Introduction: Building a Stronger Heart Through Smarter Living
Congestive heart failure (CHF) often signals a need for significant adjustments in daily life, but it should not be viewed as the end of vitality or physical performance. On the contrary, it can serve as a turning point toward healthier living and smarter strategies for endurance and stamina. Medical advancements and evidence-based lifestyle modifications now allow individuals with CHF to achieve improved quality of life and even enhanced physical performance. Instead of relying solely on medication, a multifaceted approach rooted in personalized nutrition, exercise, sleep, and stress management empowers patients to take charge of their health. In this article, we explore practical and medically sound lifestyle changes for congestive heart failure that go beyond survival—focusing instead on thriving through endurance, energy, and strength.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice
Understanding CHF and Its Influence on Physical Capacity
CHF occurs when the heart becomes too weak or stiff to pump blood efficiently, leading to symptoms like fatigue, breathlessness, swelling, and decreased exercise tolerance. These effects can limit the ability to perform even basic daily activities, let alone engage in structured exercise. However, not all physical limitations are inevitable. Many of the common symptoms are worsened by physical deconditioning—a cycle of inactivity that further weakens the muscles and the cardiovascular system.
Research shows that carefully guided physical activity can improve oxygen utilization, enhance heart efficiency, and even reverse some of the functional impairments associated with CHF. By understanding how the condition impacts the body’s energy systems and muscular endurance, individuals can begin to adopt targeted CHF lifestyle changes that promote physical performance and reduce disease progression.

Smart Nutrition to Fuel the Failing Heart
Nutrition plays a foundational role in managing heart failure and enhancing stamina. A diet designed for CHF should reduce the heart’s workload while supplying consistent energy and supporting metabolic health. Sodium restriction is crucial. Excess salt increases fluid retention, making it harder for the heart to function and worsening symptoms like edema and shortness of breath. Keeping sodium intake below 2,000 milligrams per day is typically recommended.
Beyond salt reduction, a heart-healthy diet includes whole foods rich in fiber, antioxidants, and essential nutrients. Leafy greens, berries, legumes, and omega-3-rich foods like salmon and flaxseeds help reduce inflammation and support cardiac muscle function. These foods stabilize blood sugar, enhance circulation, and provide sustained energy—an essential component for anyone looking to maintain endurance despite CHF.
Nutrient-dense diets also support lean body mass, which is critical in heart failure management. Muscle tissue helps regulate metabolism and enhances movement economy. By prioritizing high-quality calories and avoiding processed foods, patients can nourish their bodies while supporting performance.

Sustainable Weight Management Without Muscle Loss
Carrying excess weight adds stress to the heart and can worsen CHF symptoms. However, losing weight too quickly or without proper nutrient support can result in the loss of muscle mass, which diminishes endurance and weakens the body’s overall resilience.
The key is to aim for gradual fat loss while preserving muscle through adequate protein intake and light resistance training. Legumes, fish, eggs, and plant-based protein sources can provide essential amino acids without burdening the cardiovascular system. Incorporating moderate strength exercises—like bodyweight squats, resistance band routines, or light dumbbell training—helps maintain muscular health even in individuals with advanced CHF.
Maintaining a healthy weight isn’t just about appearance or numbers on a scale—it plays a significant role in energy management. Less excess fat means the heart doesn’t have to work as hard, especially during physical activity. This leads to better oxygen delivery, reduced fatigue, and improved stamina in daily life.

Exercise as Medicine: Tailored Movement for Endurance and Strength
Exercise is one of the most powerful CHF lifestyle changes when it comes to improving endurance and cardiac function. Despite outdated assumptions, most individuals with CHF benefit from physical activity—when it’s done correctly.
Cardiac rehabilitation programs, often prescribed after a heart-related event or hospitalization, provide medically supervised exercise plans that gradually build endurance, flexibility, and strength. These programs are evidence-based and tailored to individual fitness levels. They often start with low-impact aerobic activities such as walking, swimming, or cycling on a recumbent bike.
Over time, these routines lead to improved cardiovascular capacity, better breathing efficiency, and enhanced muscular endurance. Resistance training, done two to three times per week, can complement aerobic work by preserving muscle mass and promoting metabolic health. Importantly, these physical gains translate into real-world performance—walking further without resting, climbing stairs with less effort, or enjoying active hobbies again.

The Overlooked Role of Sleep and Stress in Heart Performance
Sleep and stress have profound effects on cardiac function, particularly in individuals managing CHF. Poor sleep—whether due to anxiety, discomfort, or undiagnosed sleep apnea—can reduce recovery, impair metabolism, and elevate blood pressure. It also saps energy, making physical activity more difficult and less enjoyable.
