Understanding the Intricate Connection Between Hormones and Hunger
Hunger is far more than a simple signal from an empty stomach; it is a complex physiological process deeply regulated by a network of hormones. These hormones operate in concert to maintain energy balance, regulate food intake, and ensure our bodies receive the nutrients they need. At the heart of this process lies a delicate dance between hormones such as ghrelin, leptin, insulin, and peptide YY, each with distinct roles in managing appetite and satiety. The interplay between hormones and hunger not only determines when we feel the urge to eat but also how much and what we crave.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
In today’s fast-paced environment, many individuals struggle with constant hunger, emotional eating, or difficulty recognizing fullness. Understanding what hormones make a person feel hungry—and how those signals can be influenced—is critical for anyone aiming to support a healthier lifestyle through mindful eating. Scientific research has increasingly turned its attention to the hormonal cues that drive appetite, revealing valuable insights into how we can work with our bodies rather than against them.
This article explores the biological mechanisms behind hunger, with a spotlight on ghrelin—the so-called “hunger hormone”—and offers actionable strategies to naturally modulate these hormonal signals. By delving into how to turn off hunger hormones using evidence-based approaches, readers can gain practical tools to better manage appetite, make informed dietary decisions, and align their eating habits with their wellness goals.
What Hormones Make a Person Feel Hungry? A Deeper Look at Appetite Regulation
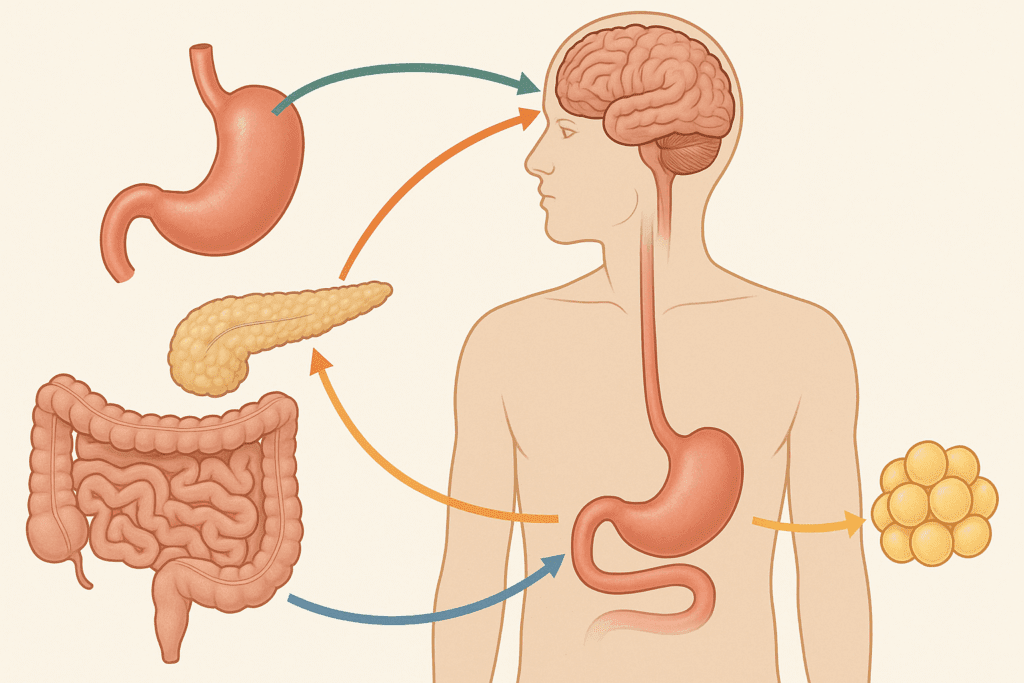
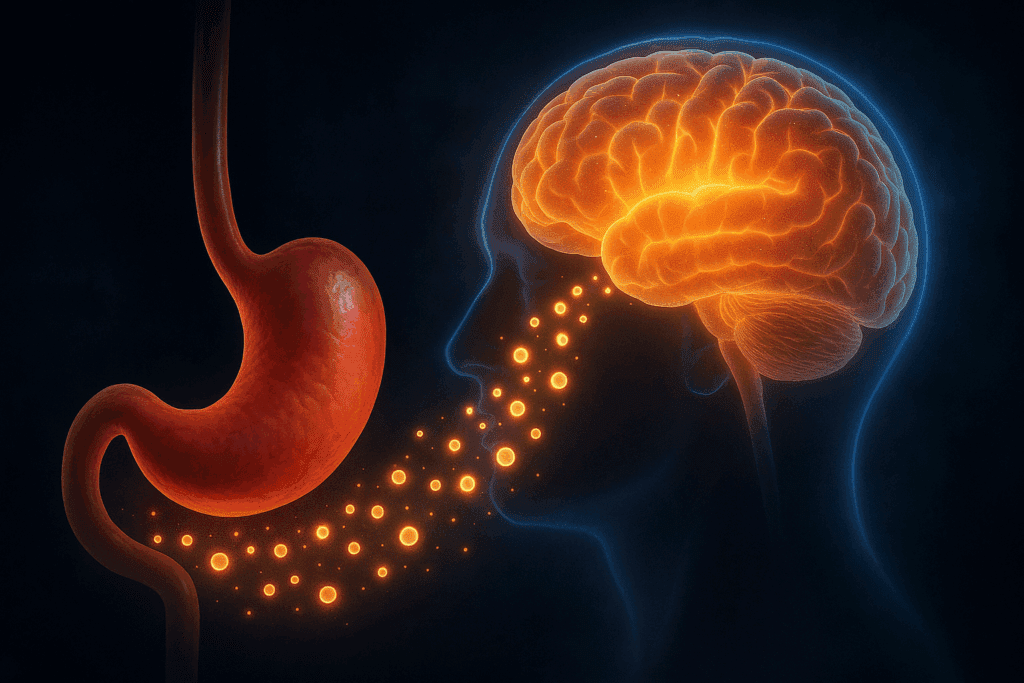
Hunger arises from a complex signaling system involving multiple hormones that communicate between the gut, brain, and other organs. Among the key players, ghrelin is perhaps the most recognized for its direct impact on stimulating appetite. Produced primarily in the stomach, ghrelin levels rise before meals and fall after eating, acting as a powerful cue for the brain to initiate food-seeking behavior. Ghrelin binds to receptors in the hypothalamus—the brain’s appetite control center—triggering sensations of hunger and increasing motivation to eat.
In contrast, leptin—produced by fat cells—acts as a satiety hormone that suppresses appetite when the body has enough energy stored. Low levels of leptin are associated with increased hunger and reduced energy expenditure, while high levels should, in theory, signal fullness. However, in individuals with obesity, leptin resistance may impair this feedback loop, making appetite regulation more challenging.
