In the world of endurance training and performance optimization, cardiovascular health is often equated with blood pressure readings. A normal blood pressure score is generally celebrated as a green light for intense physical exertion, while elevated numbers are commonly seen as a red flag. But the reality of cardiovascular health is far more nuanced. A growing body of research is beginning to explore an important, and often misunderstood, question: Can you have heart problems with good blood pressure?
This question holds profound implications not just for the general population, but particularly for athletes, fitness enthusiasts, and high performers who place heavy demands on their cardiovascular systems. Good blood pressure is undoubtedly beneficial, but it is not a foolproof indicator of optimal heart function or immunity from cardiovascular risk. In fact, focusing solely on blood pressure may cause some individuals to overlook other critical signs that could indicate underlying cardiac issues. Understanding the intricate interplay between blood pressure and heart disease is essential for anyone seeking to protect their endurance capacity and long-term health.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice

Why Blood Pressure Isn’t the Whole Story
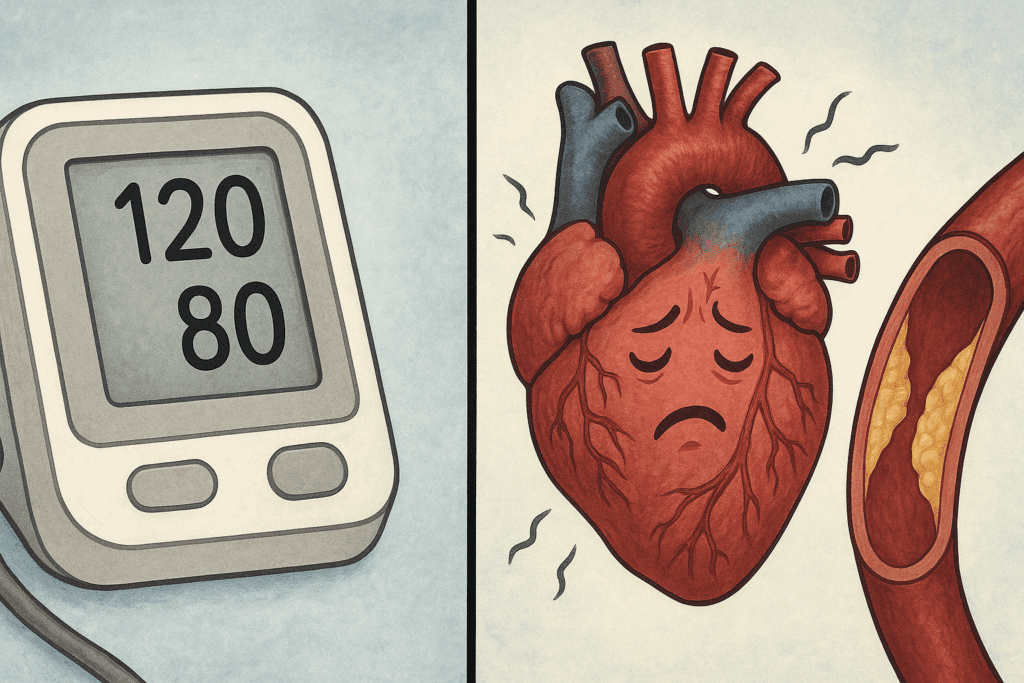
Blood pressure readings have long served as a convenient shorthand for cardiovascular health. A typical reading under 120/80 mmHg is generally viewed as ideal, suggesting efficient circulation and minimal arterial stress. However, even in the absence of hypertension, individuals can still develop a range of heart problems. That’s why the question, can you have heart problems with good blood pressure, is gaining attention in both clinical circles and among the general public.
Research shows that conditions such as coronary artery disease, arrhythmias, heart valve disorders, and even heart failure can develop in individuals with perfectly normal blood pressure. One reason for this is that blood pressure is just one facet of cardiovascular health. While it reflects the force of blood pushing against artery walls, it doesn’t capture the full picture—especially in terms of arterial plaque buildup, heart muscle efficiency, or electrical signaling in the heart.
Endurance athletes, in particular, may present with low or normal blood pressure while still developing issues such as athlete’s heart or myocardial fibrosis. These conditions might not trigger any warning signs on a standard blood pressure monitor, yet they can significantly impair performance and elevate long-term risk. Thus, relying on blood pressure alone to determine heart health can lead to a false sense of security.