Improving sleep hygiene by establishing consistent sleep schedules, limiting blue light before bed, and elevating the head with pillows to reduce fluid buildup in the lungs can significantly improve rest. In some cases, sleep apnea treatment (such as CPAP therapy) may be necessary.
Stress, meanwhile, triggers the release of cortisol and adrenaline, which place added strain on the heart. Long-term stress also promotes inflammation, impairs immunity, and contributes to emotional exhaustion. Practices such as deep breathing, mindfulness meditation, guided imagery, and yoga can reduce stress levels and improve both heart rate variability and emotional resilience. These techniques help individuals maintain the motivation needed for other CHF lifestyle changes while directly supporting cardiovascular stability.
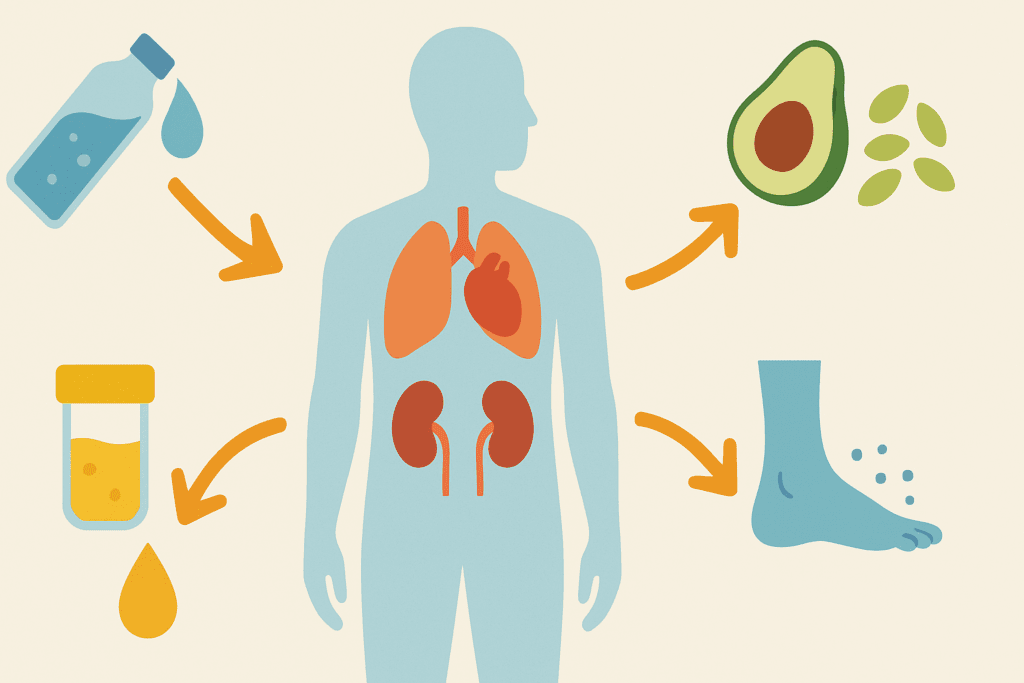
Hydration, Electrolytes, and Fluid Monitoring for Peak Function
Fluid balance is a delicate matter for those living with CHF. Too much fluid leads to swelling, pulmonary congestion, and fatigue. Too little can cause dehydration, low blood pressure, and kidney dysfunction. The goal is to maintain hydration levels that support cellular function without overburdening the heart.
Daily fluid restrictions, often between 1.5 to 2 liters, are commonly advised. Electrolytes—especially sodium, potassium, and magnesium—must also be closely monitored, especially in patients taking diuretics. Electrolyte-rich but heart-safe foods such as avocados, spinach, pumpkin seeds, and beans can help maintain a healthy balance.
Careful monitoring of body weight, urine output, and physical symptoms (like swelling or shortness of breath) allows patients to detect early signs of imbalance. Working with a healthcare provider to adjust fluid and medication regimens based on these markers is one of the most practical and important lifestyle changes for congestive heart failure.
The Importance of Medication Adherence and Communication
While lifestyle changes can dramatically support performance and heart health, they are most effective when integrated with appropriate medical treatment. Medications for CHF—such as beta-blockers, ACE inhibitors, ARBs, and diuretics—are essential for controlling symptoms, preventing disease progression, and improving survival.
However, missed doses, inconsistent timing, or poor understanding of medications can undermine their effectiveness. Patients should use pill organizers, set reminders, and keep a medication journal to improve adherence. Digital health tools and mobile apps can further support accountability and coordination.