Other hormones involved in hunger include insulin, which also plays a role in satiety by facilitating glucose uptake and signaling energy availability, and peptide YY (PYY), a hormone secreted by the small intestine that promotes feelings of fullness after meals. Each hormone contributes to a finely tuned system that, when functioning properly, maintains a healthy balance between energy intake and expenditure.
However, this hormonal balance can be disrupted by various factors including chronic stress, poor sleep, ultra-processed diets, and metabolic conditions. These disruptions may lead to an overproduction of hunger-promoting hormones or diminished sensitivity to satiety signals, which can perpetuate overeating and weight gain. For this reason, identifying what hormones make a person feel hungry and understanding how to regulate them is vital for long-term health and sustainable dietary habits.
What Is Ghrelin Hormone and Why Is It Called the “Hunger Hormone”?
Ghrelin is a peptide hormone primarily secreted by the stomach and, to a lesser extent, by other tissues including the pancreas and brain. Its principal function is to stimulate appetite, earning it the nickname “the hunger hormone.” Ghrelin is unique in that its levels increase significantly before meals and drop sharply after eating, indicating its role in signaling meal initiation. But what does ghrelin do beyond simply making us feel hungry?
The answer lies in its multifaceted influence on the body. Ghrelin not only prompts the hypothalamus to initiate feeding behaviors but also promotes fat storage, regulates glucose metabolism, and may even affect mood and cognitive function. Interestingly, ghrelin also interacts with the brain’s reward system, influencing cravings and emotional eating by making high-calorie, palatable foods more appealing. This interaction underscores why hunger can be both a physiological and psychological experience.
In individuals who are fasting, dieting, or undergoing caloric restriction, ghrelin levels tend to increase, intensifying hunger and potentially making it more difficult to stick to a reduced-calorie diet. This natural feedback mechanism is designed to preserve energy and prevent starvation, but in modern times, it can complicate efforts to lose weight. Elevated ghrelin levels have also been linked to sleep deprivation and stress, two conditions that often co-occur with increased food intake and weight gain.
