10. Will heart patients always need supervision when training, or can independence be achieved? While early-stage training for a heart patient should always be supervised, long-term independence is both possible and encouraged. With proper education and tools, a person with heart conditions can transition to self-guided routines that align with their health goals. Regular check-ins with a cardiologist, use of heart rate monitors, and a clear understanding of warning signs are essential to maintaining safety. Moreover, building self-efficacy—through confidence in managing symptoms and making informed choices—directly supports motivation and progress. Ultimately, independence becomes a form of treatment itself, reducing the risk for CHF and enhancing the heart effects of physical conditioning over time.

Conclusion: Building Strength and Stamina with a Compassionate, Science-Backed Approach
Boosting endurance with a weak heart is not only possible—it is often one of the most transformative decisions a person with heart challenges can make. Through the integration of expert-approved weak heart treatment options, individualized endurance training, and a comprehensive lifestyle approach, individuals can meaningfully reduce their risk of heart failure. Rather than focusing on limitations, this strategy highlights possibilities for renewal and resilience.
Understanding how to fix a weak heart doesn’t come from one source alone. It involves synthesizing medical heart care, consistent physical activity, informed nutrition, emotional support, and mindful monitoring of symptoms. Whether managing heart disease elderly symptoms or navigating the complex terrain of congestive heart failure and age-related decline, patients are not powerless. On the contrary, they hold the ability to influence their health outcomes through daily choices, guided by science and compassion.
As more people ask, “Do I have heart disease?” or confront the sobering realization of a diagnosis, the value of education and structured support becomes undeniable. Exercise, when done right, serves not just the body but the spirit—reminding each person with heart disease that their journey toward strength is not defined by weakness, but by the will to rise above it.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
How to Improve Heart Health Naturally?

