Introduction: Rethinking Heart Disease and Age
For years, cardiovascular disease was viewed as a condition reserved for the middle-aged and elderly. But in recent years, medical evidence has begun to rewrite that narrative. Heart problems in 20s and early 30s are no longer rare exceptions—they’re becoming an unsettling trend. With modern lifestyles that often include poor diets, high stress, inadequate sleep, and sedentary routines, younger adults are now facing risks traditionally associated with much older populations.
Questions like “can you get heart disease in your 20s?” become more relevant, it’s clear that younger generations must adopt a more proactive approach to heart health. This article explores the causes, symptoms, and risk factors behind this shift, while offering practical, natural strategies to protect cardiovascular health early in life—especially for those pursuing performance and endurance goals.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice

Why Younger Adults Are Now at Risk for Cardiovascular Disease
The rise in heart disease in 30s and 20s isn’t coincidental. It reflects significant lifestyle shifts over the past few decades. Processed food consumption, reduced physical activity, chronic sleep deprivation, and elevated stress levels all contribute to this growing problem. In particular, young adults face unique health challenges brought on by technology-driven sedentary behavior and the psychological toll of modern work and social pressures.
Research has confirmed that risk factors like obesity, high blood pressure, insulin resistance, and elevated cholesterol are appearing much earlier in life. This has led many health professionals to warn that heart problems in 20s are no longer anomalies, but part of a wider public health pattern. When these risk factors are left unchecked, they set the stage for a lifetime of cardiovascular complications.
The Silent Threat: Why Early Symptoms Often Go Ignored
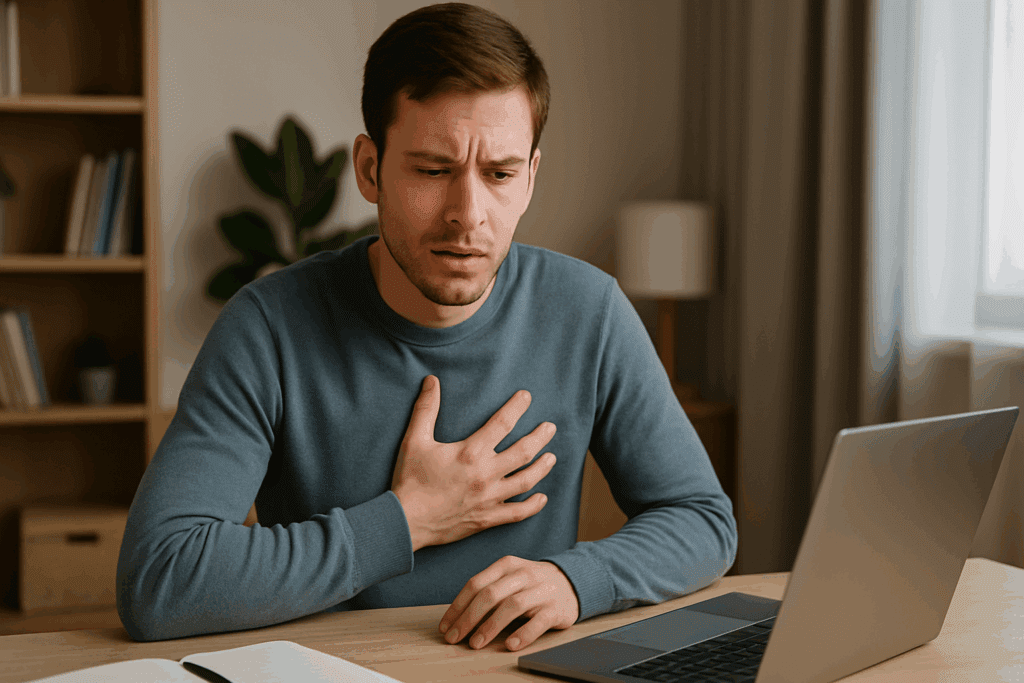
One of the greatest dangers of heart disease in 30s is how easy it is to miss the early warning signs. Young adults rarely associate symptoms like fatigue, mild chest discomfort, or shortness of breath with something as serious as cardiovascular disease. Instead, they often attribute these signs to stress, anxiety, or overexertion at the gym.