Understanding what ghrelin is and what ghrelin does is essential for those seeking to manage appetite more effectively. Since ghrelin acts as a powerful signal to eat, learning strategies to modulate its levels can play a crucial role in supporting mindful eating, weight management, and overall health.

How to Turn Off Hunger Hormones Naturally: Lifestyle and Nutrition Strategies
While we cannot eliminate hunger hormones entirely—nor should we—there are effective, evidence-based methods to regulate their activity and promote a more balanced appetite. Learning how to turn off hunger hormones naturally begins with an integrative approach that addresses diet, sleep, stress, and physical activity. These lifestyle factors profoundly influence the hormonal environment that governs hunger and satiety.
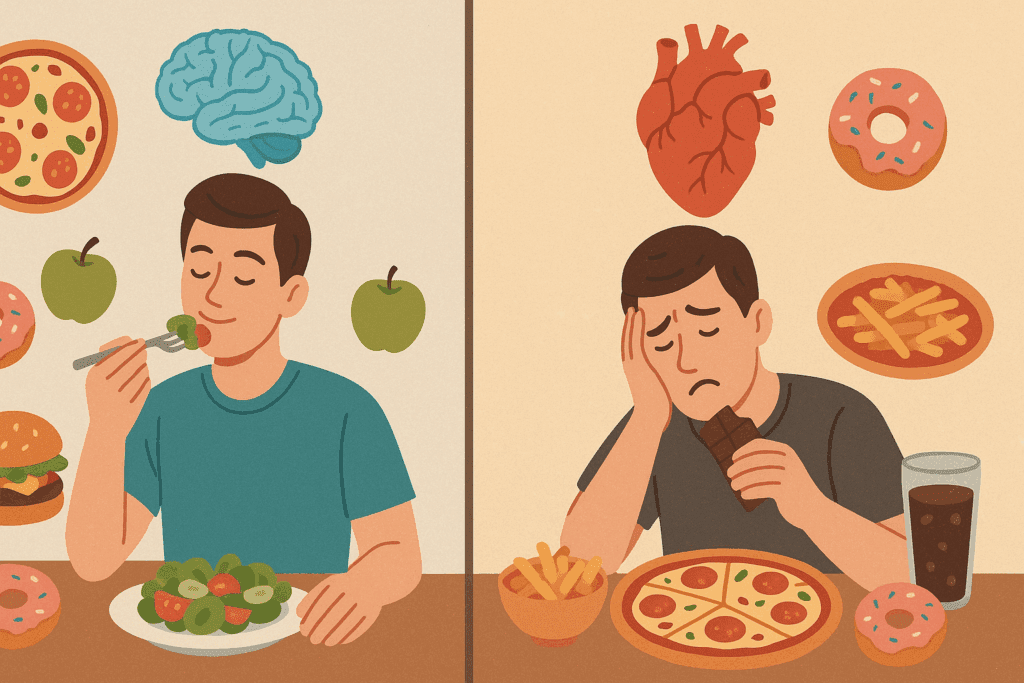
Diet plays a foundational role in hunger hormone regulation. Meals rich in protein, fiber, and healthy fats have been shown to suppress ghrelin more effectively than those high in refined carbohydrates or sugars. For instance, high-protein breakfasts can lead to prolonged satiety throughout the day, while dietary fiber slows digestion and promotes the release of peptide YY. Avoiding ultra-processed foods, which may disrupt hormonal signals and promote overeating, is also key to supporting appetite balance.
Sleep quality is another crucial factor. Inadequate sleep is associated with increased ghrelin production and reduced leptin levels, creating a hormonal profile that encourages overeating. Ensuring seven to nine hours of restorative sleep per night can help rebalance these hormones and reduce cravings. Moreover, establishing consistent sleep-wake cycles supports circadian rhythms, which in turn affect the timing and intensity of hunger cues.
Chronic stress triggers the release of cortisol, a hormone that not only increases appetite but also enhances the rewarding properties of food. Mind-body practices such as mindfulness meditation, yoga, and deep breathing exercises can help lower stress and modulate cortisol levels. These techniques not only support emotional regulation but may also reduce the urge for stress-related eating, contributing to more mindful food choices.
Physical activity also plays a role in modulating hunger hormones. Regular aerobic and resistance training have been shown to reduce fasting ghrelin levels and increase sensitivity to satiety signals such as leptin and peptide YY. In addition to helping with weight management, exercise improves mood, boosts metabolism, and enhances overall hormonal function. Together, these lifestyle interventions provide a comprehensive framework for those wondering how to turn off hunger hormones and foster a healthier relationship with food.
