In the realm of digestive and eating disorders, few conditions remain as shrouded in misunderstanding and clinical obscurity as rumination syndrome. Despite affecting individuals across all age groups, this condition often escapes early detection due to its complex and sometimes subtle symptoms. Characterized by the effortless regurgitation of recently ingested food, rumination syndrome is frequently misdiagnosed or mistaken for more well-known gastrointestinal or psychological disorders. This article explores the intricate mechanisms behind rumination syndrome, its overlap with other eating conditions, and the far-reaching nutritional and psychological implications for those affected. Through a blend of clinical research, patient perspectives, and emerging treatment modalities, we aim to shed light on a condition that merits greater awareness within the spheres of mindful eating and holistic health.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
What Is Rumination Syndrome and How Does It Differ from Other Eating Disorders?
Rumination syndrome, sometimes referred to as rumination disorder or rumination eating disorder, is a chronic condition in which individuals repeatedly and unintentionally regurgitate partially digested food shortly after eating. Unlike vomiting, this regurgitation is not preceded by nausea or abdominal pain, and the expelled food often retains a fresh taste, making it markedly different from emesis related to gastrointestinal illness. This food may be rechewed and swallowed or expelled, often without distress or discomfort. Because the behavior tends to occur repeatedly, sometimes multiple times during or after meals, it can severely interfere with daily life and nutritional health.
What distinguishes rumination syndrome from other eating disorders like bulimia nervosa is the absence of intent to purge for weight control. Individuals with rumination disorder do not typically experience body image distortions or fear of weight gain that characterize bulimia or anorexia. Similarly, it differs from gastroesophageal reflux disease (GERD), which involves acidic reflux from the stomach due to a weak lower esophageal sphincter. Instead, rumination syndrome is driven by learned behaviors—often subconscious—that involve the voluntary contraction of abdominal muscles that push food back up into the mouth.
Rumination syndrome can affect infants, children, adolescents, and adults, although the manifestation of symptoms may vary by age. In infants, the condition may resolve on its own as they mature. In older children and adults, however, the condition often persists unless specifically treated. Unfortunately, this longevity is compounded by the lack of public awareness and misidentification by healthcare providers, delaying appropriate rumination syndrome treatment.
Unraveling the Causes: Behavioral, Psychological, and Physiological Contributors
Understanding the root causes of rumination syndrome requires a multidisciplinary perspective. Behavioral scientists suggest that rumination disorder may develop from a learned response, particularly after an initial illness or stressful event. For instance, if regurgitation occurs after a bout of food poisoning or stomach flu, the body may adapt to this experience through repeated contractions that eventually become habitual. Once the behavior is reinforced—often unconsciously—it can persist long after the original trigger has disappeared.
On a psychological level, stress, anxiety, and trauma are common threads among those diagnosed with rumination syndrome. These individuals may use the act of regurgitation as a coping mechanism, either consciously or unconsciously, to alleviate internal tension. The condition is also found more frequently in people with underlying mental health disorders such as generalized anxiety disorder, obsessive-compulsive disorder, or autism spectrum disorder, where repetitive behaviors are common.
Physiologically, some researchers believe abnormalities in the diaphragm or increased intra-abdominal pressure could contribute to the condition. However, unlike reflux disorders or motility issues, rumination syndrome does not typically involve structural damage to the esophagus or stomach lining. This absence of physical pathology makes diagnosis particularly challenging, especially in the absence of clear psychosocial markers.
Environmental and familial factors also play a role. In children and adolescents, rumination eating disorder may be linked to feeding issues or family dynamics where stress, control, or lack of mealtime structure becomes a contributing factor. Recognizing and addressing these environmental variables can be crucial in tailoring an effective rumination syndrome treatment plan.