Crucially, patients must communicate with their providers when they make lifestyle adjustments. Changes in diet, exercise, or supplement use can impact how medications are absorbed or metabolized. Providers can then adjust doses or offer guidance to ensure safety and efficacy, making sure that every aspect of care is synchronized.
Rethinking Endurance: It’s More Than Physical
When people think of endurance, they often imagine running marathons or biking long distances. But in the context of CHF, endurance can also mean walking to the mailbox without stopping, climbing stairs with steady breath, or playing with grandchildren without excessive fatigue.
Mental endurance plays just as vital a role. Living with a chronic condition requires emotional strength, consistent effort, and a positive mindset. Cultivating this kind of endurance involves small, achievable goals, regular reflection, and celebrating progress. Whether it’s increasing a walking distance by a few feet or mastering a new healthy recipe, these wins reinforce motivation and foster hope.
Functional fitness—real-world strength and stamina—emerges when physical and mental endurance work in harmony. It’s the ability to live independently, engage socially, and enjoy life despite a medical diagnosis. Through consistent lifestyle changes for congestive heart failure, patients often discover new sources of strength that redefine what performance truly means.
Education and Support: The Cornerstones of Sustainable Progress
No one should face CHF alone. Emotional support, education, and accountability are vital for success. Spouses, friends, family, or caregivers can help with meal preparation, exercise encouragement, and medical follow-up. Joining support groups, whether in-person or online, offers a sense of shared experience and practical tips from others on similar journeys.
Education also plays a crucial role. Understanding the “why” behind each lifestyle change increases commitment and reduces resistance. Healthcare providers, dietitians, physical therapists, and health coaches all contribute to a comprehensive understanding of CHF management.
The more informed patients are, the more empowered they feel to make lasting changes. That empowerment—combined with supportive relationships—is the true foundation of endurance in the context of chronic illness.
Frequently Asked Questions: Lifestyle Changes for Congestive Heart Failure That Support Endurance and Performance
1. How can CHF lifestyle changes help with long-term endurance beyond basic cardiac function? CHF lifestyle changes can support long-term endurance by improving mitochondrial efficiency and peripheral oxygen utilization—factors often overlooked in standard heart failure care. These improvements happen gradually through consistent movement, proper hydration, and micronutrient support. When muscles become more efficient at extracting and using oxygen, fatigue decreases, and patients can sustain physical activity for longer durations. Over time, even moderate lifestyle adjustments can lead to measurable gains in VO2 max and muscular endurance, both critical for daily stamina. These adaptations are especially important in helping individuals with congestive heart failure maintain autonomy and reduce hospitalizations.
2. Can lifestyle changes for congestive heart failure improve cognitive performance as well as physical stamina? Yes, cognitive benefits are an important but often underappreciated outcome of comprehensive CHF lifestyle changes. Improved circulation from light aerobic exercise and better nutrition supports brain oxygenation, which can help with memory, focus, and executive function. Inflammatory markers linked to both heart failure and cognitive decline often decrease with sustained lifestyle improvements. Additionally, better sleep and stress management—two crucial components of lifestyle changes for congestive heart failure—are known to enhance mental clarity. This holistic improvement in both mind and body can significantly enhance quality of life and the ability to engage meaningfully in daily activities.
3. How do CHF lifestyle changes differ for younger patients versus older adults? Younger individuals with CHF often benefit from more intensive physical conditioning programs, as their bodies may be more resilient and adaptable to structured exercise. For older adults, the focus of lifestyle changes for congestive heart failure often shifts toward fall prevention, flexibility, and maintaining independence through functional fitness. Nutritional strategies may also differ, with older adults requiring more emphasis on protein to combat sarcopenia. Social support systems and cognitive health become more central for seniors, while younger patients might prioritize career integration and reproductive planning. Regardless of age, the core principles of CHF lifestyle changes—tailored exercise, heart-healthy eating, and stress management—remain essential.
4. Are there emerging technologies that support CHF lifestyle changes more effectively today? Yes, technology is playing an increasingly important role in facilitating sustainable CHF lifestyle changes. Wearable devices can track heart rate, oxygen saturation, and even detect arrhythmias, providing real-time feedback on physical performance. Smartphone apps tailored to congestive heart failure now allow users to log symptoms, medication schedules, and hydration levels. Telemedicine platforms also offer virtual cardiac rehab programs, bringing expert guidance directly into the home. These innovations empower patients to take a more active role in their health, reinforcing adherence to lifestyle changes for congestive heart failure through instant feedback and personalized analytics.
