Introduction: Why Insulin Control Is Critical for Effective Weight Loss
Weight loss advice often focuses on counting calories, cutting carbs, or hitting the gym. But beneath the surface of these familiar tactics lies a critical hormone that may be quietly sabotaging your efforts: insulin. Known primarily for its role in blood sugar regulation, insulin plays a deeper role in fat storage, hunger cues, and overall metabolism. When insulin levels are persistently high, it becomes far more difficult to burn fat, regardless of how diligently you diet or exercise.
Understanding the relationship between insulin and weight loss is essential for anyone seeking not only to shed pounds but to do so in a way that supports long-term health. Learning how to reduce insulin, manage insulin resistance, and support healthy insulin function naturally can transform your weight loss journey into one that aligns with your body’s biochemistry. This article will explore evidence-based strategies that show you how to keep insulin low, safely and effectively, for better metabolic health, energy balance, and lasting weight control.
You may also like: Why Am I Craving Sweets All of a Sudden? Expert-Backed Reasons and How to Stop Sugar Cravings Naturally
Understanding Insulin and Its Role in Fat Storage
Insulin is a hormone released by the pancreas in response to rising blood sugar levels, typically after eating carbohydrate-rich foods. Its job is to help move glucose from the bloodstream into the cells, where it can be used for energy or stored for future use. When insulin functions optimally, it keeps blood sugar stable and helps maintain energy balance. However, when insulin levels are chronically elevated—often due to poor diet, sedentary behavior, or stress—it signals the body to store excess calories as fat.
The link between insulin and weight loss lies in this storage mechanism. High insulin levels promote fat accumulation while simultaneously preventing the body from accessing fat stores for energy. Essentially, when insulin is elevated, the body shifts into a “storage” mode, making it very difficult to burn fat—even during calorie restriction. This is why simply eating less or exercising more doesn’t always yield results unless insulin levels are also addressed.
What Causes Insulin to Rise? Common Triggers of Elevated Insulin