Understanding the Complex Relationship Between Blood Pressure and Heart Disease
To appreciate the limitations of normal blood pressure as a standalone metric, it’s helpful to explore the broader context of blood pressure and heart disease. Elevated blood pressure, or hypertension, is undeniably one of the strongest predictors of cardiovascular disease. Studies have consistently shown that it increases one’s risk of heart disease, high blood pressure being a well-established contributor to arterial damage, left ventricular hypertrophy, and atherosclerosis.
But what if an individual has optimal blood pressure yet still exhibits signs of cardiovascular dysfunction? This is where the nuance emerges. Factors such as genetics, systemic inflammation, lipid profiles, physical activity levels, and metabolic conditions can all play significant roles in cardiovascular risk. In some cases, the heart may be overcompensating for other deficiencies or stressors, functioning inefficiently even when the blood pressure is in the normal range.
It’s also important to understand that blood pressure varies throughout the day and can be influenced by acute stress, hydration status, and even breathing patterns. Ambulatory blood pressure monitoring, which tracks readings over 24 hours, often provides a more accurate picture than isolated clinic measurements. Even then, some cases of cardiovascular dysfunction evade detection because they are driven by non-hemodynamic factors.
Can You Have Heart Disease and Normal Blood Pressure?
The answer is a resounding yes. You can, indeed, have heart disease and normal blood pressure. Cardiomyopathies, arrhythmias, and structural abnormalities like mitral valve prolapse may not alter your blood pressure readings in any obvious way. Yet these conditions can have a profound impact on both cardiac performance and endurance.
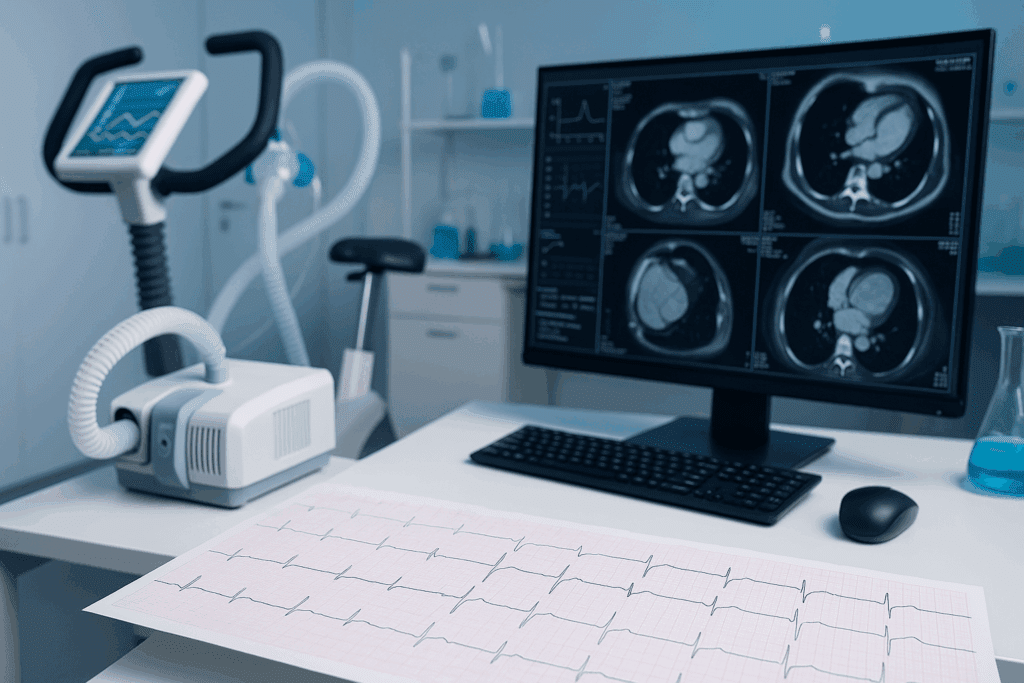
In fact, this reality underscores the importance of comprehensive cardiovascular screening—particularly for individuals engaged in high levels of physical activity. Stress testing, echocardiograms, electrocardiograms (EKGs), and even cardiac MRI can uncover underlying issues that a simple blood pressure cuff cannot detect. These tests offer deeper insights into cardiac function, valve integrity, and the presence of scar tissue or inflammation within the heart muscle.