Unfortunately, these assumptions can delay diagnosis and treatment. The subtle nature of early heart disease allows it to progress unnoticed until a more serious event occurs, such as a heart attack. Awareness is key: recurring palpitations, unexplained dizziness, and persistent exhaustion deserve medical attention—regardless of age. Proactive evaluation can make a life-saving difference.
Can You Get Heart Disease in Your 20s? The Surprising Reality
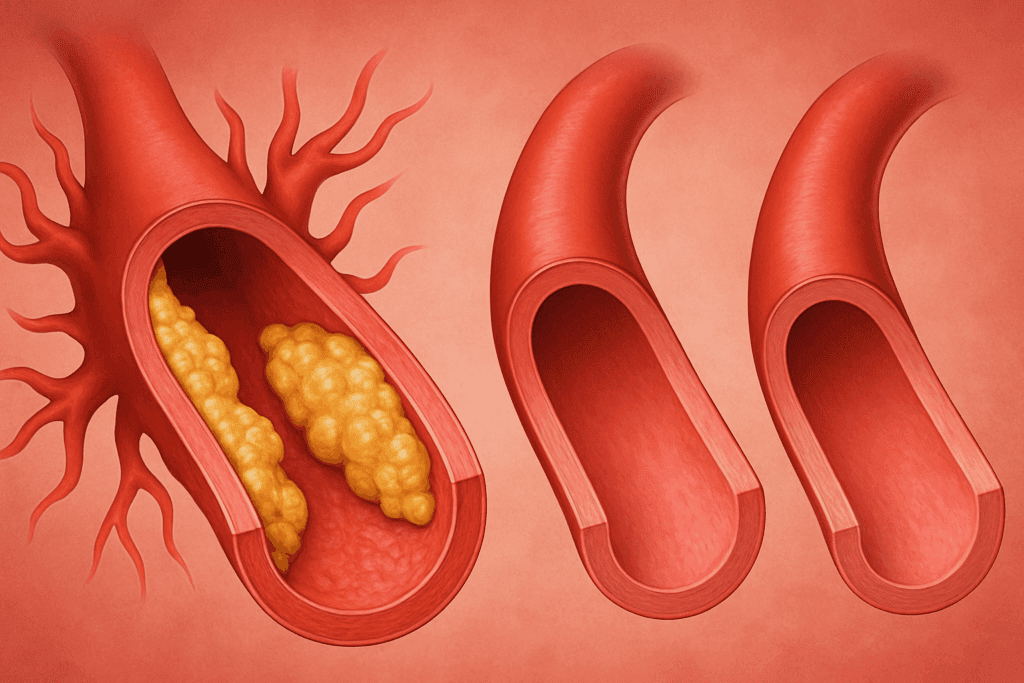
The notion that youth equals immunity from cardiovascular disease is outdated and dangerous. Can you get heart disease in your 20s? Yes, and it’s happening more frequently than ever. Clinical studies and autopsy reports have found signs of early atherosclerosis and arterial plaque buildup in young adults, even those with no obvious symptoms.
This finding shifts the emphasis toward early detection and prevention. Just because symptoms aren’t present doesn’t mean the condition isn’t developing beneath the surface. From poor dietary choices to lack of sleep and chronic stress, young adults are exposed to multiple cardiovascular stressors that, when compounded over time, lead to early damage of the arteries and heart muscle.
How Stress, Mental Health, and Overtraining Affect the Heart
Modern stress isn’t just a psychological burden—it’s a physiological one that can wreak havoc on cardiovascular health. Young adults today are navigating competitive work environments, financial strain, and a constant influx of digital stimulation. These chronic stressors trigger hormonal responses that elevate heart rate, raise blood pressure, and increase inflammation.
For those in the world of endurance and performance enhancement, overtraining adds another layer of risk. Excessive high-intensity workouts without sufficient recovery can actually increase the likelihood of arrhythmias and other heart issues. The body needs balance, and the heart is no exception. Supporting mental and emotional well-being is just as important as physical training when it comes to long-term cardiac resilience.
The Role of Chronic Inflammation and Lifestyle in Young Adult Heart Disease
Chronic inflammation plays a significant role in the development of cardiovascular disease. Poor diets, lack of sleep, and long-term exposure to stress can cause systemic inflammation that gradually damages the inner walls of arteries. Over time, this leads to the accumulation of plaque and a higher risk for heart attacks or strokes—even in individuals under 30.