5. How do social and emotional factors influence success in adopting CHF lifestyle changes? Social dynamics have a profound effect on how well individuals adopt and maintain lifestyle changes for congestive heart failure. Emotional support from family and peers can significantly boost compliance and motivation, especially during setbacks. Participation in community or online support groups provides encouragement, accountability, and practical advice. On the emotional side, unresolved grief, fear of illness progression, or frustration with physical limitations can undermine progress. Addressing these emotional barriers through counseling or behavioral therapy can dramatically improve adherence to CHF lifestyle changes and enhance both emotional and physical resilience.
6. What role does functional medicine play in complementing traditional CHF care? Functional medicine focuses on identifying and addressing root causes of illness, often through personalized lifestyle interventions. In the context of CHF lifestyle changes, this approach can include nutrient optimization, advanced metabolic testing, and gut microbiome support to reduce systemic inflammation. Functional practitioners may also explore underlying hormonal imbalances, micronutrient deficiencies, or chronic infections that could be contributing to cardiac strain. When integrated with conventional care, functional medicine can help refine dietary strategies, supplement protocols, and stress reduction techniques to better support congestive heart failure management. This integrative model appeals to patients seeking a proactive, systems-based approach to performance enhancement.
7. Can a plant-based diet alone support the necessary endurance for those with CHF? A well-planned plant-based diet can absolutely support endurance and heart health in individuals with CHF. It should include a variety of legumes, whole grains, nuts, seeds, and leafy greens to ensure adequate protein, iron, and B vitamins—all of which are vital for energy metabolism and oxygen transport. However, certain nutrients like vitamin B12 and omega-3 fatty acids may require supplementation or careful sourcing from fortified foods. This dietary strategy can reduce inflammation and improve vascular health, aligning well with the goals of lifestyle changes for congestive heart failure. With proper guidance, plant-based diets can be both cardioprotective and performance-enhancing.
8. How can caregivers support the implementation of lifestyle changes for congestive heart failure? Caregivers play an instrumental role in the successful adoption of CHF lifestyle changes. Their involvement often determines whether dietary recommendations, medication regimens, and exercise plans are followed consistently. Beyond logistics, caregivers provide emotional encouragement, help recognize early warning signs of symptom worsening, and assist in communication with healthcare providers. Training caregivers in the principles of CHF management and involving them in care planning enhances long-term outcomes. Their support can transform lifestyle changes for congestive heart failure from a solitary effort into a collaborative, sustainable routine.
9. What are the most underestimated challenges when maintaining CHF lifestyle changes long term? One frequently underestimated challenge is behavioral fatigue—the gradual loss of motivation that can occur months or even years into a lifestyle regimen. Another is the social pressure to deviate from dietary or activity guidelines during holidays, travel, or social events. Some individuals may also experience emotional burnout or develop unrealistic expectations, leading to discouragement when progress slows. Environmental factors, such as limited access to healthy foods or safe exercise spaces, can further complicate adherence. Understanding these nuanced barriers is essential to designing more resilient and realistic lifestyle changes for congestive heart failure.
10. How might the future of CHF treatment evolve in terms of lifestyle integration? The future of CHF treatment will likely feature greater personalization through precision medicine and AI-driven insights into behavior, genetics, and metabolic function. Wearables and remote monitoring tools will allow continuous feedback loops, making lifestyle adjustments more responsive and data-driven. Medical professionals may begin prescribing digital therapeutics—apps or programs validated through clinical trials—that coach users through CHF lifestyle changes in real time. We may also see wider adoption of integrative cardiac clinics that blend cardiology with nutrition, movement therapy, and psychological support under one roof. This future signals a shift away from reactive care and toward proactive, lifestyle-centered models of health for those with congestive heart failure.
Conclusion: Lifestyle as the Engine of Endurance in Heart Failure
Living with congestive heart failure does not mean giving up on strength, vitality, or performance. Instead, it presents an opportunity to build a new foundation for endurance—one rooted in daily choices that support the heart, muscles, mind, and spirit. From adopting a heart-healthy diet and maintaining a consistent exercise routine to managing stress and improving sleep, these CHF lifestyle changes are powerful tools that enhance not just life span, but health span.
When approached with knowledge, guidance, and dedication, these changes offer real, measurable improvements in how individuals with CHF feel and function. They restore confidence, improve energy, and unlock the potential to move, live, and thrive with purpose. For those ready to embrace a healthier path, the journey begins not with perfection, but with progress—and every smart step forward becomes a part of the endurance-building story.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Home Remedies: Lifestyle changes can help your heart health
Lifestyle Changes for Cardiomyopathy & Heart Failure
Congestive Heart Failure: Prevention, Treatment and Research

