For many people, hunger is a predictable and essential part of daily life. It signals the body’s need for nourishment and helps maintain the delicate balance of energy and nutrition. But what happens when that sense of hunger suddenly fades, even when you haven’t eaten all day? Or when the thought of eating causes discomfort or nausea? A sudden or prolonged loss of appetite can be unsettling, especially when paired with other symptoms such as fatigue or digestive discomfort. Understanding what causes no appetite, and recognizing when it’s a sign of something more serious, is key to supporting long-term wellness and nutritional balance.
The phrase “why am I not hungry anymore” is more than just a momentary concern; it reflects an issue that may stem from physical, emotional, or lifestyle-related factors. Whether you’re feeling hungry but no appetite follows, or you’re struggling with a lack of hunger even after long periods without food, these experiences deserve careful attention. This article takes an in-depth look at the potential causes of appetite loss, explores its connection to nausea and fatigue, and offers science-backed strategies to help you support your appetite and overall health.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
Understanding Appetite: How Hunger Works in the Body
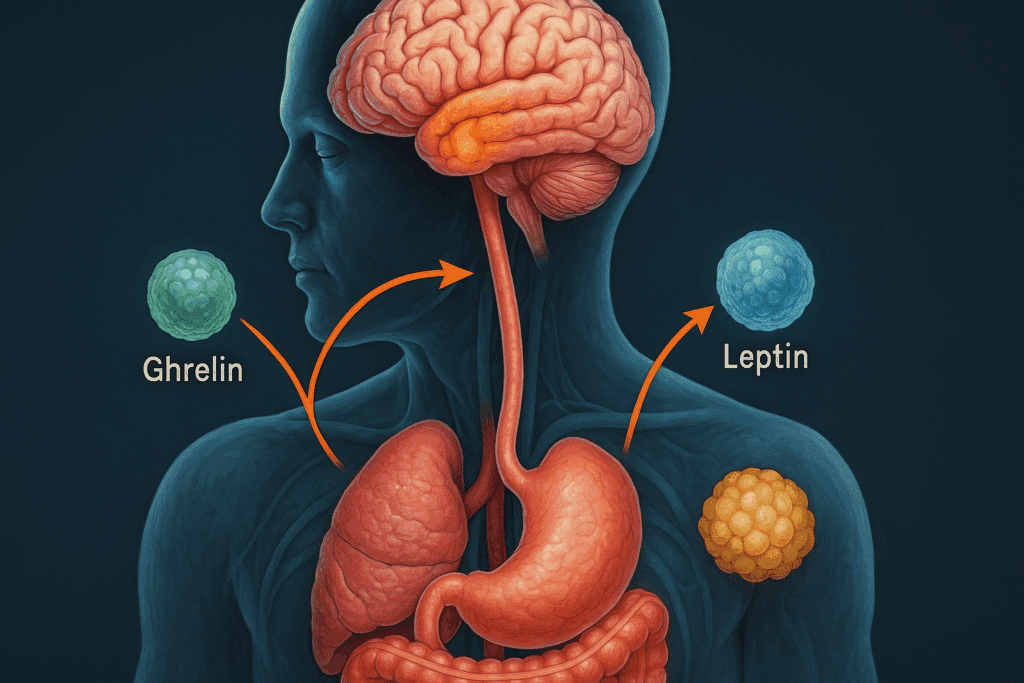
Before delving into the causes of a decreased appetite, it helps to understand how hunger operates in the body. Appetite is not merely about physical need; it’s a complex interaction of hormones, brain signals, digestive cues, emotional states, and external factors like stress or environment. Hormones such as ghrelin and leptin regulate hunger and satiety. Ghrelin, often called the “hunger hormone,” stimulates the appetite, while leptin signals fullness. When these hormones are disrupted, your body may stop giving the usual cues that it’s time to eat.
In addition to hormonal signals, the hypothalamus plays a central role in controlling appetite. It interprets signals from the body and responds accordingly. If something interferes with this communication system—such as illness, medications, or emotional distress—the result can be a sudden loss of appetite. You may find yourself saying, “I need to eat but I have no appetite,” without understanding why. It’s not always a sign of disease, but it does warrant thoughtful investigation.