The Role of Emotional and Cognitive Factors in Perceived Hunger
Hunger is not merely a physical sensation—it is also shaped by psychological and emotional states. Many people experience what is known as “hedonic hunger,” a craving for food driven by pleasure or emotion rather than energy needs. Emotional eating, food-related habits, and conditioned responses to stress or boredom can all override true physiological hunger cues, leading to a disconnect between hormone signals and actual eating behavior.
The brain’s reward centers, particularly the mesolimbic dopamine system, respond strongly to palatable foods, reinforcing the habit of eating in response to emotions rather than hunger. Ghrelin, interestingly, enhances the reward value of food, which means that during periods of elevated ghrelin, individuals may be more susceptible to emotional or impulsive eating. This biological mechanism may explain why dieting, stress, and sleep deprivation often lead to increased consumption of high-fat or sugary foods.
Cognitive factors such as attention, perception, and memory also play a role in hunger. For example, distractions during meals—such as watching television or scrolling through a phone—can interfere with the brain’s ability to register fullness, potentially leading to overeating. Similarly, individuals who practice mindful eating—paying close attention to hunger and satiety signals—tend to consume fewer calories and report greater satisfaction with meals.
Understanding the interplay between hormones and hunger requires addressing these emotional and cognitive influences. Incorporating mindfulness techniques, cognitive behavioral strategies, and intuitive eating practices can enhance awareness of true hunger cues and reduce reliance on food for emotional comfort. These psychological tools, combined with hormonal regulation, offer a powerful approach to cultivating a healthier relationship with eating.
Hormones and Hunger in the Context of Obesity and Metabolic Health
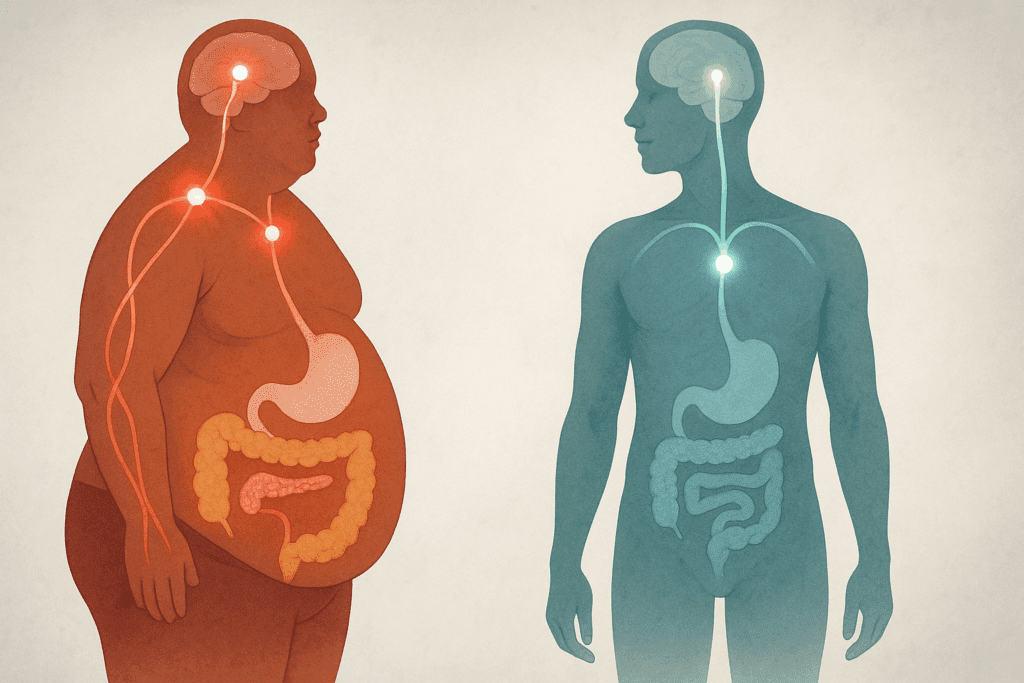
Obesity is often accompanied by significant hormonal dysregulation, particularly in the pathways that govern hunger and satiety. Individuals with obesity frequently exhibit elevated ghrelin levels and resistance to leptin’s satiety signals, creating a hormonal environment that perpetuates increased food intake. This imbalance can create a cycle in which the body continues to signal hunger even when energy needs are met, complicating weight management efforts.