There are several lifestyle and dietary factors that contribute to chronically high insulin levels. The most common and impactful cause is excessive intake of refined carbohydrates and sugars. When you eat foods like white bread, sugary snacks, or sweetened beverages, your blood sugar spikes, prompting the pancreas to release a surge of insulin. Over time, repeated insulin spikes can lead to insulin resistance, where cells become less responsive to insulin, causing even more insulin to be produced.
In addition to diet, stress is another major driver of elevated insulin. Chronic stress increases cortisol, a hormone that can impair insulin sensitivity. Poor sleep, inflammation, and physical inactivity also play roles in raising insulin levels. Recognizing these root causes helps clarify how to reduce insulin through sustainable lifestyle changes rather than temporary fixes or fad diets.
Dietary Shifts That Help Lower Insulin Naturally
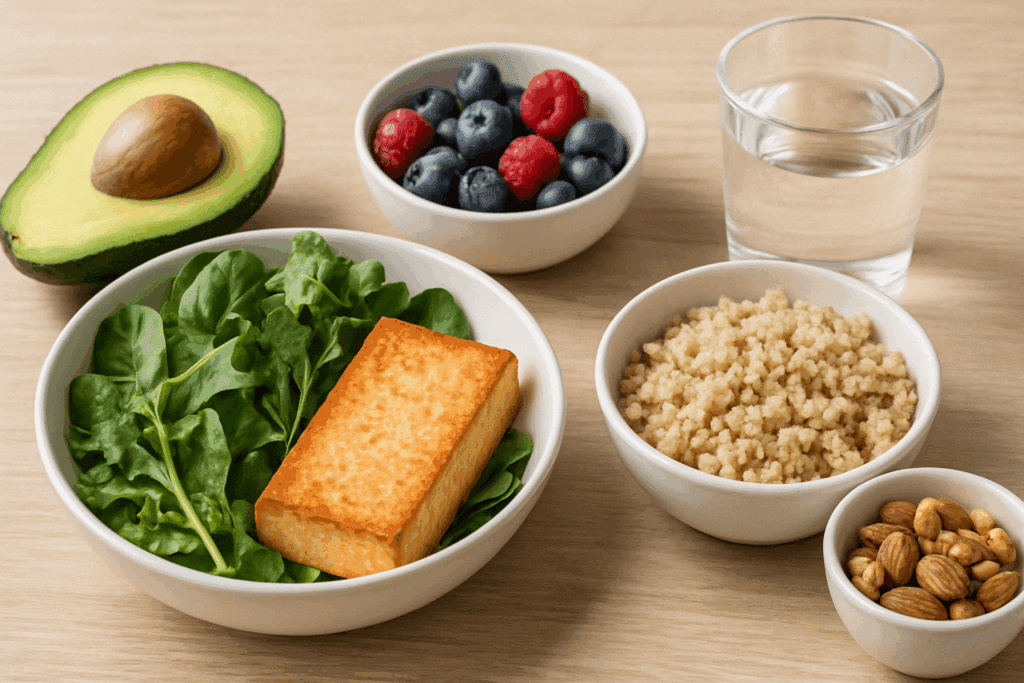
The first step toward lowering insulin is making smart, consistent changes to your diet. A diet rich in fiber, healthy fats, and lean proteins—particularly plant-based options—can blunt insulin spikes and promote better blood sugar balance. Reducing or eliminating refined carbohydrates and sugary beverages is essential. Instead, focus on whole foods like leafy greens, legumes, nuts, seeds, berries, and whole grains that digest more slowly and have a gentler effect on blood sugar.
Eating balanced meals that include protein and healthy fats slows digestion and reduces the insulin response. For example, pairing a serving of quinoa with vegetables and avocado is far more insulin-friendly than eating a bowl of white rice. The goal is not to eliminate all carbs but to choose those that nourish the body without triggering excessive insulin production. These dietary choices are at the heart of how to keep insulin low on a daily basis.
How Intermittent Fasting Supports Lowering Insulin
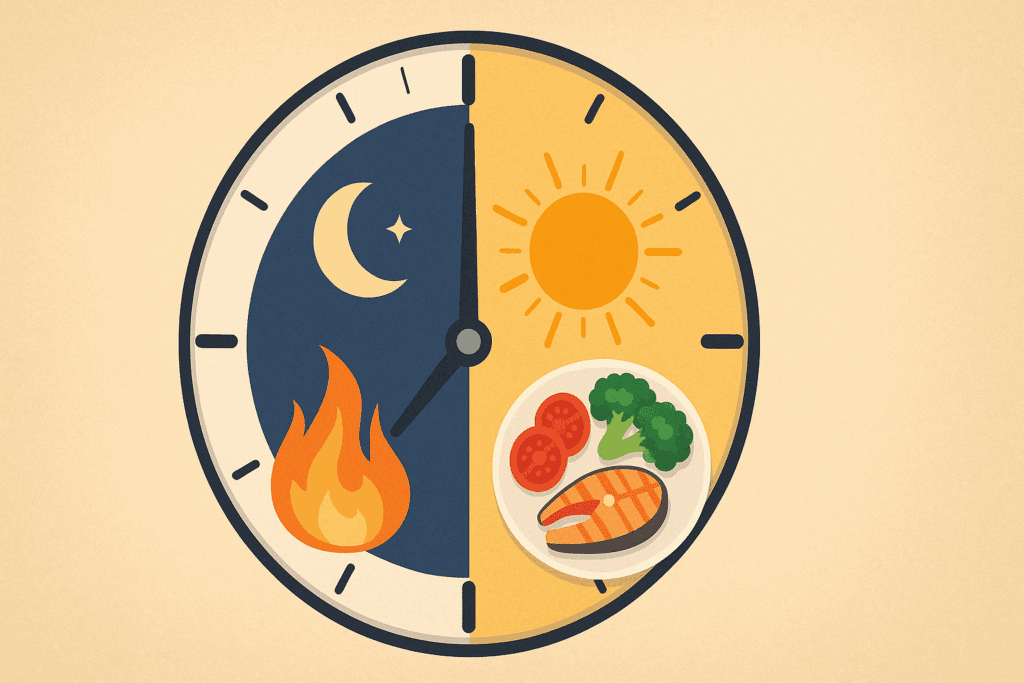
One of the most effective natural strategies for reducing insulin is intermittent fasting (IF). When you fast, your body has time to metabolize previously consumed glucose, allowing insulin levels to drop. In the absence of frequent food intake—especially carbohydrate-heavy snacks—your insulin response becomes more controlled, and your body can begin accessing stored fat for energy.