The Nutritional Fallout: How Rumination Food Behaviors Disrupt Wellness
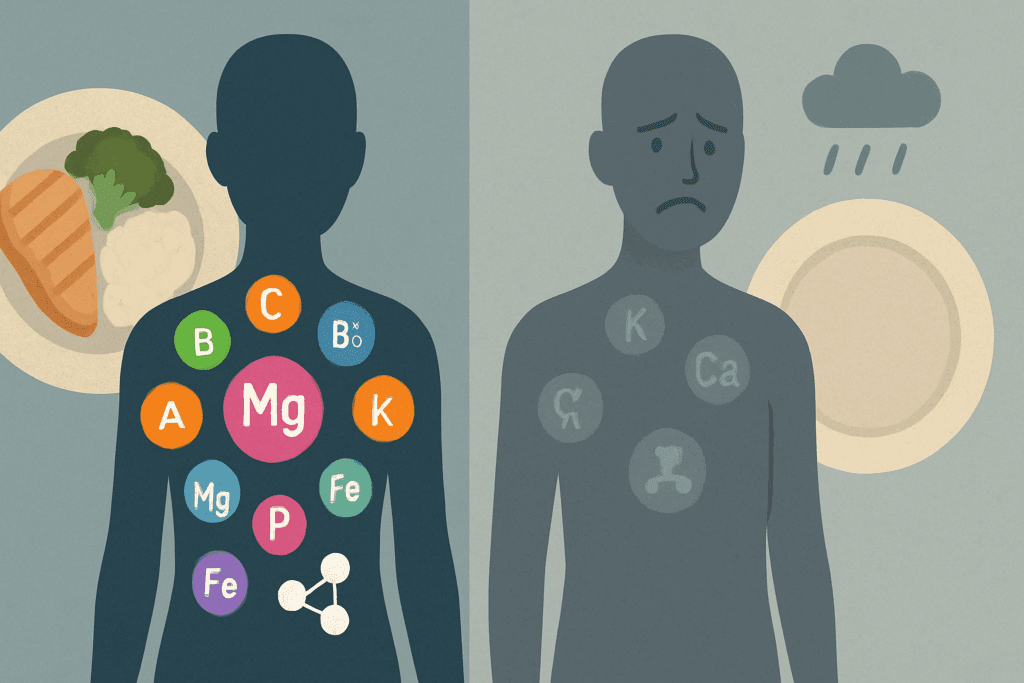
The impact of rumination syndrome on nutritional health is both immediate and profound. Because food is not fully digested or absorbed, individuals with this disorder often suffer from malnutrition, weight loss, and deficiencies in essential vitamins and minerals. Over time, the body’s inability to retain adequate nourishment can weaken the immune system, disrupt hormonal balance, and impair growth and development—particularly in children and adolescents.
Compounding this issue is the fact that individuals may begin to avoid eating altogether in an attempt to prevent regurgitation episodes. This avoidance behavior often leads to a restrictive diet lacking in diversity and nutritional adequacy. Some may favor bland or liquid meals over solid foods, mistakenly believing this will ease symptoms. As a result, rumination food choices tend to become increasingly limited, further exacerbating malnutrition risks.
Moreover, the repetitive regurgitation of stomach contents exposes the esophagus and oral cavity to digestive enzymes and gastric acids, which may lead to dental erosion, throat irritation, and chronic inflammation. These physical side effects add another layer of complexity to the nutritional challenges posed by rumination disorder. The combined effects of nutrient loss and physiological damage can significantly lower quality of life and overall wellness.
Socially, eating in public or with others becomes a source of anxiety and embarrassment. The fear of visible regurgitation episodes or strange eating behaviors can lead to isolation and avoidance of social gatherings, contributing to mental health decline and a cycle of worsening symptoms. Thus, addressing the nutritional and psychological impacts of rumination syndrome requires an integrated, multidisciplinary approach that spans physical, emotional, and behavioral domains.

The Diagnostic Process: Challenges and Clinical Considerations
Diagnosing rumination syndrome is notoriously complex. Many healthcare providers may initially suspect more common gastrointestinal disorders such as GERD, gastroparesis, or functional dyspepsia. Because standard imaging and laboratory tests often return normal results, patients may undergo a series of unnecessary and invasive procedures before a correct diagnosis is made. This diagnostic delay not only prolongs suffering but also complicates the course of rumination syndrome treatment.