Insulin resistance, a hallmark of metabolic syndrome, further exacerbates this issue by impairing glucose uptake and contributing to erratic blood sugar levels. Fluctuating glucose levels can mimic hunger symptoms, triggering additional food intake. Moreover, inflammation and changes in gut microbiota—both common in obesity—may alter the secretion and sensitivity of appetite-regulating hormones.
Lifestyle interventions aimed at improving metabolic health often focus on restoring hormonal balance. Weight loss itself can improve leptin sensitivity and reduce ghrelin secretion over time, though the body may initially resist these changes by increasing hunger signals. This adaptive response is part of the body’s effort to maintain homeostasis, but it can be overcome through sustained, health-supportive behaviors.
Medical strategies, including bariatric surgery, have also shown significant effects on hunger hormones. Procedures like gastric bypass have been associated with decreased ghrelin levels and enhanced release of satiety hormones such as GLP-1 and PYY. These hormonal shifts contribute to reduced appetite and sustained weight loss in many patients, illustrating the profound impact of hormonal regulation on eating behavior and metabolic health.
Understanding how hormones and hunger are connected in the context of obesity can inform more effective and compassionate approaches to treatment. Rather than viewing weight gain solely as a matter of willpower, recognizing the biological drivers of appetite empowers individuals and healthcare providers to implement targeted, science-based strategies for long-term success.
Frequently Asked Questions: Hormones and Hunger
1. Can stress cause long-term disruptions in hunger hormones, and how can this be addressed naturally? Yes, chronic stress can significantly alter the balance between hormones and hunger. Elevated cortisol levels, triggered by ongoing stress, may increase ghrelin secretion and desensitize the body’s satiety signals over time. This can create a persistent sensation of hunger, even when caloric needs are met. What’s particularly concerning is that this hormonal disruption can lead to long-term weight gain and increased risk of metabolic disorders. Learning how to turn off hunger hormones in this context often involves stress-reduction techniques like breathwork, guided meditation, or establishing a consistent sleep schedule, all of which help recalibrate the hormonal response to stress and food intake.
2. How does intermittent fasting affect ghrelin and other hunger-related hormones? Intermittent fasting introduces cycles of eating and fasting that influence what hormones make a person feel hungry, especially ghrelin. Initially, ghrelin levels may spike during fasting windows, increasing hunger cues. However, research shows that with consistent practice, the body begins to adapt, and ghrelin peaks may become less intense and more predictable. This shift allows individuals to feel more in control of hunger patterns. Understanding what ghrelin does in the context of fasting can help tailor eating windows that align with personal energy needs, offering a practical way to reset hunger hormone rhythms without extreme restriction.
3. Are there medications that target hunger hormones directly? Yes, several emerging therapies aim to modulate hormones and hunger to support appetite control and weight management. Some medications mimic hormones like GLP-1 or reduce ghrelin levels, helping suppress appetite. For example, GLP-1 receptor agonists not only promote fullness but also delay gastric emptying, providing a prolonged feeling of satiety. While these drugs can be effective, they are typically prescribed in cases of obesity or type 2 diabetes and require careful medical supervision. Exploring what hormones make a person feel hungry helps inform whether pharmaceutical intervention is appropriate, especially when paired with natural methods for learning how to turn off hunger hormones.
4. Can gut health influence hunger hormones and overall appetite regulation? Absolutely—gut microbiota play a critical role in how hormones and hunger interact. A healthy and diverse gut flora supports the production of short-chain fatty acids that stimulate hormones like peptide YY and GLP-1, which help reduce appetite. Conversely, dysbiosis—an imbalance in gut bacteria—can impair these signaling pathways and increase inflammation, which may lead to elevated ghrelin levels and heightened hunger. Supporting gut health through probiotic-rich foods, fermented products, and a fiber-rich diet can improve hormonal communication between the gut and brain. This approach offers another practical avenue for addressing what is ghrelin hormone function and how it fits into the broader picture of appetite regulation.
5. Why do some people still feel hungry after eating large meals? Feeling hungry after a large meal may be less about caloric intake and more about how specific nutrients affect hormones and hunger. Meals high in refined carbohydrates or low in protein and fiber can cause rapid blood sugar spikes followed by crashes, leading to increased ghrelin levels shortly after eating. Additionally, emotional or habitual eating patterns can override physiological cues, making it difficult to distinguish true hunger from conditioned responses. Understanding what hormones makes a person feel hungry can help individuals identify whether their hunger is biologically driven or psychologically conditioned. To naturally address this issue, choosing meals with balanced macronutrients and practicing mindful eating can help recalibrate hunger perception.
