Understanding Malabsorption: The Silent Disruptor of Health
Malabsorption is a complex yet often overlooked condition that interferes with the body’s ability to absorb essential nutrients from food. It can lead to a wide range of health issues, including weight loss, fatigue, and nutrient deficiencies that may have long-term consequences. Understanding what causes malabsorption, its symptoms, and available treatments is crucial for maintaining optimal digestive health. While many people suffer from malabsorption syndrome without realizing it, identifying the signs early can pave the way for effective intervention.
You may also like: How to Improve Nutrient Absorption: Unlock the Benefits of Bioavailable Nutrients for Holistic Wellness
The human digestive system is designed to break down food and extract nutrients efficiently. However, various factors—including medical conditions, gut imbalances, and dietary choices—can disrupt this process. Whether it’s fat malabsorption symptoms caused by gallbladder dysfunction or the inability to absorb adequate amounts of nutrients due to celiac disease, pinpointing the underlying cause is essential. In this in-depth exploration, we will discuss what causes malabsorption, how to recognize its symptoms, and the most effective natural solutions to restore digestive harmony.
The Mechanisms Behind Malabsorption
To fully understand malabsorption, it’s important to delve into how nutrient absorption occurs. When food enters the digestive tract, enzymes and bile break it down into absorbable components. The small intestine, lined with villi—tiny, finger-like projections—absorbs these nutrients and transfers them into the bloodstream. Any disruption in this process can lead to malabsorption diseases, ranging from mild deficiencies to severe health complications.
Several factors can contribute to malabsorption syndrome. Damage to the intestinal lining, as seen in celiac disease, can hinder nutrient uptake. Pancreatic insufficiency, a condition where the pancreas does not produce enough digestive enzymes, may result in fat malabsorption. Additionally, bacterial overgrowth in the gut can interfere with food absorption—how to tell if you are affected often depends on identifying key symptoms. Understanding these mechanisms allows for targeted approaches to treating malabsorption disorder.
Common Causes of Malabsorption in Adults
Malabsorption can arise from a variety of medical conditions, dietary imbalances, and lifestyle factors. Some of the most common causes include:
- Celiac Disease: An autoimmune condition triggered by gluten consumption, celiac disease leads to inflammation and damage in the small intestine. This can severely impact nutrient absorption, often causing weight loss and malabsorption poop that appears pale, greasy, and foul-smelling.
- Lactose Intolerance: The inability to digest lactose, a sugar found in dairy, leads to bloating, diarrhea, and poor absorption of nutrients.
- Pancreatic Disorders: Conditions such as chronic pancreatitis and cystic fibrosis impair enzyme production, leading to fat malabsorption symptoms such as oily stools and vitamin deficiencies.
- Bacterial Overgrowth: Small intestinal bacterial overgrowth (SIBO) disrupts nutrient absorption by causing excessive fermentation and inflammation.
- Intestinal Surgery: Surgeries such as gastric bypass can shorten the digestive tract, reducing the body’s ability to absorb essential vitamins and minerals.
- Parasitic Infections: Intestinal parasites can damage the gut lining, leading to poor absorption of key nutrients.
Each of these conditions disrupts normal digestion in unique ways, highlighting the need for individualized malabsorption treatments.
Recognizing Malabsorption Syndrome Symptoms
Identifying malabsorption symptoms is essential for early intervention. While symptoms vary depending on the underlying cause, some of the most common signs include:
- Chronic Diarrhea: Loose, watery stools that persist over time may indicate issues with fat absorption or carbohydrate malabsorption.
- Unexplained Weight Loss: The inability to absorb calories and nutrients can lead to significant weight loss despite adequate food intake.
- Fatigue and Weakness: Malabsorption of iron, B vitamins, and other essential nutrients often results in chronic fatigue and weakness.
- Bloating and Gas: Poorly absorbed carbohydrates and proteins can ferment in the gut, leading to excessive bloating and discomfort.
- Malabsorption Poop Look Like: Stools may appear pale, bulky, and oily due to fat malabsorption, often floating in the toilet due to excess fat content.
- Nutrient Deficiencies: Symptoms such as anemia (iron deficiency), brittle nails (calcium deficiency), and muscle cramps (magnesium deficiency) can indicate poor nutrient absorption.
These signs of malabsorption often overlap with other gastrointestinal disorders, making proper diagnosis essential.
Diagnostic Tests for Malabsorption Syndrome
Accurately diagnosing malabsorption syndrome requires a combination of clinical evaluation and laboratory tests. Physicians typically begin with a detailed medical history and physical examination before recommending further diagnostic procedures. Some of the most effective tests include:
- Stool Analysis: Examining stool samples can reveal undigested fat, indicating fat malabsorption syndrome.