Moreover, it is not uncommon for younger, seemingly healthy individuals to be diagnosed with early-stage heart disease despite having textbook blood pressure. This disconnect emphasizes the need for a more holistic view of cardiovascular health—one that moves beyond a singular focus on blood pressure and incorporates lifestyle, family history, and performance metrics.
Hidden Risk Factors That May Go Unnoticed
When asking, can you have heart problems with good blood pressure, it becomes crucial to examine the subtler risk factors that might not manifest in traditional screenings. One major factor is endothelial dysfunction, a condition in which the lining of the blood vessels fails to function normally. This can occur even in individuals with good blood pressure and may lead to impaired blood flow and increased risk of clot formation.
Similarly, chronic inflammation and oxidative stress can quietly damage cardiovascular tissues without necessarily elevating blood pressure. High-sensitivity C-reactive protein (hs-CRP) tests and other inflammatory markers can help detect these risks early on. Metabolic syndrome, insulin resistance, and elevated lipoprotein(a) levels are additional factors that can compromise heart health despite normal blood pressure.
Another key consideration is autonomic imbalance. The autonomic nervous system governs involuntary functions like heart rate and blood vessel constriction. In cases of overtraining or chronic stress, the sympathetic nervous system can dominate, impairing heart rate variability and increasing susceptibility to arrhythmias—even in the presence of stable blood pressure readings.

When Normal Blood Pressure Masks High Performance Risk
For athletes and high performers, the implications of hidden cardiac risks are particularly sobering. In sports where endurance is prized, the cardiovascular system is pushed to its limits. Many athletes pride themselves on having low resting heart rates and ideal blood pressure, which are often considered markers of superior fitness. However, when asking whether you can have heart disease and normal blood pressure, we must consider how training adaptations might camouflage early warning signs.
Athlete’s heart, characterized by an enlarged left ventricle, can sometimes be difficult to distinguish from early-stage cardiomyopathy. Likewise, endurance athletes may develop scarring in the heart muscle due to chronic volume overload, which can set the stage for arrhythmias or even sudden cardiac events. These conditions often fly under the radar in individuals whose blood pressure remains well within the normal range.
Moreover, the obsession with peak performance can sometimes lead to overtraining syndrome, a state in which physiological stress outpaces recovery. This state often coexists with hormonal dysregulation, reduced heart rate variability, and altered autonomic function—all of which are rarely detected through standard blood pressure measurements. Therefore, a performance-focused approach to cardiovascular screening is essential for athletes and active individuals.
Is High Blood Pressure Considered Heart Disease?
This question reveals another area of common confusion. Technically, high blood pressure itself is not considered heart disease, but it significantly increases one’s risk of heart disease. High blood pressure strains the heart and arteries, causing micro-damage that accumulates over time. This can lead to atherosclerosis, aneurysms, and heart failure if left unchecked.
Thus, while high blood pressure is a risk factor rather than a diagnosis of heart disease, its impact cannot be overstated. More importantly, even when blood pressure is normal, the absence of overt hypertension does not mean the heart is in perfect shape. For this reason, performance-conscious individuals must ask more nuanced questions than simply, is high blood pressure considered heart disease. They must also consider whether their cardiovascular systems are functioning at peak efficiency—or whether unseen vulnerabilities are lurking beneath the surface.
How to Evaluate Cardiovascular Risk Beyond Blood Pressure
A proactive approach to cardiovascular health requires a toolkit that extends beyond the sphygmomanometer. Resting and exercise EKGs, stress echocardiograms, VO2 max testing, and even coronary artery calcium scans can provide valuable insights into cardiovascular function and disease risk. These tests assess aspects of heart health that blood pressure cannot measure—such as the elasticity of blood vessels, the efficiency of cardiac output, and the presence of arterial calcification.
In addition to diagnostic testing, lifestyle assessments play a crucial role. Nutritional habits, sleep quality, psychological stress levels, and recovery routines can all influence cardiovascular health. Integrating heart rate variability (HRV) tracking into one’s training regimen can help gauge autonomic balance and recovery status, providing an early warning system that complements traditional metrics like blood pressure.