What Causes No Appetite? Exploring the Most Common Reasons
There are many potential reasons behind a lack of appetite, some temporary and benign, others more serious. Emotional stress is a common trigger. Anxiety, depression, grief, and trauma can all interfere with hunger signals. For many people, mental health challenges result in feeling starving but no appetite persists, particularly during times of acute emotional distress. The brain, preoccupied with other concerns, deprioritizes the urge to eat.
Medical conditions are also important to consider when you ask, “Why do I not have an appetite?” Chronic illnesses such as liver disease, kidney problems, heart failure, and cancer are all associated with appetite changes. Gastrointestinal issues like gastritis, acid reflux, or irritable bowel syndrome can cause nausea and poor appetite. Even short-term infections like the flu or COVID-19 can lead to a noticeable decrease in hunger. For some, the question becomes, “Why have I lost my appetite for days?” when the body is fighting an illness.
Medications are another leading cause of loss of appetite. Many prescription drugs—including antibiotics, antidepressants, chemotherapy agents, and pain medications—list appetite suppression as a side effect. If you’ve noticed a pattern of nausea and lack of appetite after starting a new medication, this connection is worth exploring with your healthcare provider. Addressing the root cause can often restore appetite naturally.
Loss of Appetite and Nausea: Why They Often Occur Together
Experiencing a loss of appetite and nausea together is more common than you might think. This combination can result from digestive disturbances, hormonal imbalances, or neurological factors. For instance, gastrointestinal inflammation can trigger both symptoms, making it uncomfortable to eat and difficult to keep food down. Conditions like gastritis, peptic ulcers, or gastroenteritis frequently present with these issues.
Hormonal fluctuations—such as those that occur during pregnancy, menopause, or thyroid dysfunction—can also interfere with the body’s hunger and digestion signals. Nausea and poor appetite may be your body’s way of coping with these internal changes. Likewise, if you feel “I have no appetite and feel sick when I eat,” it’s important to consider if there is a pattern or correlation to hormonal cycles or stress levels.
Neurological disorders and migraines are less commonly considered but relevant causes of nausea and lack of appetite. In these cases, the brain’s processing of sensory input is affected, which can alter taste perception, cause dizziness, and make food unappealing. The key is to view these symptoms as interconnected, not isolated, and to track them over time for clues to their origin.
Why Am I Not Hungry After Not Eating All Day?
It might seem counterintuitive, but some people report not feeling hungry even after skipping meals. This phenomenon can be frustrating and confusing. One reason this occurs is due to prolonged fasting or irregular eating patterns that disrupt normal hunger cues. When the body goes without food for extended periods, it can enter a state of conservation, reducing the sensation of hunger to prioritize essential functions.
This response may be adaptive in the short term but can lead to long-term issues with metabolism and nutrient intake. If you’re wondering, “Why am I not hungry after not eating all day?” it’s essential to reflect on your eating habits, sleep quality, hydration, and stress levels. Sleep deprivation, dehydration, or chronic stress can dampen the release of ghrelin and other hunger-related hormones, blunting appetite even when caloric needs are high.
Additionally, individuals recovering from illness or experiencing emotional burnout may face a delayed return of appetite. In these cases, the body is still recalibrating, and it may take time to reestablish normal hunger signals. A gentle and consistent routine with small, nutrient-dense meals can help encourage the return of appetite without overwhelming the digestive system.
Loss of Appetite and Fatigue: When to Pay Closer Attention
While occasional loss of appetite may not be cause for concern, a sustained decrease in hunger accompanied by fatigue warrants a more thorough evaluation. Fatigue can stem from nutrient deficiencies, hormonal imbalances, chronic illness, or mental health conditions—all of which can also impact appetite. In this context, the question is not just “why am I not hungry anymore” but also “why am I so tired and unmotivated to eat?”
Vitamin and mineral deficiencies, particularly in B vitamins, iron, and magnesium, can create a cycle of low energy and poor appetite. If the body lacks the nutrients needed for energy production, it may struggle to generate hunger cues. Similarly, thyroid dysfunctions such as hypothyroidism can cause both fatigue and a decrease in appetite. People experiencing this might say, “I’m losing appetite and nausea hits me every time I try to eat.”
In cases where both symptoms persist, it’s crucial to rule out more serious conditions such as anemia, chronic infections, autoimmune diseases, or depression. A comprehensive blood panel and physical exam can help pinpoint the source of the problem. Ignoring ongoing symptoms can delay treatment and allow nutritional imbalances to worsen.

