A New Look at EDNOS and Unspecified Eating Disorders
Eating disorders are often misunderstood, and one of the most commonly overlooked categories involves diagnoses that don’t quite fit traditional criteria. Known as “eating disorder not otherwise specified” or EDNOS, this term was widely used prior to updates made in the DSM-5, which have since reclassified and expanded diagnostic options. Still, many individuals find themselves in diagnostic gray areas. Whether referred to as EDNOS, eating disorder NOS, or unspecified eating disorder, these conditions remain real, serious, and deserving of attention.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
Despite the evolving terminology, the lived experience of those struggling with disordered eating patterns that don’t align neatly with anorexia nervosa, bulimia nervosa, or binge eating disorder DSM-5 criteria remains just as significant. The challenge for healthcare professionals and patients alike lies in addressing these complex and often fluid conditions. Fortunately, growing awareness and evolving diagnostic standards have begun to shift the focus toward more nuanced treatment pathways. This shift includes not only clinical interventions but also integrative approaches that emphasize nutrition, lifestyle changes, and supportive environments.
Understanding these disorders from a modern, multidimensional perspective is essential. Many individuals who fall under the classification of eating disorders not otherwise specified EDNOS may cycle through different symptoms over time. This variability underscores the importance of a flexible, holistic approach to treatment—one that considers mental health, nutritional support, physical well-being, and the social determinants of health. By viewing EDNOS and unspecified eating disorder diagnoses as valid and treatable, rather than as diagnostic leftovers, the health and wellness community can better serve those who might otherwise slip through the cracks.
DSM Changes and the Ongoing Relevance of EDNOS
With the publication of the DSM-5, major updates were made to the way eating disorders are diagnosed. Binge eating disorder, once often diagnosed under the umbrella of EDNOS, was given its own distinct diagnostic category. This adjustment reflected the growing body of research highlighting the unique psychological and physiological dimensions of what is now referred to as DSM-V binge eating disorder. Despite this shift, many individuals still experience symptoms that don’t meet full criteria for any one disorder and continue to be diagnosed with what is now known as an unspecified eating disorder.
The terminology transition from EDNOS to unspecified eating disorder has not eliminated diagnostic ambiguity. In practice, healthcare providers still encounter individuals with significant eating-related distress who do not meet the strict criteria for anorexia, bulimia, or binge eating disorder DSM-5. The persistence of such cases emphasizes the continued relevance of understanding and addressing EDNOS eating disorder diagnoses. Importantly, the label should not be perceived as a lesser form of illness. Instead, it indicates a need for personalized treatment strategies that adapt to the complexity of each case.
Furthermore, the cultural and environmental contexts in which eating disorders develop can shape how symptoms are expressed. For instance, disordered eating patterns driven by trauma, chronic stress, or inconsistent access to food may not align with existing diagnostic categories. This highlights the need for inclusive diagnostic models and the importance of a compassionate approach that acknowledges the full spectrum of disordered eating behavior. Such an approach is foundational for delivering effective, stigma-free care.

The Hidden Challenges of Diagnosing Eating Disorders Not Otherwise Specified
Diagnosing eating disorders not otherwise specified EDNOS is often fraught with challenges. Because the criteria are less defined, symptoms may be minimized or misinterpreted by both patients and healthcare providers. Individuals may not perceive themselves as “sick enough,” and medical professionals might overlook key behavioral or psychological indicators that suggest an underlying problem. This underdiagnosis can delay access to treatment and prolong suffering.
One key issue is that many people with EDNOS or an eating disorder not specified may present with mixed or fluctuating symptoms. For example, someone may restrict their food intake but not meet the weight criteria for anorexia, or they may binge without purging, leading to a misclassification. This makes accurate diagnosis highly dependent on detailed clinical assessment and ongoing observation over time. Practitioners must consider the broader context of the patient’s behavior, including emotional distress, compulsive thoughts, and functional impairment.