- Blood Tests: Measuring nutrient levels, including vitamins and minerals, helps identify deficiencies caused by malabsorption disorder.
- Breath Tests: Used to diagnose lactose intolerance and SIBO by detecting gases produced during fermentation.
- Endoscopy and Biopsy: Direct examination of the small intestine can reveal damage caused by conditions like celiac disease.
- Pancreatic Function Tests: Assessing enzyme output can help determine if pancreatic insufficiency is contributing to malabsorption syndrome symptoms.
Early detection through these tests allows for timely interventions that can prevent complications and improve overall digestive health.
How to Treat Malabsorption and Restore Gut Health
Managing malabsorption syndrome involves addressing the underlying cause while supporting the digestive system. A multi-faceted approach that includes dietary modifications, supplementation, and holistic interventions can significantly improve food absorption. How to tell if treatment is working depends on monitoring symptoms and nutrient levels.
- Dietary Changes: Removing trigger foods (such as gluten for celiac disease) and incorporating nutrient-dense, easily digestible foods can help manage malabsorption.
- Digestive Enzymes: Supplementing with pancreatic enzymes can aid digestion for those with enzyme deficiencies.
- Probiotics and Prebiotics: Restoring a healthy gut microbiome through probiotics can improve digestion and reduce bacterial overgrowth.
- Vitamin and Mineral Supplementation: Addressing deficiencies with targeted supplements ensures adequate nutrient intake.
- Medications for Fat Malabsorption: In some cases, prescription medications such as bile acid sequestrants may be required.
By implementing these strategies, individuals can effectively manage malabsorption and regain digestive balance.
Can Malabsorption Be Cured?
The question of whether malabsorption can be cured depends on its underlying cause. While some conditions, such as lactose intolerance, can be managed with dietary changes, others, like celiac disease, require lifelong adjustments. The goal of treatment is to manage malabsorption syndrome symptoms and prevent complications.
For many, optimizing gut health through holistic interventions can significantly improve nutrient absorption. Addressing inflammation, supporting the microbiome, and using bioavailable nutrients can enhance overall digestive function. With the right approach, individuals can minimize symptoms and maintain long-term health.

Frequently Asked Questions (FAQ) About Malabsorption
What are the long-term effects of malabsorption syndrome if left untreated?
If malabsorption syndrome is left untreated, the long-term consequences can be severe, affecting multiple systems in the body. Chronic nutrient deficiencies may lead to osteoporosis due to insufficient calcium absorption, anemia from iron or vitamin B12 deficiency, and neurological complications stemming from a lack of essential vitamins. Individuals with prolonged fat malabsorption symptoms often experience significant weight loss and muscle wasting, making them more susceptible to infections and fatigue. Additionally, untreated malabsorption diseases can increase the risk of cardiovascular issues, as the body struggles to absorb essential fatty acids and fat-soluble vitamins like A, D, E, and K. Over time, these deficiencies can also contribute to cognitive decline and memory issues, emphasizing the importance of early detection and intervention.
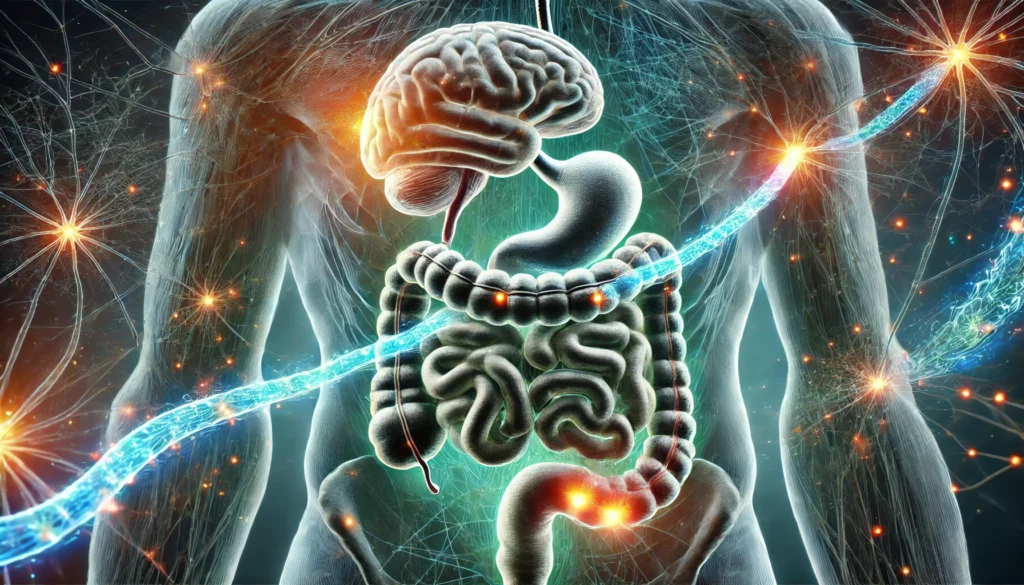
Can stress or anxiety contribute to malabsorption disorders?