What Are 4 Things That Affect Appetite? Key Influencers You Should Know
When examining appetite fluctuations, it’s helpful to identify the main factors that can affect hunger patterns. Four major elements that influence appetite are psychological health, hormonal regulation, dietary habits, and medication use. Each of these components interacts with the others, creating a dynamic system that governs when and how we feel hungry.
Psychological factors play a prominent role. Stress, anxiety, grief, and depression can significantly suppress appetite by interfering with neurotransmitter balance. Individuals experiencing emotional strain often report a lack of appetite and describe meals as unappealing or overwhelming. In this context, asking “why do I have a loss of appetite” leads to deeper mental health conversations that are vital to overall well-being.
Hormones are another key player. Beyond ghrelin and leptin, hormones like cortisol (stress), insulin (blood sugar regulation), and serotonin (mood) all contribute to hunger signals. Disruptions to these hormones—due to sleep disorders, endocrine conditions, or erratic eating schedules—can easily cause a sudden loss of appetite.
Dietary patterns also matter. Highly processed foods, excessive caffeine, or irregular eating schedules can blunt hunger cues. Skipping meals or fasting inconsistently may cause your body to ignore natural hunger signals over time. Finally, medications—both over-the-counter and prescription—can dull hunger, increase nausea, or alter taste perception, all of which contribute to appetite suppression.
Why Is It Hard to Have an Appetite? The Psychological Dimension
For many individuals, eating is not just a biological function but an emotional and psychological experience. Trauma, chronic stress, eating disorders, or adverse childhood experiences can all condition the brain to disassociate from hunger cues. When the brain is wired to avoid food as a coping mechanism, even physical hunger may be misinterpreted or ignored.
This disconnection often becomes a learned behavior, reinforced over time by anxiety or discomfort surrounding food. People who say, “Why is it hard to have an appetite?” may be dealing with deeply ingrained behavioral patterns. For example, individuals with a history of restrictive dieting or body image issues may find themselves hungry but no appetite arises due to internalized guilt or fear.
Restoring appetite in these cases requires a compassionate, therapeutic approach. Working with a licensed therapist, registered dietitian, or counselor trained in disordered eating can help address the root causes of food aversion. Techniques such as mindful eating, intuitive eating practices, and somatic therapy can help rebuild a healthier relationship with food and bodily cues.
Starving but No Appetite: A Paradox Worth Exploring
One of the most confusing and distressing experiences related to appetite is the feeling of being physically starved yet having no desire to eat. This paradox often stems from a disconnect between the body’s physiological needs and the brain’s emotional or sensory processing of hunger. People in this state may say, “I’m starving but no appetite kicks in,” reflecting the tension between bodily deprivation and psychological inhibition.
This condition can emerge in response to chronic stress or trauma, during which the sympathetic nervous system suppresses digestive function. When stress hormones are elevated, the body enters a state of fight-or-flight, diverting energy away from non-essential processes like digestion. As a result, the stomach may feel empty, yet the brain fails to trigger an appropriate hunger response.
In other cases, inflammation of the digestive tract can send confusing signals to the brain, creating the sensation of emptiness without the corresponding appetite. This is commonly seen in individuals with gastrointestinal disorders or food intolerances. Addressing these underlying issues—whether physiological or psychological—is key to resolving the dissonance and restoring normal hunger patterns.
What Does Loss of Appetite Mean for Long-Term Health?
Prolonged appetite suppression can have serious implications for long-term health. Nutrient deficiencies, muscle wasting, weakened immunity, and hormonal imbalances are all potential consequences of sustained caloric deprivation. If someone regularly feels, “I need to eat but I have no appetite,” their body may be struggling to meet even basic energy requirements.
Appetite is a fundamental biological drive designed to protect the body from starvation and support optimal function. Disruptions to this system can weaken nearly every physiological process, from bone health to cardiovascular function. Over time, even a mild but persistent decrease in food intake can lead to unintentional weight loss, reduced concentration, and mood instability.
Maintaining appetite is particularly important for populations at risk, such as older adults, individuals with chronic illness, or those recovering from surgery. In these groups, even temporary loss of appetite and fatigue can delay recovery, increase the risk of complications, and reduce quality of life. Early intervention and supportive care can prevent long-term health decline.
