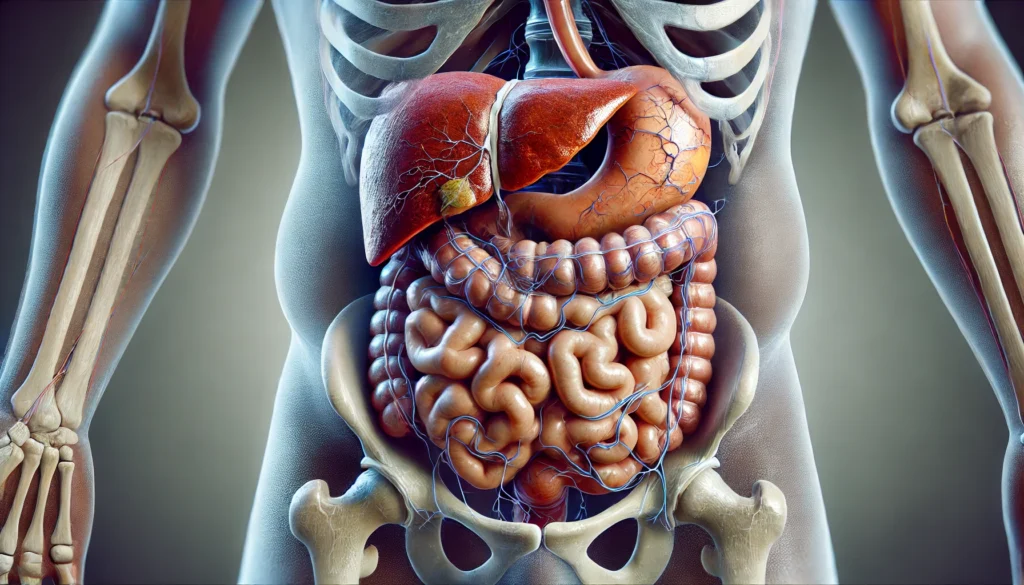
Cirrhosis is a severe and progressive liver condition characterized by extensive scarring, leading to impaired liver function and, in many cases, the development of complications such as ascites. Ascites is the abnormal accumulation of fluid in the abdominal cavity, signaling the decompensation of liver function. Understanding the signs and symptoms of cirrhosis and ascites is crucial for early detection, proper management, and improved patient outcomes. As cirrhosis advances, symptoms range from mild and manageable to severe and life-threatening. Knowing what to expect at different stages can help individuals and healthcare providers make informed decisions about treatment and lifestyle adjustments.
You may also like: The Best Liver Detox Supplements: How to Choose Safe and Effective Support for Your Liver
The Stages of Cirrhosis and the Onset of Symptoms
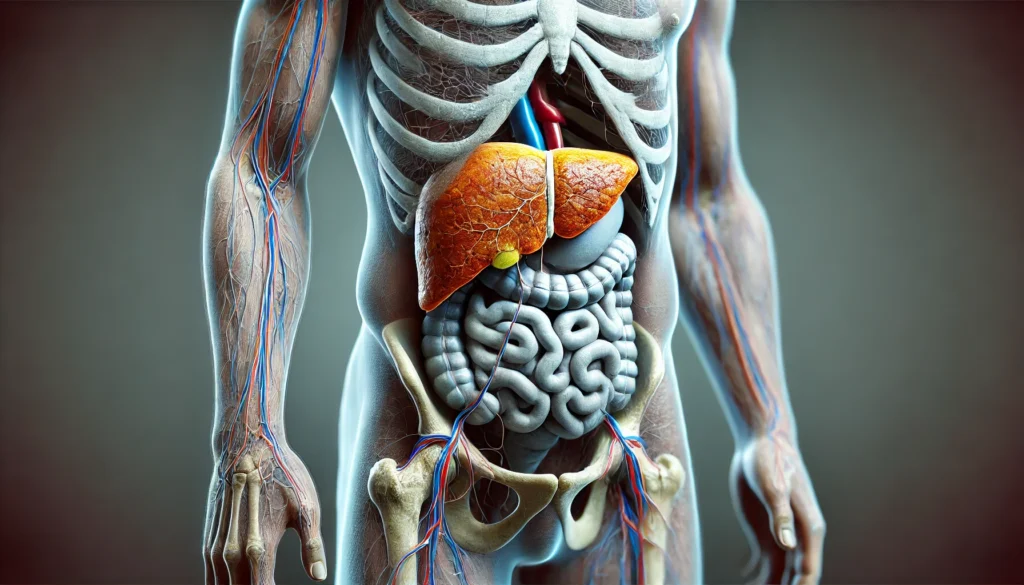
Cirrhosis progresses through several stages, from compensated to decompensated disease. In its early stages, the liver may still perform essential functions despite the presence of fibrosis. However, as scarring worsens, liver function deteriorates, leading to noticeable symptoms and complications. The first signs often include fatigue, weakness, loss of appetite, and mild jaundice. As liver damage progresses, symptoms become more pronounced, with complications such as hepatic encephalopathy, variceal bleeding, and ascites marking the transition to decompensated cirrhosis. Understanding the levels of cirrhosis of the liver helps in predicting disease progression and guiding medical interventions.