There is also a notable stigma surrounding these ambiguous diagnoses. Patients may internalize the notion that their struggles are not as serious as those with more defined disorders, which can undermine their willingness to seek help. The healthcare system, too, often prioritizes more visible or acute conditions, contributing to gaps in care. These challenges make it even more essential to build awareness around the legitimacy of EDNOS and unspecified eating disorders.
Addressing these challenges requires more than just clinical intervention; it also involves public education and systemic changes in how disordered eating is perceived and treated. Broader acceptance and understanding can help ensure individuals receive timely and appropriate care. Promoting visibility and inclusivity for those with eating disorder NOS diagnoses can foster a more compassionate healthcare environment that supports long-term recovery.
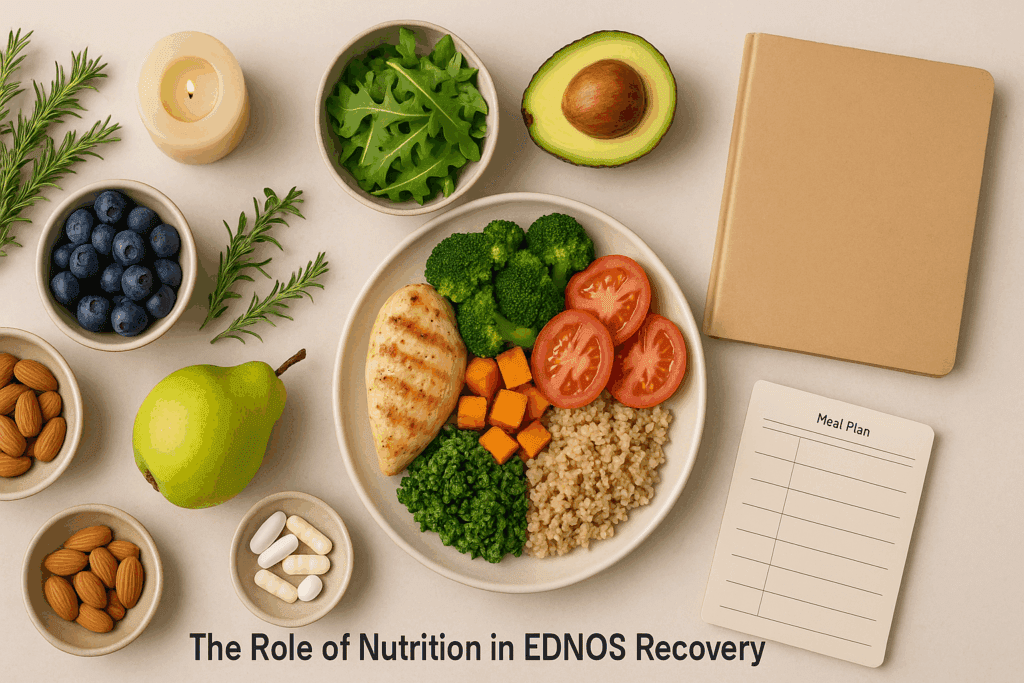
The Role of Nutrition in EDNOS Recovery
Nutrition plays a central role in healing from any eating disorder, and this is no less true for those diagnosed with an eating disorder not otherwise specified. Unlike traditional diet plans or restrictive regimens, nutritional rehabilitation for EDNOS focuses on re-establishing a healthy relationship with food, balancing macronutrient intake, and addressing specific deficiencies that may result from prolonged disordered eating patterns. A personalized, non-judgmental approach is essential in this process.
Malnutrition and nutrient imbalances are common among individuals with EDNOS, even if they do not appear underweight or exhibit overt signs of illness. These imbalances can exacerbate physical symptoms like fatigue, hormonal disruption, and digestive issues, while also impacting mental health. For instance, inadequate intake of omega-3 fatty acids, B vitamins, or iron can worsen mood disorders, cognitive function, and energy levels. Addressing these gaps through targeted nutritional support can significantly improve both physical and psychological outcomes.