6. Are there gender differences in how hunger hormones operate? Yes, biological sex can influence how hormones and hunger interact. Research suggests that women may experience greater sensitivity to ghrelin fluctuations, especially during different phases of the menstrual cycle. For instance, ghrelin levels often increase during the luteal phase, contributing to heightened hunger and cravings. Hormonal birth control can also influence appetite by altering estrogen and progesterone levels, which may interact with ghrelin and leptin. Recognizing what ghrelin does in the context of female physiology offers deeper insight into how to turn off hunger hormones naturally, such as by tailoring nutrition and exercise strategies around hormonal fluctuations.
7. Can exercise timing impact hunger hormone regulation? The timing and type of exercise can significantly affect what hormones make a person feel hungry. Aerobic exercise performed in the morning may reduce ghrelin levels temporarily while boosting peptide YY, helping to suppress appetite for several hours post-workout. Resistance training, on the other hand, has been associated with improved insulin sensitivity and long-term hormonal balance. Understanding what is ghrelin hormone behavior in response to physical activity allows individuals to strategically schedule workouts to align with their appetite patterns. Exercising before meals may also enhance the natural rhythm of hunger hormone release and support mindful eating.
8. How do artificial sweeteners impact hunger hormones? Artificial sweeteners can disrupt the normal signaling processes involved in hormones and hunger, even though they contain little to no calories. Some studies suggest that these sweeteners may trick the brain into expecting caloric intake, potentially increasing ghrelin levels and reinforcing cravings. Over time, this may impair the body’s ability to regulate appetite accurately, especially when consumed frequently. If someone is learning how to turn off hunger hormones, replacing artificial sweeteners with natural alternatives or reducing overall sweet taste exposure may support better hormonal balance. Understanding what ghrelin does in response to both real and perceived sugar intake is crucial for managing long-term eating behavior.
9. Is it possible to retrain hunger hormones after years of overeating? Yes, the hormonal system involved in appetite regulation is highly adaptive, and with time, it can respond positively to behavioral changes. For individuals who have experienced chronic overeating, ghrelin levels may remain elevated and satiety hormones may be downregulated. However, by consistently implementing nutrient-dense meals, sleep hygiene, stress management, and physical activity, the body can gradually restore hormonal sensitivity. Understanding what hormones makes a person feel hungry can empower individuals to differentiate between temporary withdrawal cues and true hunger signals. Retraining the body in this way requires patience and consistency but offers meaningful long-term benefits.
10. Are there specific foods that help reduce ghrelin more effectively than others? Yes, certain foods are particularly effective at suppressing ghrelin and supporting overall appetite regulation. High-protein foods such as eggs, Greek yogurt, and legumes have been shown to reduce ghrelin levels for extended periods. Additionally, omega-3 fatty acids and polyphenol-rich foods like berries and green tea may indirectly affect what ghrelin does by reducing inflammation and supporting insulin sensitivity. Including these items in daily meals provides a practical approach for those looking to understand what is ghrelin hormone behavior and how to turn off hunger hormones naturally. These food choices offer a sustainable way to align nutrition with the body’s hormonal appetite signals.
Conclusion: Managing Hormones and Hunger for Sustainable Health and Wellness
Navigating the complex relationship between hormones and hunger is key to achieving lasting health and well-being. By understanding what hormones make a person feel hungry—particularly the central role played by ghrelin—and learning how to turn off hunger hormones naturally, individuals can take proactive steps toward more mindful, balanced eating. Rather than battling against hunger, aligning with the body’s natural hormonal rhythms offers a sustainable path to wellness.
Strategies such as prioritizing sleep, managing stress, choosing nutrient-dense foods, and engaging in regular physical activity can all contribute to hormonal harmony and appetite control. Moreover, acknowledging the emotional and psychological dimensions of hunger allows for a more holistic approach that addresses both the mind and body. This comprehensive framework supports not only weight management but also emotional resilience and long-term metabolic health.
The science of hunger hormones continues to evolve, offering new insights into how we can harness our biology to support better nutrition and lifestyle choices. For anyone looking to optimize their health, understanding what ghrelin does and how hormonal signals shape eating behavior is a valuable foundation. Ultimately, mindful engagement with our hunger—guided by evidence-based strategies—can lead to more empowered and healthful living.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.