A thorough clinical history is the cornerstone of diagnosis. Healthcare professionals must ask specific questions about meal timing, symptom onset, and the nature of regurgitation. Observational methods, such as watching the patient eat in a controlled environment, can be extremely useful in confirming behavioral patterns consistent with rumination. Video-fluoroscopic studies and high-resolution manometry can also provide insight into the mechanics of the regurgitation, although they are not always necessary.
Psychological evaluations are equally critical. Understanding the emotional and behavioral context surrounding the symptoms allows clinicians to differentiate rumination eating disorder from other psychological or somatic conditions. In adolescents and adults, structured interviews and validated questionnaires can help identify comorbid mental health disorders that may require concurrent treatment.
Misdiagnosis can have serious consequences. When rumination syndrome is mistaken for bulimia or voluntary vomiting, patients may be treated inappropriately or stigmatized. Similarly, when misattributed to reflux disease, they may be prescribed medications like proton pump inhibitors that offer no relief. Educating both patients and healthcare providers about the nuances of rumination disorder is essential for accurate recognition and timely intervention.
Treatment Strategies: Behavioral Therapy and Holistic Support
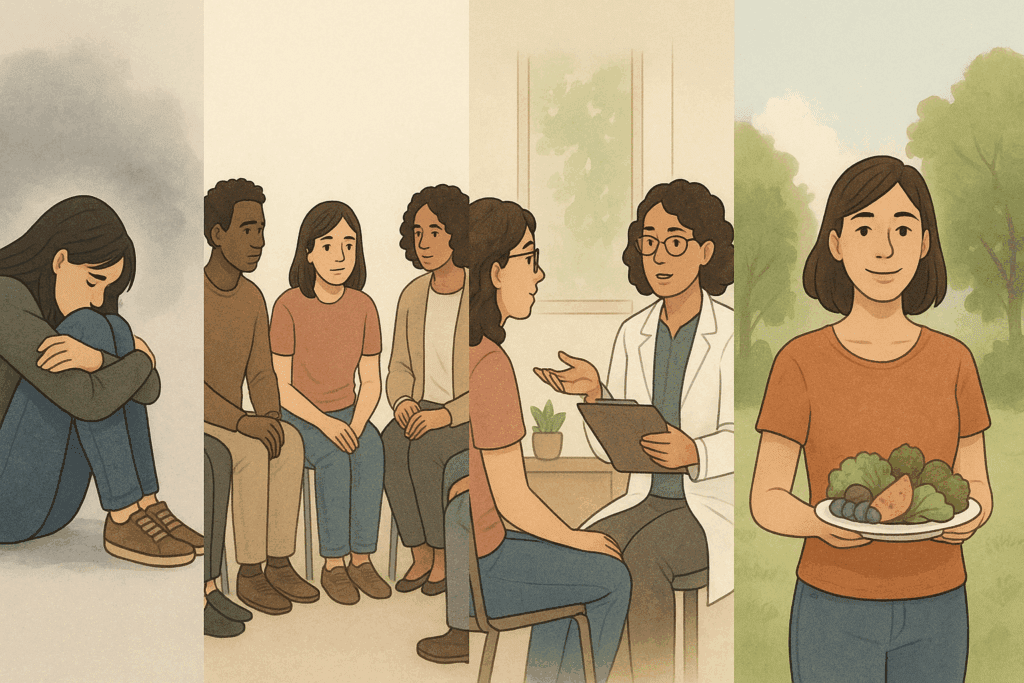
The most effective approach to rumination syndrome treatment is behavioral therapy, particularly a technique known as diaphragmatic breathing. This method involves teaching patients to engage their diaphragm during and after meals in a way that prevents the abdominal contractions responsible for regurgitation. With consistent practice, diaphragmatic breathing can significantly reduce or eliminate symptoms in many patients.