Various forms of intermittent fasting, such as the 16:8 method (16 hours fasting, 8-hour eating window) or alternate-day fasting, have shown significant benefits for both insulin sensitivity and weight loss. These methods allow insulin to remain low for longer periods, improving metabolic flexibility. Studies confirm that intermittent fasting is an effective and sustainable way to support insulin health and enhance fat metabolism.
For those asking, “how do I lower my insulin levels without medication?”, intermittent fasting offers a science-backed option that works with your body’s natural rhythms to regulate hormones and improve weight outcomes.

Exercise: A Powerful Tool to Improve Insulin Sensitivity
Physical activity is another pillar of effective insulin management. Exercise helps muscle cells become more sensitive to insulin, meaning the body doesn’t need to produce as much of it to maintain blood sugar control. Even a single workout can improve insulin sensitivity for up to 48 hours, making regular movement a powerful way to lower insulin.
Strength training and aerobic exercise both offer benefits, and the best approach is often a combination of the two. Resistance training builds lean muscle mass, which burns more glucose even at rest, while cardio exercises like walking, jogging, or cycling help the body process glucose more efficiently. A consistent fitness routine not only supports weight loss but plays a key role in how to reduce insulin naturally and holistically.
The Overlooked Role of Sleep and Stress in Insulin Regulation
Many people focus on diet and exercise but neglect the importance of sleep and stress management—two factors that directly impact insulin. Poor sleep, especially chronic sleep deprivation, disrupts the body’s ability to regulate blood sugar and insulin. One study showed that just a few nights of poor sleep can reduce insulin sensitivity by as much as 25%.
Similarly, ongoing stress elevates cortisol, which interferes with insulin’s function and raises blood sugar levels. Over time, this stress-induced hormonal imbalance can contribute to weight gain, especially around the abdominal area. Learning to manage stress through mindfulness, deep breathing, yoga, or time in nature is crucial for lowering insulin and maintaining long-term health.
A holistic approach to how to keep insulin low must include prioritizing restorative sleep and actively managing emotional stress. These often-overlooked factors are essential for breaking the cycle of insulin resistance and supporting lasting weight loss.

Supplements That May Help Lower Insulin Levels
While lifestyle changes are the foundation of insulin regulation, some supplements may offer additional support. Magnesium plays a key role in insulin signaling, and studies have shown that magnesium deficiency is linked to insulin resistance. Adding magnesium-rich foods like pumpkin seeds, spinach, and almonds—or supplementing if needed—may help improve insulin sensitivity.
Chromium is another trace mineral that may assist in glucose metabolism, and alpha-lipoic acid (ALA), a powerful antioxidant, has shown potential in enhancing insulin function. Additionally, cinnamon, particularly in extract form, has been studied for its ability to stabilize blood sugar and support lower insulin levels.
While supplements are not a cure-all, they can complement diet and lifestyle changes. If you’re asking, “how do I lower my insulin levels effectively?”, it’s worth exploring whether these nutrients can play a supportive role in your personalized plan. Always consult a healthcare provider before starting any new supplement, especially if you’re managing a medical condition.
Mindful Eating and Its Role in Insulin Regulation
Mindful eating is an emerging strategy for insulin control that extends beyond food choices to how we eat. When meals are consumed slowly, without distractions like screens or rushed environments, the body can better regulate digestive hormones, including insulin. Mindful eating promotes awareness of hunger and satiety cues, helping to prevent overeating—one of the major contributors to insulin spikes.
Chewing thoroughly, savoring each bite, and pausing between servings allows the body to fully process food and signals the brain when enough has been consumed. This behavioral shift is a subtle yet powerful way to support metabolic health and reduce the frequency and intensity of insulin responses. Practicing mindfulness around food helps people naturally eat less and avoid the constant grazing that keeps insulin levels high.