Intuitive eating frameworks have gained traction in the recovery space for EDNOS eating disorder cases. This model encourages individuals to listen to internal hunger and fullness cues, reject diet culture, and prioritize body respect. Although not a substitute for clinical treatment, intuitive eating can be a valuable complement to therapy, particularly for individuals working to rebuild trust in their own bodies. This approach reinforces self-awareness, fosters empowerment, and helps dismantle the shame often associated with food.
Incorporating mindful eating practices is also beneficial. Slowing down during meals, savoring flavors, and recognizing emotional eating triggers can help individuals with an unspecified eating disorder reconnect with the eating experience in a positive way. These practices support not only physical nourishment but also emotional healing. Nutrition education delivered with empathy and free of judgment is a powerful tool for building resilience and supporting long-term recovery.
Lifestyle Changes That Promote Healing and Stability
In addition to nutritional interventions, lifestyle changes can make a meaningful difference in managing and recovering from EDNOS. Establishing consistent daily routines, prioritizing sleep hygiene, and reducing exposure to stressors are foundational aspects of healing. While these changes may seem simple, they often require intentional effort and support, particularly for individuals whose lives have been disrupted by disordered eating.
Physical activity, when approached with care, can also play a supportive role in recovery. The emphasis should not be on weight loss or performance but rather on joyful movement and reconnecting with one’s body. Activities such as yoga, walking, or swimming can help reduce anxiety, enhance body awareness, and foster a sense of competence. However, exercise should be carefully tailored to each individual’s needs and should not become a means of control or punishment.
Psychosocial support is equally critical. Building a recovery-oriented environment that includes supportive friends, family members, and professionals helps counteract the isolation that often accompanies eating disorders. Participating in group therapy or peer support networks can provide validation, encouragement, and a sense of belonging. These connections remind individuals that they are not alone and that healing is not only possible but also sustainable.
Mindfulness practices, including meditation and breathing techniques, can reduce compulsive behaviors and promote emotional regulation. These tools help individuals with eating disorders not otherwise specified develop healthier coping mechanisms, replacing harmful habits with constructive strategies. Integrating mindfulness into daily life builds resilience and cultivates self-compassion—an essential quality for those navigating the ups and downs of recovery.
Ultimately, lifestyle changes should be implemented gradually and compassionately, allowing space for setbacks without judgment. The goal is not perfection, but progress—creating a life that feels balanced, manageable, and fulfilling. When combined with medical and nutritional support, these changes contribute to a comprehensive recovery framework that honors the complexity of EDNOS and unspecified eating disorders.

Integrating Therapeutic Support for Lasting Recovery
Therapeutic interventions remain a cornerstone of effective treatment for EDNOS and related conditions. Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Acceptance and Commitment Therapy (ACT) are all evidence-based modalities that have shown promise for individuals with an eating disorder not specified. These approaches help individuals challenge unhelpful thoughts, regulate emotions, and develop healthier coping strategies.
CBT, in particular, is widely used to address disordered eating behaviors and the underlying beliefs that fuel them. For those diagnosed with binge eating disorder DSM-5 or who display patterns of emotional eating, CBT can help break the cycle of binge-restrict behaviors. It focuses on reshaping thought patterns, identifying triggers, and setting realistic goals for behavioral change. In cases of EDNOS, CBT can be adapted to fit a wide range of symptom profiles.
DBT is especially helpful for individuals who struggle with intense emotional fluctuations or co-occurring mental health conditions such as borderline personality disorder or PTSD. By teaching skills for distress tolerance, interpersonal effectiveness, and emotional regulation, DBT empowers individuals to navigate daily challenges more effectively. This is particularly beneficial for those with complex, overlapping symptoms that may fall under the category of unspecified eating disorder.
ACT, with its emphasis on values-based living, encourages individuals to accept uncomfortable thoughts and feelings without allowing them to dictate behavior. This can be transformative for those who have spent years feeling trapped by perfectionism, shame, or body dissatisfaction. When integrated into a broader treatment plan, ACT offers a pathway toward self-acceptance and intentional living.