Yes, stress and anxiety can play a significant role in worsening malabsorption disorders. Chronic stress affects digestion health by altering gut motility, increasing inflammation, and reducing the production of essential digestive enzymes. The gut-brain connection is well-documented, and psychological stress can exacerbate symptoms of intestinal malabsorption, leading to discomfort and irregular digestion patterns. Those experiencing persistent anxiety may develop gastrointestinal symptoms such as bloating, diarrhea, or malabsorption poop that resembles undigested food. Managing stress through meditation, exercise, and cognitive-behavioral therapy can help improve digestion and reduce the severity of malabsorption syndrome symptoms. Addressing both mental and digestive health is crucial for individuals looking to manage malabsorption effectively.
What dietary changes can help improve nutrient absorption?
Individuals struggling with malabsorption disorders can benefit from targeted dietary modifications that support digestion health. Incorporating easily digestible foods such as bone broth, steamed vegetables, and fermented foods can enhance the absorption of essential nutrients. Consuming healthy fats in moderation—such as avocados, olive oil, and coconut oil—may support individuals experiencing fat malabsorption syndrome. Additionally, soaking and sprouting grains and legumes can help break down anti-nutrients that hinder absorption, allowing the body to utilize more vitamins and minerals. Supplements like digestive enzymes and probiotics can also support gut health and aid in breaking down food more effectively. Personalized nutrition strategies, guided by a healthcare professional, are often the best way to manage malabsorption treatments effectively.
How can someone determine if they are experiencing malabsorption?
Recognizing malabsorption symptoms requires attention to changes in digestive patterns and overall well-being. One key indicator is experiencing chronic diarrhea or malabsorption poop that is oily, pale, or particularly foul-smelling. Fatigue, unintentional weight loss, and frequent nutrient deficiencies—such as brittle nails or hair thinning—can also point to malabsorption syndrome symptoms. Digestive discomfort, bloating, and a feeling of food sitting undigested in the stomach for extended periods may indicate problems with food absorption. How to tell definitively often requires diagnostic tests for malabsorption syndrome, including stool analysis, blood tests, and imaging studies. Consulting a healthcare provider for a comprehensive assessment is the best course of action for those suspecting a malabsorption disorder.
What are some of the most effective natural treatments for malabsorption?
Natural approaches to managing malabsorption disorder focus on supporting the digestive system and enhancing food absorption. How to treat malabsorption naturally includes incorporating herbal remedies like ginger, peppermint, and fennel, which aid digestion and reduce bloating. Bone broth and collagen supplements can help repair damage to the intestinal lining, particularly for individuals with celiac disease fat malabsorption stool issues. Probiotics and prebiotics are essential for restoring gut flora balance, which plays a key role in nutrient absorption. Ensuring adequate hydration also supports enzyme function and digestive processes. While these natural interventions can be beneficial, individuals with severe malabsorption diseases should seek medical guidance for a comprehensive treatment plan.
Are there specific medications available for treating malabsorption?
Yes, various medications for fat malabsorption and other forms of malabsorption syndrome exist, depending on the underlying cause. Enzyme replacement therapy, such as pancreatic enzyme supplements, helps individuals with pancreatic insufficiency break down and absorb fats and proteins more effectively. Bile acid sequestrants may be prescribed for those experiencing issues with bile acid diarrhea, which can contribute to intestinal malabsorption. For individuals with bacterial overgrowth contributing to malabsorption, targeted antibiotics can help restore gut flora balance. Vitamin and mineral supplementation, often in bioavailable forms like liposomal or sublingual options, may be recommended to correct deficiencies. A physician can determine the most appropriate medications based on individual malabsorption syndrome symptoms and underlying conditions.