Cognitive-behavioral therapy (CBT)b is another valuable tool, especially when rumination is linked to underlying anxiety or obsessive thought patterns. CBT can help patients develop healthier coping mechanisms and reduce the compulsive aspects of the disorder. In some cases, biofeedback techniques are employed to enhance awareness of muscle contractions and support the development of new behavioral responses.
Nutritional rehabilitation is also a critical component of treatment. Working with a registered dietitian can help patients restore nutritional balance, diversify their diets, and address any nutrient deficiencies caused by prolonged regurgitation. This support also includes addressing fears or anxieties around eating, which may persist even as physical symptoms improve.
Support groups and peer counseling can provide emotional reinforcement, reducing feelings of isolation and shame that often accompany rumination eating disorder. Holistic approaches, such as mindfulness training and stress reduction techniques, are also gaining traction in clinical settings. These methods not only help reduce symptom frequency but also improve overall quality of life.
While there is no single medication specifically approved for rumination syndrome, pharmacological support may be used in certain cases where anxiety, depression, or obsessive-compulsive tendencies are prominent. Medications should be used as an adjunct to, rather than a replacement for, behavioral and psychological interventions.
Living with Rumination Syndrome: Patient Experiences and Long-Term Outlook
Living with rumination syndrome presents daily challenges that extend beyond physical symptoms. Many individuals describe a long and frustrating journey toward diagnosis, marked by confusion, skepticism, and ineffective treatments. For some, the path includes years of medical visits and unnecessary procedures before receiving an accurate diagnosis.
Patients often report a sense of relief upon learning that their condition has a name and is treatable. This recognition is a critical step in reducing self-blame and initiating a successful treatment journey. Over time, with consistent therapeutic intervention and lifestyle adjustments, many individuals experience significant symptom improvement and restored nutritional health.
Long-term management focuses on maintenance of behavioral techniques, emotional resilience, and continued engagement with healthcare providers. For some, flare-ups may still occur during periods of high stress or emotional turmoil, making ongoing support essential. Relapses should not be viewed as failures but rather as reminders to re-engage with proven strategies and seek additional guidance when needed.
Advocacy and education remain vital components of long-term care. Patients and their families benefit from increased public awareness and better training for medical professionals. As understanding of the condition expands, so too does the hope for improved diagnostic tools and more comprehensive treatment options.
The journey through rumination disorder is deeply personal, shaped by individual biology, life experience, and support systems. Yet across these diverse narratives, one theme is clear: with the right combination of knowledge, care, and perseverance, recovery is possible.
Frequently Asked Questions: Understanding Rumination Syndrome and Its Broader Implications
What are some early lifestyle signs that may indicate the onset of rumination syndrome?
While the clinical diagnosis of rumination syndrome usually hinges on specific gastrointestinal symptoms, subtle lifestyle cues often emerge first. Individuals might begin to avoid social meals due to unexplained discomfort or embarrassment after eating. They may also develop peculiar meal habits—such as eating more slowly than usual or sticking exclusively to bland, easily digestible foods—in an attempt to manage recurring symptoms. These behavioral shifts can be the body’s unconscious attempt to reduce the frequency of regurgitation episodes. Recognizing these changes early on can support timely intervention and reduce the long-term effects of rumination disorder.
Can individuals with rumination eating disorder maintain a healthy weight?
Yes, it is possible—though challenging—for individuals with a rumination eating disorder to maintain a healthy weight, especially if their episodes are less frequent or if they adapt by consuming high-calorie foods. However, this can lead to an imbalance in nutritional quality, as caloric intake may not equate to adequate nutrient absorption. Over time, even individuals with seemingly normal body weight may suffer from micronutrient deficiencies and weakened immunity due to poor digestion and repeated loss of partially digested food. Careful monitoring and nutrition support become essential in these cases. Addressing rumination syndrome treatment early helps prevent such hidden consequences.
How does rumination syndrome affect oral and dental health?