Therapy is not a one-size-fits-all solution, and it works best when tailored to the unique needs and preferences of each person. Incorporating expressive therapies such as art, music, or movement can offer additional pathways to healing, particularly for those who struggle with verbal expression. The key is to create a flexible, responsive treatment plan that evolves over time as the individual’s needs change.
Frequently Asked Questions About EDNOS and Unspecified Eating Disorders
What is the difference between EDNOS and an unspecified eating disorder?
While these terms are often used interchangeably, there are subtle distinctions based on diagnostic frameworks. EDNOS eating disorder was a classification used primarily before the DSM-5 update, encompassing individuals with disordered eating symptoms that didn’t fit criteria for anorexia or bulimia. After the DSM-5 revision, the term “unspecified eating disorder” replaced EDNOS to capture similar diagnostic gaps. However, the core concern remains the same—these individuals experience serious eating-related distress that does not fully align with established categories. Understanding this evolution helps clarify why eating disorder NOS is still relevant in both clinical and recovery conversations today.
Why might someone not meet criteria for binge eating disorder DSM-5 but still need treatment?
DSM V binge eating disorder includes specific diagnostic thresholds, such as frequency of binge episodes and associated behaviors. However, many individuals may engage in binge-like eating without meeting all criteria, which often results in a diagnosis of an eating disorder not otherwise specified. These individuals still experience emotional distress, body dissatisfaction, and disruption in daily functioning. The absence of full diagnostic criteria does not mean the absence of suffering or risk. For this reason, even those who fall under eating disorder NOS deserve comprehensive, compassionate treatment.
Can eating disorders not otherwise specified EDNOS change over time into more defined disorders?
Yes, eating disorders not otherwise specified EDNOS can evolve over time as symptoms become more defined or meet new criteria. Someone initially diagnosed with an eating disorder not specified might later meet full criteria for binge eating disorder DSM-5 or another recognized eating disorder. This fluidity reflects how eating behaviors and psychological states can shift depending on life events, stress levels, or comorbid conditions. Early intervention is key because it may prevent progression or help stabilize emerging symptoms. It also underlines the importance of viewing EDNOS as a dynamic, not static, condition.
What role does culture play in how EDNOS and unspecified eating disorders are diagnosed?
Cultural context plays a profound role in eating disorder diagnosis. Behaviors that may be considered disordered in one culture might be normalized in another, leading to underdiagnosis or misclassification. This is particularly true for EDNOS eating disorder cases, where the criteria are more flexible and culturally influenced. Societal beauty ideals, stigma around mental health, and access to care all impact how eating disorder NOS is perceived and treated. Health professionals must apply a culturally sensitive lens when evaluating symptoms and determining whether an unspecified eating disorder is present.
How does social media impact individuals with eating disorder NOS or EDNOS?
Social media can exacerbate disordered eating tendencies, particularly in individuals with vulnerable or undiagnosed conditions. Those with EDNOS eating disorder symptoms may feel invalidated by posts that portray eating disorders in extreme or stereotypical ways. Additionally, the constant exposure to diet culture, comparison, and body-focused content can worsen symptoms associated with eating disorder NOS. While social media can offer community and resources, it can also trigger anxiety, shame, and relapse in those with an unspecified eating disorder. Curating feeds with recovery-focused and body-positive accounts can be a helpful coping strategy.
Are there specific challenges in treating EDNOS that differ from treating anorexia or bulimia?
Absolutely. One major challenge in treating EDNOS is diagnostic ambiguity, which can lead to uncertainty in treatment planning. Many providers may default to general eating disorder protocols that do not address the unique and fluctuating symptoms of an eating disorder not specified. This can make individuals feel misunderstood or underserved. Furthermore, insurance coverage is often tied to specific DSM V diagnoses, making it more difficult for those with EDNOS or an unspecified eating disorder to access care. Customized, client-centered approaches are especially important for this population.