How Cirrhosis Leads to Ascites: Pathophysiology and Contributing Factors
Ascites occurs when cirrhosis disrupts normal liver function and blood flow, leading to portal hypertension. This condition increases pressure in the portal vein, causing fluid leakage into the abdominal cavity. Additionally, reduced albumin production by the liver exacerbates fluid retention. The imbalance of sodium and water regulation further contributes to ascites development. Alcoholic cirrhosis of the liver with ascites is particularly concerning, as chronic alcohol consumption exacerbates liver damage and accelerates fluid buildup. Patients with cirrhosis and fluid retention often experience discomfort, bloating, and breathing difficulties due to the increasing abdominal pressure.
Recognizing the Symptoms of Ascites and Cirrhosis Progression
Symptoms of ascites include a visibly swollen abdomen, weight gain, and a feeling of fullness. In severe cases, patients may develop spontaneous bacterial peritonitis, an infection of the ascitic fluid that requires immediate medical attention. Cirrhosis stomach swelling often leads to additional complications such as hernias and restricted mobility. As cirrhosis advances, patients may experience jaundice, easy bruising, confusion due to hepatic encephalopathy, and worsening fatigue. End-stage liver cirrhosis symptoms include profound weakness, severe ascites, significant muscle wasting, and multiorgan failure, often signaling the final stages of the disease.
Treatment and Management Strategies for Cirrhosis and Ascites
The management of cirrhosis and ascites focuses on slowing disease progression, reducing complications, and improving quality of life. Lifestyle modifications, including alcohol cessation and dietary changes, play a critical role in treatment. Medications such as diuretics help control fluid retention, while paracentesis may be necessary for severe ascites cases. Liver transplantation remains the only curative option for advanced cirrhosis. Understanding how does cirrhosis lead to ascites enables patients and healthcare providers to take proactive steps in managing the condition and reducing complications.
Preventing Further Liver Damage and Promoting Wellness
Preventative measures are crucial for individuals with cirrhosis or those at risk of developing the disease. Vaccination against hepatitis B and C, maintaining a healthy weight, and avoiding hepatotoxic substances can help preserve liver function. Differentiating between hepatitis vs cirrhosis is essential for early intervention and appropriate treatment. Routine medical monitoring, adherence to prescribed treatments, and patient education about cirrhosis and fluid retention contribute to better outcomes and improved overall health.