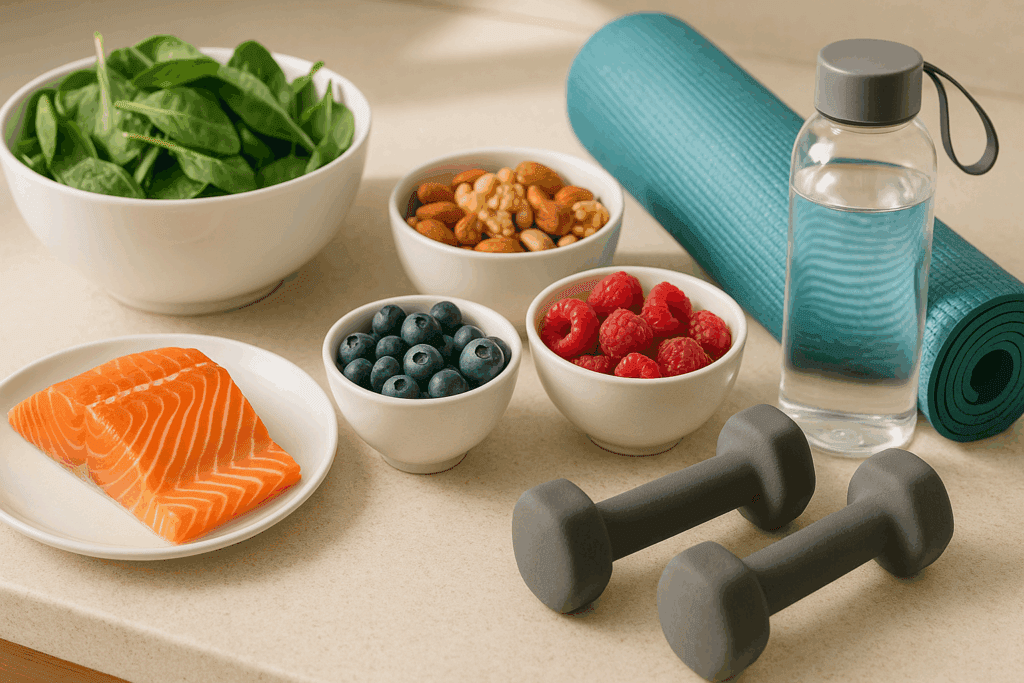
Elevated inflammatory markers, such as C-reactive protein (CRP), are increasingly being detected in people in their 20s and 30s. These findings highlight the importance of early lifestyle interventions. Diets rich in anti-inflammatory foods—like leafy greens, berries, nuts, and omega-3-rich fish—can significantly lower the risk of heart problems in 20s and beyond.
Performance Culture and the Hidden Cardiovascular Costs
The pursuit of peak performance often comes with cardiovascular compromises, especially when fitness is taken to extremes. Young men and women involved in high-level athletic training or bodybuilding may unknowingly put their hearts at risk through overexertion or the use of unregulated performance-enhancing supplements.
Many such substances increase heart rate, blood pressure, and even cholesterol, especially when taken without medical supervision. Combined with intense physical stress and inadequate rest, these habits accelerate cardiovascular aging. That’s why even high-performing athletes are not immune to heart disease in 30s—and why smart performance strategies should prioritize heart-safe protocols.
Creating a Heart-Healthy Routine for Young Adults
Establishing heart-conscious habits early in life can be transformative. A combination of regular moderate exercise, high-quality sleep, stress reduction practices, and balanced nutrition forms the foundation of cardiovascular wellness. Contrary to popular belief, more isn’t always better—especially in training.
Recovery time, hydration, and adequate nutrient intake are critical. A Mediterranean-style diet, for instance, emphasizes whole grains, fresh vegetables, healthy fats, and lean proteins—all shown to reduce heart disease risk. Fitness enthusiasts should also incorporate low-impact activities like yoga or swimming into their routines to give the heart a chance to recover while maintaining endurance.
The Link Between Sleep and Cardiovascular Health
Sleep is often the most overlooked pillar of heart health. Inconsistent or insufficient sleep raises blood pressure, increases insulin resistance, and triggers hormonal imbalances that strain the heart. Unfortunately, many young adults sacrifice sleep to meet work deadlines, social obligations, or screen time habits—often unaware of the cardiovascular toll.