Can someone recover fully from an unspecified eating disorder without a formal diagnosis?
Yes, full recovery is possible even without a formal diagnosis. Many people with eating disorders not otherwise specified EDNOS never receive a definitive label but still benefit from therapy, nutritional support, and lifestyle changes. The key is addressing the underlying thought patterns, emotional triggers, and behavioral cycles contributing to disordered eating. Whether or not someone meets the criteria for binge eating disorder DSM-5 or another specific diagnosis, their recovery journey is just as valid. Recognition, rather than labeling, is often the first step toward healing.
What are the long-term risks if an EDNOS eating disorder goes untreated?
When left untreated, eating disorder NOS can result in both psychological and physiological complications. These may include nutrient deficiencies, hormonal imbalances, digestive issues, and an increased risk of anxiety, depression, or substance use. The chronic stress associated with an unspecified eating disorder can also weaken immune function and impair cognitive performance. Socially, relationships may suffer as individuals withdraw or become preoccupied with food and body image. The sooner EDNOS is addressed, the better the chances of preventing long-term damage and supporting sustainable recovery.
How can family and friends best support someone with an eating disorder not otherwise specified?
Support systems play a pivotal role in recovery, but it’s important that loved ones approach with sensitivity and awareness. Educating themselves on the nuances of EDNOS and other unspecified eating disorders helps avoid harmful assumptions or language. Rather than focusing on food or appearance, offering emotional validation and asking open-ended questions encourages connection. In many cases, helping the individual find professional support, whether for EDNOS or binge eating disorder DSM-5, can make all the difference. Most importantly, maintaining consistent, judgment-free communication builds trust and promotes healing.
Is it possible to experience remission from EDNOS while still facing occasional disordered thoughts?
Yes, remission from EDNOS or an eating disorder not specified does not necessarily mean the complete absence of all disordered thoughts. Recovery often involves managing residual symptoms with tools learned in therapy, such as cognitive reframing and emotion regulation. It’s normal for old patterns to resurface during periods of stress or life transition. The key difference in remission is that individuals are equipped to respond to these thoughts without engaging in harmful behaviors. Acknowledging this reality helps set realistic expectations and empowers long-term resilience.
Reclaiming Health: A Comprehensive Path Forward for EDNOS and Unspecified Eating Disorders
Recovery from EDNOS and unspecified eating disorders is a deeply personal and non-linear process. There is no singular roadmap, but with the right combination of clinical support, nutritional rehabilitation, lifestyle changes, and therapeutic engagement, healing is not only possible—it is sustainable. Recognizing the validity of eating disorders not otherwise specified EDNOS and providing evidence-based, compassionate care paves the way for long-term wellness.
In this journey, nutrition is not merely a matter of eating more or less—it is about rebuilding a relationship with food rooted in trust, nourishment, and respect. Integrating holistic lifestyle practices such as mindful eating, joyful movement, and emotional self-regulation supports not only physical recovery but also emotional and psychological resilience. These practices are especially meaningful for those who may feel overlooked or misunderstood within traditional diagnostic frameworks.
Therapy remains a cornerstone of recovery, offering individuals a space to unpack their experiences, challenge harmful beliefs, and cultivate new patterns of thought and behavior. Whether dealing with symptoms that resemble dsm v binge eating disorder or fluctuating between disordered behaviors, therapy provides a foundation of safety and transformation. Importantly, therapeutic support validates the experiences of those with an eating disorder not specified, affirming that their struggles are both real and treatable.
As understanding continues to evolve, the health and wellness community must remain committed to inclusivity and nuance. No one should be denied care because their symptoms do not fit neatly into a diagnostic box. By embracing the complexity of EDNOS eating disorder presentations and responding with flexibility and empathy, we can create systems that support true healing for everyone. In doing so, we honor the courage it takes to seek help and affirm the hope that recovery offers—a future grounded in nourishment, balance, and self-compassion.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.