Incorporating mindful eating into your lifestyle offers a simple and intuitive solution for those seeking practical ways to lower insulin without resorting to restrictive diets or harsh calorie limits.
Recognizing the Signs of High Insulin and When to Seek Support
Many people live with elevated insulin levels without realizing it. Signs that insulin may be too high include intense cravings for sugar or carbs, frequent hunger (even after eating), energy crashes, difficulty losing weight, and increased abdominal fat. Skin tags, dark patches of skin (especially on the neck or armpits), and high triglyceride levels are also potential indicators of insulin resistance.
If these signs sound familiar, it may be time to consult a healthcare provider for blood tests, including fasting insulin and glucose. Early detection and intervention can help you reverse insulin resistance before it develops into prediabetes or type 2 diabetes. Armed with this information, you can create a personalized plan based on the principles outlined in this article, focusing on how to reduce insulin naturally and safely.
FAQ: Advanced Insights on Insulin and Weight Loss — Practical Approaches to Naturally Lower Insulin
1. Can high insulin levels affect hunger and food cravings?
Yes, elevated insulin levels can significantly impact hunger and food cravings. When insulin is consistently high, it suppresses the hormone glucagon, which normally helps maintain stable blood sugar levels. This leads to blood sugar crashes that trigger intense cravings, especially for sugary or carb-rich foods. Over time, this cycle contributes to overeating and weight gain, making the relationship between insulin and weight loss even more complex. Understanding how to reduce insulin through mindful eating and balanced nutrition not only supports metabolic health but can also stabilize appetite and reduce emotional or habitual cravings that derail weight management efforts.
2. How does alcohol consumption impact insulin levels and weight loss?
Alcohol can influence insulin in several nuanced ways, depending on the type, amount, and frequency of consumption. While moderate alcohol, particularly red wine, may have some insulin-sensitizing effects due to compounds like resveratrol, excessive intake often leads to spikes in triglycerides, liver fat accumulation, and insulin resistance. Chronic drinking also disrupts glucose metabolism and may lead to reactive hypoglycemia, which prompts the pancreas to release more insulin than necessary. For those focused on lowering insulin, it’s wise to limit alcohol intake or choose options with minimal sugar content. Balancing alcohol with high-fiber meals and hydration can also help keep insulin low during occasional indulgences.
3. Can mental health challenges interfere with efforts to lower insulin levels?
Mental health plays a surprisingly strong role in insulin regulation. Chronic anxiety, depression, and trauma often elevate cortisol, which in turn raises blood sugar and insulin secretion over time. Additionally, individuals with mood disorders may struggle with consistent routines around sleep, exercise, or nutrition, which are key to how to keep insulin low. Addressing mental health with professional support—such as therapy, mindfulness practices, or medication when appropriate—can create a more stable internal environment that promotes both emotional and metabolic balance. In this way, supporting mental wellness becomes a foundational piece in any effective insulin and weight loss strategy.
4. Are there cultural or social eating habits that make insulin control more difficult?
Yes, social and cultural factors can significantly impact insulin dynamics. Frequent celebratory meals, late-night dining traditions, and communal eating centered on carbohydrate-dense foods can lead to repeated insulin spikes. In cultures where bread, rice, or sweets are dietary staples, learning how to reduce insulin may require careful planning rather than total avoidance. Choosing to eat traditional meals in smaller portions or substituting with lower-glycemic versions allows individuals to honor cultural norms while still working to lower insulin naturally. Education and community-based health initiatives that respect cultural preferences can empower more people to adopt sustainable insulin-friendly habits.
5. How do hormonal changes during menopause influence insulin and weight gain?
Hormonal shifts during perimenopause and menopause often lead to increased insulin resistance, particularly due to declining estrogen levels. Estrogen plays a protective role in maintaining insulin sensitivity, and when it drops, women may experience increased abdominal fat and difficulty losing weight. This makes it especially important during this life stage to understand how do I lower my insulin levels through diet, activity, and stress management. Strength training becomes particularly valuable, as it helps maintain lean mass and improves glucose uptake. By adapting lifestyle habits to these hormonal changes, women can regain better control over both insulin and weight.
6. Is it possible to lower insulin without following a strict diet plan?
Absolutely. While structured diets can be helpful for some, lowering insulin doesn’t require rigid meal plans or elimination diets. Instead, the focus should be on consistency with foundational habits: reducing added sugars, choosing whole foods, managing stress, and prioritizing sleep. Those wondering how to keep insulin low sustainably should start with small, realistic changes—like swapping sugary beverages for water, adding more fiber to meals, or taking short walks after eating. These micro-habits add up over time, and often deliver better long-term results than extreme dietary restrictions that are hard to maintain.
7. Can insulin be lowered through environmental or lifestyle design?
Surprisingly, yes—environmental cues can deeply influence hormonal regulation. For instance, exposure to natural light in the morning can help regulate circadian rhythms, which in turn support better cortisol and insulin balance throughout the day. Likewise, designing your kitchen and workspace to promote mindful eating (e.g., keeping fruit on the counter instead of cookies) reinforces habits that help lower insulin passively. Even standing desks or prompts to move regularly during the day can support metabolic flexibility. Integrating insulin and weight loss strategies into your daily environment makes them easier to follow and more effective over the long term.
8. Are there emerging therapies or research areas exploring insulin control and weight management?
Yes, several exciting developments are underway in the realm of insulin research. Nutrigenomics—the study of how genes and diet interact—may one day help personalize insulin-lowering strategies based on individual genetic profiles. Additionally, compounds like berberine and inositol are gaining traction for their potential to mimic the effects of insulin or improve its sensitivity. Some researchers are also exploring how gut microbiome diversity influences insulin signaling, suggesting that probiotics and fermented foods could support how to reduce insulin naturally. While these areas are still emerging, they point toward a future of more tailored, holistic metabolic care.
9. How do shift work and irregular schedules impact insulin and weight control?
People who work night shifts or rotating schedules often face challenges with circadian misalignment, which disrupts the normal release of insulin and cortisol. Eating at night when the body is less insulin-sensitive can lead to higher blood sugar and increased fat storage. For those in these roles, being intentional about meal timing and food choices becomes critical to lowering insulin. Strategic fasting, high-protein meals earlier in the day, and minimizing nighttime snacking can help mitigate these effects. Understanding how to keep insulin low in non-traditional lifestyles requires flexible, individualized strategies that prioritize circadian-friendly eating whenever possible.
10. What’s the long-term benefit of keeping insulin low beyond weight loss?
While many people focus on insulin and weight loss, the benefits of insulin control extend far beyond aesthetics. Maintaining lower insulin levels helps reduce the risk of cardiovascular disease, certain cancers, and cognitive decline. It also improves energy stability, reduces inflammation, and supports hormonal balance across the lifespan. Over time, learning how to reduce insulin is less about short-term results and more about creating a strong foundation for aging well. When insulin is balanced, the entire metabolic system functions more efficiently, making how do I lower my insulin levels not just a temporary question, but a lifelong health pursuit.
Conclusion: Lasting Weight Loss Starts with Insulin Balance
For anyone struggling to lose weight despite doing “everything right,” the missing link may be hormonal. Insulin is not just a blood sugar hormone—it’s a key metabolic regulator that determines whether your body stores fat or burns it. Understanding the connection between insulin and weight loss changes the game. It shifts the focus from willpower and calorie restriction to hormonal balance and metabolic efficiency.
Knowing how to keep insulin low involves more than cutting carbs. It’s about eating whole, nourishing foods, staying active in a way that supports your lifestyle, managing stress, prioritizing quality sleep, and being mindful at meals. Whether through intermittent fasting, smarter food choices, or supporting sleep and stress, each step you take to lower insulin naturally can help you regain control of your health and weight.
The path to metabolic wellness is not about quick fixes—it’s about long-term commitment to habits that respect the body’s internal rhythms. If you’ve been wondering how do I lower my insulin levels safely, this guide offers a clear, actionable framework. With science-backed strategies and a holistic mindset, you can transform your health from the inside out—starting with your hormones, starting with insulin.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
13 Ways to Lower Your Insulin Levels
How can I lower my insulin levels?
Diet tips to improve insulin resistance
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.