Sleep deprivation disrupts circadian rhythms, which can weaken heart rate variability and reduce parasympathetic recovery. For those seeking endurance and performance gains, proper sleep hygiene is essential. Consistent bedtimes, reduced caffeine intake, and limiting screens before bed can significantly lower the risk of heart problems in 20s and help maintain long-term vitality.
Why Earlier Cardiovascular Screenings Matter
Given the increase in heart disease in 30s, health professionals are now calling for routine screenings to begin earlier—especially for at-risk individuals. Traditional guidelines often suggested waiting until age 40 or older, but emerging evidence suggests that waiting may cost valuable time in prevention.
Screenings such as lipid panels, blood pressure checks, glucose testing, and even echocardiograms for those with symptoms or family history can offer crucial early insight. Young adults, especially those with risk factors like obesity, smoking, or family history of heart disease, should speak with their healthcare provider about early testing. Knowledge gained early empowers timely lifestyle changes and medical interventions.
Future Trends in Cardiovascular Research for Young Adults
As our understanding of early-onset cardiovascular disease evolves, so too does our ability to prevent and treat it. Advances in wearable health tech, including continuous heart rate and oxygen monitors, are giving users unprecedented visibility into their own cardiovascular trends. AI-driven diagnostics are also being used to predict heart disease risk with higher precision, even in asymptomatic individuals.
Clinical research now includes younger adults in trials for cholesterol-lowering therapies and early intervention medications. This growing body of evidence will help refine guidelines and personalize care. Meanwhile, health campaigns and media influencers are helping spread awareness that getting heart disease in your 20s is not just a rhetorical question—it’s a public health wake-up call.
Frequently Asked Questions: Early-Onset Heart Disease in Your 20s and 30s
1. Why are heart problems in your 20s becoming more common now than in previous generations?
Several factors have converged to increase the likelihood of heart problems in 20s today. One of the most critical is the rise of metabolic syndrome among younger populations, driven by poor diets high in refined sugars and trans fats. Additionally, the shift toward sedentary jobs, reduced physical activity, and increased screen time have all contributed to earlier cardiovascular strain. Environmental stressors, such as financial pressures, digital burnout, and social isolation, have intensified sympathetic nervous system activity and chronic inflammation. These modern lifestyle changes explain why we’re now seeing more heart problems in our 20s than ever before.
2. Can you get heart disease in your 20s even if you don’t have a family history of it?
Yes, you can get heart disease in your 20s even in the absence of genetic predisposition. While hereditary factors do play a role, environmental and behavioral factors are proving equally influential. The overconsumption of processed foods, exposure to chronic psychological stress, and sleep deprivation can accelerate endothelial dysfunction regardless of family history. New research shows that even without inherited risk, consistent exposure to high blood pressure or poor glycemic control can result in early plaque formation. Therefore, individuals without family history must still be proactive in protecting cardiovascular health.
3. How does vaping compare to smoking in terms of heart disease risk in young adults?
Although vaping is often marketed as a safer alternative to traditional cigarettes, it still poses significant cardiovascular risks, especially for young adults. Nicotine in both products can raise blood pressure and heart rate, increasing the risk of arrhythmias and arterial damage. Preliminary studies suggest that the flavoring agents and aerosolized chemicals in e-cigarettes may also contribute to oxidative stress in the vascular system. When used regularly, vaping has been linked to increased inflammation and endothelial dysfunction, both of which are precursors to heart disease in the 30s. The perception of safety may lead younger users to underestimate its potential for harm.
4. What role does gut health play in early heart disease development?
Emerging evidence points to a powerful link between gut microbiome health and cardiovascular outcomes. Imbalances in gut bacteria can produce metabolites such as trimethylamine N-oxide (TMAO), which promote atherosclerosis. This pathway is especially relevant for those experiencing heart problems in their 20s, as microbiome imbalances can occur early due to antibiotic overuse, poor diet, or lack of fiber. Strengthening the gut through prebiotic-rich foods, fermented products, and diverse plant-based meals can reduce systemic inflammation. For young adults, maintaining gut health is an underappreciated but vital part of cardiovascular prevention.