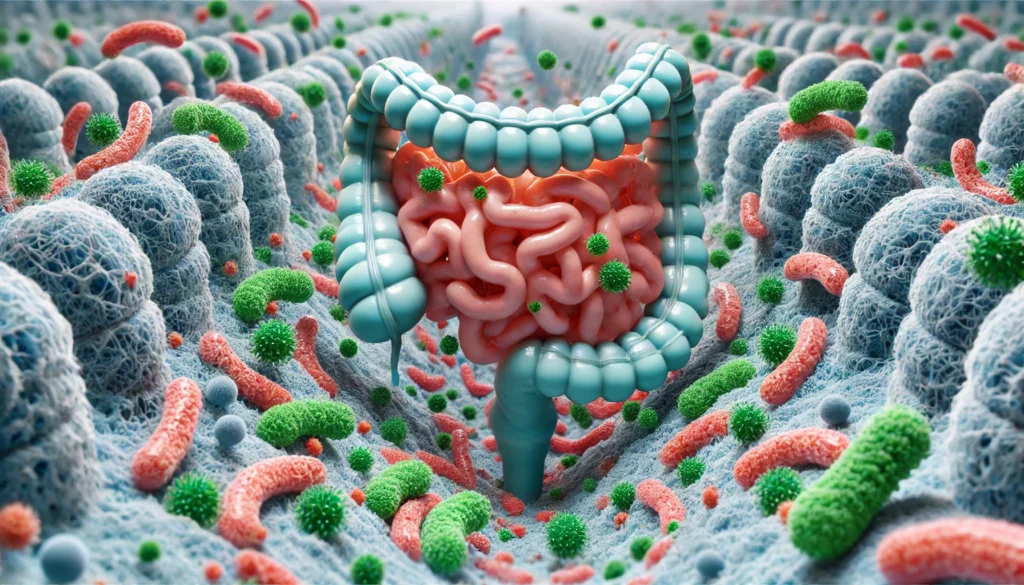
How does gut microbiome imbalance contribute to malabsorption issues?
A disrupted gut microbiome plays a significant role in many cases of malabsorption, affecting digestion efficiency and nutrient absorption. Beneficial gut bacteria help break down food and facilitate the absorption of essential vitamins, such as B12 and K2. When gut flora is imbalanced—due to factors like antibiotic overuse, poor diet, or chronic stress—harmful bacteria can proliferate, leading to gi malabsorption and chronic inflammation. Small intestinal bacterial overgrowth (SIBO) is one example where excessive bacterial growth interferes with digestion, leading to symptoms such as bloating and malabsorption of fat in stool. Restoring microbial balance through probiotics, prebiotics, and fiber-rich foods can help manage malabsorption treatments effectively.
Is malabsorption more common in certain age groups?
Malabsorption can affect individuals at any age, but certain groups are more vulnerable due to physiological changes or underlying conditions. Infants and young children may experience malabsorption diseases due to genetic disorders like cystic fibrosis or lactose intolerance. In adults, aging can lead to reduced digestive enzyme production, increasing the likelihood of fat malabsorption symptoms and nutrient deficiencies. Older adults are also at higher risk due to conditions such as atrophic gastritis, which impairs stomach acid production, making it harder to break down and absorb nutrients. Individuals with chronic gastrointestinal disorders or those who have undergone intestinal surgery are also at higher risk. Proper dietary strategies and medical interventions can help manage malabsorption syndrome in different age groups.
Can malabsorption syndrome be completely cured?
Whether malabsorption syndrome can be cured depends on the underlying cause and the individual’s overall health. Some forms, such as those caused by bacterial overgrowth or enzyme deficiencies, can be effectively treated with targeted interventions, leading to complete symptom resolution. However, chronic conditions like celiac disease fat malabsorption stool issues require lifelong dietary management to prevent malabsorption symptoms from recurring. Individuals with pancreatic insufficiency or structural gastrointestinal disorders may need long-term enzyme supplementation or medications for fat malabsorption. While malabsorption treatments can significantly improve symptoms and quality of life, ongoing monitoring and dietary adjustments are often necessary. Working closely with a healthcare provider can help manage malabsorption syndrome effectively and minimize long-term complications.
Conclusion: The Path to Better Nutrient Absorption
Understanding what causes malabsorption is the first step in reclaiming digestive health. By recognizing symptoms, undergoing proper diagnostic testing, and implementing effective treatments, individuals can address malabsorption disorder and improve overall well-being. While malabsorption syndrome presents challenges, targeted interventions and a commitment to gut health can lead to lasting improvements.
gut health, digestive health, nutrient absorption, intestinal health, food intolerance, enzyme deficiency, chronic diarrhea, gluten sensitivity, holistic digestion, gut microbiome, inflammation and digestion, probiotics for digestion, healthy digestion tips, SIBO treatment, pancreatic insufficiency, bile acid metabolism, nutrition deficiency, digestive wellness, optimal nutrient absorption, bioavailable nutrients
Further Reading:
What to know about malabsorption
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions