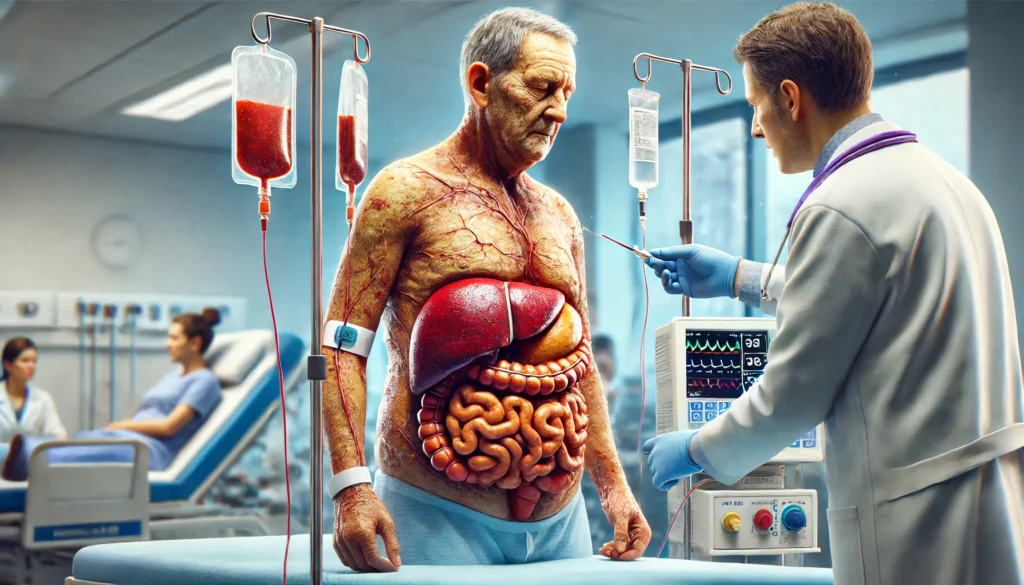
Understanding the Stages of Death from Cirrhosis of the Liver
As cirrhosis progresses to its final stages, symptoms become more severe, and complications increase. The liver’s ability to function declines significantly, leading to hepatic failure and systemic effects. Decompensated cirrhosis symptoms such as profound jaundice, recurrent infections, severe ascites, and mental confusion indicate poor prognosis. Swollen abdomen cirrhosis liver cases often result in respiratory distress, making breathing difficult due to excessive fluid accumulation. Hospice care and palliative treatment become essential in managing pain and ensuring comfort in the liver cirrhosis late stages.
Frequently Asked Questions (FAQ) About Cirrhosis and Ascites
1. What stage of liver disease is ascites most commonly associated with?
Ascites is most commonly associated with decompensated cirrhosis, which is considered an advanced stage of liver disease. At this stage, the liver’s ability to regulate fluid balance is severely impaired, leading to excessive fluid accumulation in the abdominal cavity. While early-stage cirrhosis may not present with ascites, progression to moderate or severe hepatic cirrhosis with ascites often indicates significant liver dysfunction. Patients with cirrhosis of the liver with ascites require close monitoring to prevent complications such as spontaneous bacterial peritonitis. Lifestyle modifications, sodium restriction, and diuretics are often the first line of management before considering more advanced treatments.
2. How does cirrhosis lead to ascites?
Cirrhosis leads to ascites due to increased pressure in the portal vein (portal hypertension) and reduced production of albumin, a protein that helps maintain blood vessel integrity. As cirrhosis progresses, scarring of the liver obstructs normal blood flow, causing fluid to leak into the abdominal cavity. Additionally, hormonal imbalances result in sodium and water retention, exacerbating cirrhosis and fluid retention. When ascites develops, it often indicates significant liver impairment and an increased risk of further complications. Managing fluid buildup through dietary changes and medication is essential to slow disease progression.
3. What are the symptoms of decompensated cirrhosis and ascites?
Decompensated cirrhosis symptoms include jaundice, confusion (hepatic encephalopathy), and a swollen abdomen (cirrhosis stomach swelling). In cases of hepatic cirrhosis with ascites, patients often experience shortness of breath due to increased abdominal pressure. Cirrhosis and fluid retention may also cause significant discomfort, leading to difficulty in movement and daily activities. As the liver function declines further, patients may develop bleeding tendencies, kidney dysfunction, and an increased risk of infections. Early medical intervention is crucial to managing symptoms and preventing further deterioration.
4. What is the difference between hepatitis and cirrhosis?
Hepatitis and cirrhosis are both liver conditions but differ in their causes and progression. Hepatitis refers to liver inflammation, which can be caused by viruses, alcohol, or autoimmune disorders. While hepatitis can sometimes lead to cirrhosis, not all cases progress to severe liver damage. Cirrhosis, on the other hand, is characterized by irreversible scarring and liver dysfunction. Patients with alcoholic cirrhosis of liver with ascites often have a history of long-term alcohol use, while viral hepatitis-related cirrhosis develops over years of chronic infection. Monitoring liver enzyme levels and imaging studies help differentiate between these conditions.
5. What are the stages of death from cirrhosis of the liver?
The stages of death from cirrhosis of the liver progress from compensated cirrhosis (where the liver still functions relatively well) to decompensated cirrhosis, and eventually to end-stage liver failure. In the final stages, patients experience severe complications such as cirrhosis of the liver abdominal swelling, kidney failure, and hepatic encephalopathy. Cirrhosis death stages may also include gastrointestinal bleeding due to ruptured varices in the esophagus or stomach. At this point, supportive care and palliative measures become the main focus to improve the patient’s quality of life. Liver transplantation may be the only curative option for those eligible.
6. How is ascites of hepatic cirrhosis treated?
The treatment for ascites of hepatic cirrhosis typically includes sodium restriction, diuretics, and paracentesis (fluid drainage). In patients with refractory ascites that do not respond to initial treatments, a transjugular intrahepatic portosystemic shunt (TIPS) may be considered to relieve portal hypertension. Liver cirrhosis fluid retention can be controlled with proper dietary management, but severe cases require frequent medical intervention. In some cases, infections such as spontaneous bacterial peritonitis (SBP) may develop, necessitating antibiotic therapy. Long-term management includes close monitoring of kidney function and consideration of liver transplantation if cirrhosis progresses.
7. What complications arise from cirrhosis and ascites?
Cirrhosis and ascites can lead to numerous complications, including spontaneous bacterial peritonitis (SBP), hepatorenal syndrome (kidney failure due to liver disease), and malnutrition. Patients with a swollen abdomen cirrhosis liver often experience breathing difficulties and reduced appetite, leading to weight loss and muscle wasting. Additionally, cirrhosis stomach swelling increases the risk of hernias due to increased intra-abdominal pressure. Hepatic encephalopathy, characterized by confusion and cognitive impairment, is another serious complication of advanced liver disease. Timely intervention and ongoing medical care are essential to managing these risks.
8. Can mild decompensation liver cirrhosis be reversed?
Mild decompensation liver cirrhosis can sometimes be stabilized with lifestyle changes and proper medical treatment. Unlike end-stage liver cirrhosis symptoms, which indicate irreversible damage, early intervention may help slow progression and even improve liver function. Abstinence from alcohol, antiviral therapy for hepatitis, and weight management for fatty liver disease can aid in recovery. While the scarring itself is not reversible, improved liver function may delay or prevent further deterioration. Regular monitoring with imaging and blood tests helps assess the effectiveness of treatment strategies.
9. Why does cirrhosis cause a swollen stomach?
Cirrhosis swollen stomach is primarily caused by fluid accumulation due to portal hypertension and low protein production. The liver’s reduced ability to synthesize albumin leads to fluid leakage into the abdominal cavity, resulting in cirrhosis of the liver abdominal swelling. This condition can become severe, causing discomfort, pressure on the lungs, and difficulty eating. Management includes fluid restriction, diuretics, and, in some cases, therapeutic paracentesis. Addressing the underlying liver disease is crucial to reducing the risk of recurrent ascites.
10. What are the levels of cirrhosis of the liver, and how do they impact prognosis?
The levels of cirrhosis of the liver range from compensated to decompensated cirrhosis and ultimately end-stage liver disease. Compensated cirrhosis means the liver is still functioning, often with few or no symptoms. Decompensated cirrhosis, marked by cirrhosis and fluid retention, jaundice, and encephalopathy, significantly impacts quality of life and prognosis. In liver cirrhosis late stages, complications such as kidney failure and severe bleeding become more common. While early-stage cirrhosis can be managed with lifestyle changes, late-stage disease often requires liver transplantation as the only curative option.
Conclusion: Recognizing Cirrhosis and Ascites for Better Management
Understanding cirrhosis and ascites is vital for early detection and effective management. Recognizing the symptoms of hepatic cirrhosis with ascites allows for timely intervention and improved patient care. Awareness of cirrhosis swollen stomach and cirrhosis of the liver abdominal swelling can help individuals seek medical attention before complications arise. With advancements in treatment and better lifestyle choices, patients with cirrhosis can manage their condition effectively and improve their quality of life.
liver disease progression, portal hypertension complications, chronic liver disease signs, managing cirrhosis symptoms, hepatic failure prevention, early signs of cirrhosis, liver fibrosis symptoms, cirrhosis dietary recommendations, ascites treatment options, hepatic encephalopathy causes, end-stage liver disease management, liver transplant eligibility, preventing liver cirrhosis, alcohol-related liver damage, liver detoxification strategies, fluid retention and liver disease, jaundice and cirrhosis, cirrhosis pain management, hepatology treatment advancements, lifestyle changes for liver health
Further Reading:
Fluid retention in cirrhosis: pathophysiology and management
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.