5. Can mental health conditions contribute to heart disease in 30s, even in otherwise healthy people?
Absolutely. Psychological disorders such as anxiety and depression can significantly increase cardiovascular risk, even in people with no other medical conditions. These disorders are associated with increased cortisol production, elevated blood pressure, and poor health behaviors like overeating or inactivity. Chronic stress also impairs autonomic nervous system balance, increasing the likelihood of arrhythmias and heart palpitations. For individuals in their 30s, untreated mental health conditions can quietly contribute to heart disease in their 30s without overt warning signs. Integrating mental health care into general wellness routines is crucial for long-term cardiovascular health.
6. How does long-term sleep disruption impact young adult heart health?
Sleep disruption interferes with essential cardiovascular repair processes, particularly during deep, restorative sleep cycles. Young adults who regularly sleep fewer than six hours per night or experience poor-quality sleep are more likely to have elevated resting heart rates, impaired glucose tolerance, and elevated stress hormone levels. These factors can all accelerate vascular aging and increase the risk of developing heart disease in the 30s. Circadian rhythm misalignment, such as that caused by night shifts or irregular sleep schedules, also increases cardiac strain. Prioritizing sleep consistency is a highly underrated preventive strategy.
7. Are there any early fitness signs that could signal undetected heart issues in young adults?
Yes, certain fitness-related symptoms could suggest underlying cardiovascular problems in otherwise active individuals. These include exercise intolerance (reduced stamina or breathlessness), unexplained rapid heart rate during moderate activity, dizziness after standing, or delayed heart rate recovery post-exercise. Even those in peak physical condition can exhibit early signs of heart problems in 20s if they are overtraining, not recovering adequately, or relying on stimulants. Monitoring these subtle performance shifts can prompt timely cardiac evaluation before more serious symptoms emerge.
8. How do hormonal changes or birth control affect heart disease risk in women under 35?
Hormonal contraceptives can elevate the risk of thrombosis, especially in women who smoke, are overweight, or have underlying metabolic conditions. Estrogen-containing birth control can slightly increase blood clotting factors, which—when combined with other risks—may contribute to heart disease in 30s. Additionally, conditions such as polycystic ovary syndrome (PCOS) can lead to insulin resistance and elevated cholesterol, compounding cardiovascular vulnerability. While most young women tolerate contraceptives well, it’s important for healthcare providers to evaluate personal and family history before prescribing. Women should also monitor blood pressure and lipid levels regularly if using hormonal birth control.
9. Can heart disease in the 30s manifest differently than in older adults?
Yes, heart disease in the 30s can often present atypically, making early diagnosis more challenging. Younger adults are more likely to experience symptoms such as fatigue, back pain, or jaw discomfort rather than classic chest pain. They may also present with palpitations, nausea, or anxiety-like symptoms, which can be misdiagnosed as panic attacks or stress. The subtler presentation often leads to delays in treatment, exacerbating long-term damage. For this reason, young adults must advocate for thorough evaluation when symptoms persist or feel unusual.
10. What innovations are helping detect heart problems in younger populations?
Wearable technology is revolutionizing early cardiovascular monitoring. Devices that track heart rate variability, oxygen saturation, and even ECG patterns are now widely available and increasingly accurate. These tools can help detect arrhythmias or subtle changes in autonomic balance before clinical symptoms appear. Mobile health apps are also leveraging machine learning to assess user data and predict cardiovascular risk, especially valuable for detecting heart problems in 20s. These advances enable young people to take control of their heart health proactively, often before standard medical screenings would flag an issue.
Conclusion: Protecting Your Heart Early Is a Game-Changer
The idea that heart problems in 20s or heart disease in 30s are rare is no longer accurate. The reality is that early cardiovascular challenges are becoming increasingly common—but also increasingly preventable. The knowledge that you can get heart disease in your 20s should not inspire fear, but rather action. Through informed choices, regular screenings, and balanced performance routines, young adults can take control of their heart health now and prevent more serious issues later in life.
This shift in awareness marks a new era in wellness—one where prevention is prioritized and age is no longer the sole determinant of risk. For anyone aiming to maximize their performance, stamina, and quality of life, the message is clear: protect your heart early, and it will serve you well for decades to come.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Prevent Heart Disease in Your 20s And 30s