Supporting a Healthy Appetite: Practical and Evidence-Based Strategies
If you find yourself wondering, “Why have I lost my appetite?” and want to restore healthy eating habits, the first step is to identify and address the root cause. A comprehensive approach includes nutritional support, emotional care, and lifestyle adjustments. Eating small, frequent meals that are nutrient-dense but not overwhelming can stimulate appetite gently and sustainably.
Incorporating foods rich in zinc and B vitamins—both of which support appetite regulation—may help improve hunger over time. Aromatic herbs like ginger, mint, and fennel can ease digestion and reduce nausea. Hydration is also key; dehydration can mask as fullness or reduce hunger cues. Warm broths, herbal teas, and electrolyte solutions can support hydration without causing discomfort.
For those dealing with no appetite and nausea, avoiding overly spicy or greasy foods and opting for bland, easily digestible meals can provide nourishment without irritation. Stress management techniques—such as yoga, deep breathing, or nature walks—can shift the body out of fight-or-flight mode and restore parasympathetic (rest-and-digest) function, encouraging hunger.
Frequently Asked Questions (FAQ): Understanding Sudden Loss of Appetite, Nausea, and What It Means for Your Health
1. Can environmental factors contribute to a sudden loss of appetite, even if I’m not sick? Yes, environmental and seasonal changes can significantly impact appetite without indicating illness. For example, hot weather can reduce the body’s need for calories and may lead to a loss of appetite, especially when paired with dehydration. Air pollution, disrupted circadian rhythms, or a lack of exposure to natural sunlight can also influence mood and appetite-regulating hormones like serotonin and leptin. People often wonder, “Why do I not have an appetite when the weather changes?” This can be due to your body adapting to its environment in ways that temporarily suppress hunger signals. Understanding these nuanced loss of appetite causes helps differentiate between serious medical conditions and situational fluctuations.
2. Why do I feel full so quickly even when I haven’t eaten much? Feeling full after eating only a small amount can be frustrating, especially when paired with a lack of hunger throughout the day. This sensation may stem from delayed gastric emptying, a condition where the stomach digests food more slowly than normal. In these cases, someone may say, “I am starving but no appetite appears once I start eating.” It can also occur with certain stress-related disorders or autonomic nervous system imbalances, where digestion is slowed due to chronic fight-or-flight activation. If you’re experiencing this consistently and asking yourself, “Why am I not hungry after eating so little?” it may be time to evaluate gut motility and consult a specialist.
3. How do hormonal changes during perimenopause or menopause affect appetite and nausea? Fluctuating estrogen and progesterone levels can disrupt hunger and fullness signals, making appetite unpredictable. Some individuals experience nausea and poor appetite during hormonal transitions, leading to meals being skipped unintentionally. As hormones shift, it’s common to wonder, “Why have I lost my appetite for days without explanation?” In perimenopause, a heightened stress response and declining serotonin levels can trigger both digestive changes and mood swings, contributing to loss of appetite and fatigue. This isn’t just about aging—it’s about recalibrating the body during a time of hormonal upheaval.
4. Why do I have a loss of appetite when I’m under pressure, even though I logically know I need to eat? When under chronic pressure or stress, the brain prioritizes alertness and survival over digestion. The sympathetic nervous system suppresses hunger, often leaving you thinking, “I need to eat but I have no appetite and don’t know why.” This biological adaptation can become problematic when prolonged, as it leads to undernutrition and potential health issues. In high-achieving environments, this pattern can go unnoticed because individuals are focused on productivity rather than self-care. Understanding what causes no appetite under stress can help you introduce calming rituals, such as breathwork or grounding exercises, that re-activate digestion.
5. Is loss of appetite and nausea common after intense physical activity or athletic training? Yes, especially after endurance training, people often feel nauseated and report a lack of appetite despite having exerted significant energy. This is due to blood being diverted away from the stomach to support muscle function, causing temporary digestive suppression. You might notice you’re hungry but no appetite remains once the workout is over, especially if hydration was insufficient. Additionally, cortisol released during strenuous exercise can cause loss of appetite and nausea, particularly in individuals new to training regimens. It’s important to prioritize post-workout recovery with fluids and small, easily digestible meals to rebuild both appetite and energy.