For individuals with a family history of heart disease, genetic testing may offer further insights. Certain gene variants can predispose individuals to cardiomyopathies, lipid disorders, and clotting abnormalities—conditions that may not affect blood pressure but can have severe implications for heart health. When interpreted alongside blood pressure and other biometric data, genetic testing can be a powerful tool for personalized prevention.

Implications for Training, Recovery, and Long-Term Performance
If we accept that you can have heart disease and normal blood pressure, the implications for training and performance strategies are profound. Athletes, coaches, and healthcare providers must move beyond simplistic metrics and embrace a more integrated model of cardiovascular monitoring. This includes evaluating endurance capacity not only through output measures like time trials or power zones but also through recovery indices, HRV trends, and cardiac-specific assessments.
Training programs should be individualized, taking into account both performance goals and physiological stress markers. Recovery should be prioritized as much as exertion, with structured deload weeks, adequate sleep, and nutrition tailored to support cardiac resilience. Supplements such as omega-3 fatty acids, magnesium, and coenzyme Q10 may also support mitochondrial and cardiovascular health, although these should be used under medical supervision.
Ultimately, peak performance and heart health are not mutually exclusive, but they must be managed in tandem. By acknowledging that normal blood pressure does not guarantee immunity from cardiac concerns, endurance athletes can take proactive steps to optimize both short-term gains and long-term well-being.
Frequently Asked Questions: Can You Have Heart Problems with Good Blood Pressure?
1. Can someone experience exercise-induced heart complications even with normal blood pressure readings? Absolutely. Even in the absence of elevated blood pressure, intense physical exertion can unmask underlying cardiac issues like arrhythmias or left ventricular hypertrophy. These issues often remain hidden during routine health checks but may present during periods of peak cardiovascular stress. The reality is that you can have heart problems with good blood pressure, particularly if there are genetic predispositions or structural abnormalities. Blood pressure and heart disease are related, but blood pressure alone doesn’t capture performance-induced vulnerabilities. Advanced diagnostic tools like VO2 max testing and stress echocardiography are often required to detect these concerns in athletic individuals.
2. How do hidden inflammatory conditions contribute to heart disease despite normal blood pressure? Chronic inflammation is a silent but potent contributor to cardiovascular disease. It can damage blood vessels and promote plaque buildup, even when blood pressure is well-managed. Many people assume they’re in the clear because their numbers fall within the normal range, yet inflammatory markers like C-reactive protein may be elevated. This scenario reinforces the concern that you can have heart disease and normal blood pressure while facing serious cardiovascular risk. These conditions may not raise immediate red flags during routine screenings, but they significantly elevate long-term vulnerability.
3. Are individuals with normal blood pressure but poor sleep quality at increased cardiac risk? Yes, poor sleep quality is a recognized but often underestimated cardiovascular risk factor. Sleep deprivation elevates sympathetic nervous system activity, which can lead to hormonal imbalances and increased arterial stiffness. Even if blood pressure readings remain normal during the day, nighttime disruptions may indicate hidden cardiac strain. This is another case where one can have heart problems with good blood pressure and not be aware of it until a more severe event occurs. Sleep studies and wearable heart rate variability monitors can be valuable in identifying risks early.
4. Can emotional stress affect heart function without raising blood pressure? Emotional stress can lead to conditions such as Takotsubo cardiomyopathy, also known as stress-induced heart syndrome. This temporary weakening of the heart muscle often occurs without concurrent hypertension. The dissociation between emotional health and vascular readings underscores how you can have heart disease and normal blood pressure at the same time. Chronic stress also alters cortisol and adrenaline levels, which over time damages blood vessels, regardless of visible blood pressure changes. Incorporating mental health assessments into cardiovascular care plans is crucial.
5. Why do some people with good blood pressure still suffer from poor cardiac output? Cardiac output refers to the amount of blood the heart pumps per minute, and it is not always directly correlated with blood pressure. Some individuals maintain normal vascular resistance and pressure, yet have weakened heart muscle or dysfunctional valves that reduce efficiency. This functional decline is a lesser-known but serious indicator that increases one’s risk of heart disease—high blood pressure not always being the cause. Recognizing such impairments requires more in-depth analysis, like echocardiography or cardiac MRI. Again, this proves that blood pressure and heart disease are not always synchronized.