6. Could social or cultural factors influence why I’m losing my appetite? Absolutely. Cultural perceptions of body image, meal timing norms, and emotional relationships with food can all impact appetite. In some cultures, eating in public or eating alone may trigger discomfort, which can be misinterpreted as loss of appetite. People sometimes find themselves asking, “Why is it hard to have an appetite around others or in certain settings?” These responses are often rooted in learned behaviors, self-consciousness, or performance-related stress. Exploring the psychological and sociocultural layers of why appetite changes in different environments can offer insight into how deeply interconnected eating patterns are with identity and belonging.
7. What can cause loss of appetite in older adults who seem otherwise healthy? In aging populations, sensory decline—especially changes in taste and smell—can significantly reduce the enjoyment of food, leading to gradual loss of appetite and fatigue. Additionally, medications often increase with age, and drug interactions can dull hunger or cause nausea and lack of appetite. If an older adult says, “I have no appetite and feel sick when I eat,” consider not just physical conditions but also loneliness, grief, or undiagnosed depression as possible contributors. Nutritional needs change with age, and appetite signals may weaken even when energy requirements stay the same. Understanding what are the causes of losing appetite in later life is crucial for proactive care and nutrition planning.
8. How does loss of appetite relate to gut-brain axis dysfunction and mental health? The gut-brain axis is a bidirectional communication system that significantly affects hunger, mood, and digestion. When disrupted by inflammation, microbial imbalance, or psychological stress, it can lead to nausea and poor appetite or even a sudden loss of appetite. People with anxiety, depression, or PTSD frequently report appetite changes, leading to questions like, “Why do I have a loss of appetite when nothing seems physically wrong?” These changes often originate in the microbiome and the vagus nerve’s altered signaling. Supporting gut health through probiotics, prebiotics, and mind-body therapies can help restore both mood and appetite over time.
9. Is it possible to retrain the body’s hunger signals after a period of low appetite? Yes, and it often starts with consistent, gentle eating habits rather than forcing large meals. After periods where someone might say, “Why am I not hungry after not eating all day?” the body can become desensitized to normal hunger cues. Meal timing, portion control, and sensory stimulation (such as the smell and appearance of food) play an essential role in reawakening appetite. Gradually reintroducing regular eating schedules, even with small snacks, can normalize hormonal signaling. It’s important to approach this process with patience, especially in cases involving loss of appetite and nausea or recovering from illness.
10. How do I know when loss of appetite is serious enough to seek medical help? If you’ve asked yourself, “Why am I not hungry anymore?” for more than a week without improvement—especially if it’s accompanied by weight loss, nausea, dizziness, or fatigue—it’s time to consult a healthcare provider. While some causes are temporary or psychological, others may indicate underlying medical conditions that require intervention. Chronic loss of appetite and fatigue could point to thyroid dysfunction, gastrointestinal disease, or even neurological conditions. It’s also concerning if someone experiences recurring nausea and lack of appetite without explanation, as this may suggest malabsorption or hormonal disorders. Early evaluation ensures timely diagnosis and treatment, preventing long-term health deterioration.
Conclusion: Listening to Your Body When You Ask, “Why Am I Not Hungry Anymore?”
Experiencing a sudden or prolonged loss of appetite is not something to ignore. Whether you’re feeling no appetite and nausea, asking why you’re not hungry after eating so little, or struggling with a general lack of hunger, these are important messages from your body that deserve thoughtful attention. Appetite is a vital component of well-being, and disruptions can have wide-reaching effects on your health, energy, and emotional balance.
Understanding the causes—whether hormonal, emotional, digestive, or neurological—can empower you to take meaningful steps toward recovery. If you’ve been wondering, “Why am I not hungry after not eating all day?” or “Why has my appetite decreased?” the answer may lie in the intricate interplay of lifestyle, health conditions, and mental well-being. Paying attention to your symptoms, seeking professional support, and implementing gentle, sustainable changes can help restore your appetite and, with it, your vitality.
Trusting your body means listening to its cues, even when they change. A loss of appetite may be your body’s way of asking for help—not just nutritionally, but holistically. When you honor those signals with curiosity and care, you begin the journey back to balance, nourishment, and wellness.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.