6. What role does cardiovascular genetics play in individuals with normal blood pressure? Genetic predispositions can significantly increase cardiovascular risk even when blood pressure is within the normal range. Certain inherited conditions, such as hypertrophic cardiomyopathy or familial hypercholesterolemia, may manifest without affecting blood pressure initially. This is particularly important when evaluating why you can have heart problems with good blood pressure despite leading an otherwise healthy lifestyle. Genetic screening may uncover silent risk factors that routine checkups miss. It emphasizes the importance of personalized risk assessment in cardiovascular prevention.
7. Can endurance athletes develop heart disease despite optimal blood pressure readings? Yes, and it happens more often than many realize. Endurance athletes often exhibit bradycardia and textbook blood pressure levels, yet are not immune to myocardial scarring, arrhythmias, or athlete’s heart syndrome. The paradox is that the very training that boosts endurance may introduce micro-injuries or remodeling that mimics early heart disease. This is one more reason why the question, can you have heart disease and normal blood pressure, deserves deeper attention in sports medicine. Routine screening should go beyond numbers to evaluate structural and electrical health of the heart.
8. How does long-term high blood pressure affect people even after their blood pressure returns to normal? Prolonged exposure to high blood pressure can cause lasting damage, even if later normalized through medication or lifestyle changes. The cumulative effects on arteries, kidneys, and the heart do not simply reverse when readings improve. This means that having a history of high blood pressure increases one’s risk of heart disease—high blood pressure being a lingering legacy even if not currently present. This delayed risk can manifest as arterial stiffness, diastolic dysfunction, or silent ischemia. Continued surveillance and secondary prevention strategies are critical.
9. Are wearable devices effective in detecting hidden cardiac risk when blood pressure appears normal? Many modern wearable technologies can offer insights that traditional blood pressure readings cannot. Devices that track heart rate variability, oxygen saturation, and even EKG-like signals are now helping to fill the diagnostic gap. For example, fluctuations in HRV can indicate autonomic imbalance, a sign that may precede detectable blood pressure changes. In this context, the gap between blood pressure and heart disease can be better bridged with continuous data. While wearables are not replacements for clinical testing, they are useful adjuncts for early detection.
10. How should people with normal blood pressure but strong family history of heart disease approach screening? Individuals with a family history of cardiac events should not rely on blood pressure readings alone. In fact, such cases reinforce that you can have heart problems with good blood pressure and still be at considerable risk. Early imaging, stress testing, coronary artery calcium scoring, and lab tests for cholesterol and inflammation are all advisable. This is especially true if symptoms like fatigue, palpitations, or chest discomfort occur—even subtly. Proactive screening can uncover early-stage disease and help offset what otherwise might be a missed opportunity for prevention.
Conclusion: Why Good Blood Pressure Alone Isn’t Enough to Protect Your Heart
In the pursuit of endurance and performance, relying solely on blood pressure as a measure of cardiovascular health can be dangerously misleading. The notion that normal readings equate to a healthy heart is increasingly challenged by evidence showing that you can, in fact, have heart problems with good blood pressure. From athlete’s heart to autonomic imbalance, from metabolic factors to silent inflammatory conditions, numerous threats can compromise heart health without affecting blood pressure.
Equally important is understanding that while high blood pressure increases one’s risk of heart disease, high blood pressure is just one piece of a much larger puzzle. Asking whether high blood pressure is considered heart disease reveals the importance of language and precision in cardiovascular care. We must move beyond binary thinking and embrace a more nuanced approach—one that evaluates risk across multiple domains, from genetics and inflammation to performance metrics and recovery quality.
As the science of performance enhancement evolves, so must our understanding of what it means to be truly heart-healthy. For athletes and high performers, this means committing to comprehensive cardiovascular screening, personalized training, and continuous self-monitoring that goes far beyond the occasional blood pressure check. Only by integrating these layers of insight can we safeguard both endurance and long-term heart health.
So, the next time you—or your clients—ask, can you have heart disease and normal blood pressure, the answer should be clear. Yes, and it’s exactly why we need to expand our definition of cardiovascular fitness to include more than just a number on a monitor. True heart health is multifaceted, and it deserves an equally comprehensive approach.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.