The repeated exposure of the mouth and teeth to partially digested rumination food—especially if it contains gastric acid—can be detrimental to oral health. Enamel erosion, increased tooth sensitivity, and persistent bad breath are common issues for individuals dealing with rumination disorder. Additionally, regurgitation may irritate the soft tissues of the mouth and throat, causing chronic soreness or inflammation. Dentists who notice these patterns without another explanation might be the first healthcare professionals to suspect a behavioral origin like rumination syndrome. Collaborative care involving dental, nutritional, and psychological support is key for holistic recovery.
Is there a genetic predisposition to developing rumination eating disorder?
Research into the genetic basis of rumination eating disorder is still in its early stages, but current insights suggest that a combination of genetic vulnerability and environmental stressors may contribute to its development. Families with a history of anxiety disorders, gastrointestinal sensitivities, or other eating disorders may be more likely to experience intergenerational patterns. This doesn’t mean rumination syndrome is inherited in a direct way, but rather that certain inherited traits—like heightened stress responses or behavioral rigidity—can create a fertile ground for the disorder. Understanding this interplay can guide more personalized approaches to rumination syndrome treatment, especially in family-based or pediatric cases.
What role does sensory sensitivity play in rumination disorder?
Sensory processing issues are frequently reported by individuals with rumination disorder, particularly among children and those on the autism spectrum. Hypersensitivity to texture, taste, or temperature of food can trigger discomfort that leads to regurgitation as a means of avoidance. In this context, rumination food aversions are not just psychological but stem from genuine neurological differences. Therapists specializing in sensory integration may help patients gradually build tolerance to various food experiences, making it easier to maintain a balanced diet and reduce symptoms. Tailoring rumination syndrome treatment to include sensory strategies can lead to more sustainable outcomes.
How do stress management techniques influence the success of rumination syndrome treatment?
Stress management is not merely complementary—it’s often central to effective rumination syndrome treatment. Because emotional distress can exacerbate muscle contractions in the abdomen, anxiety frequently intensifies regurgitation symptoms. Techniques such as mindfulness meditation, guided imagery, or progressive muscle relaxation can help regulate the autonomic nervous system. These tools are particularly helpful for individuals whose rumination disorder is triggered by performance pressure or social anxiety. Integrating stress-reduction techniques into daily routines empowers patients to break the cycle of regurgitation and reclaim a sense of normalcy.
Can restrictive diets worsen the symptoms of rumination syndrome?
Ironically, attempts to self-manage rumination syndrome through restrictive eating can sometimes make symptoms worse. Limiting food variety in an effort to avoid rumination food triggers can lead to nutrient gaps, irregular digestion, and increased anxiety around mealtimes. In some cases, these restrictions mirror disordered eating behaviors and complicate recovery. A registered dietitian familiar with rumination eating disorder can help patients reintroduce diverse foods in a structured and psychologically safe manner. When balanced with behavioral therapy, this approach supports both physical healing and emotional resilience.
Are there specific challenges in diagnosing rumination syndrome in children versus adults?
Yes, the presentation of rumination syndrome differs significantly between children and adults, leading to diagnostic challenges. Young children may not have the language to describe their symptoms, and regurgitation might be misattributed to common conditions like reflux or colic. In adults, rumination disorder can be mistaken for intentional vomiting or even malingering, particularly in cases without visible distress. Additionally, older patients may mask symptoms out of embarrassment, further delaying diagnosis. Pediatric and adult healthcare providers alike must be trained to recognize subtle behavioral clues and probe beyond gastrointestinal symptoms.
What emerging technologies are improving the diagnosis and treatment of rumination disorder?
Advancements in wearable diagnostic devices, such as pH monitoring systems and high-resolution manometry, are enhancing clinicians’ ability to identify the mechanical patterns behind rumination disorder. These technologies provide real-time data on esophageal activity and diaphragm function during and after meals. On the treatment side, digital health platforms now offer guided diaphragmatic breathing programs and teletherapy for remote behavioral coaching. Virtual reality (VR) exposure therapy is also being explored to desensitize individuals to eating-related anxiety. As these innovations become more accessible, the landscape of rumination syndrome treatment continues to evolve, offering patients more personalized and flexible options.
What long-term outcomes can individuals expect after successful treatment of rumination syndrome?
With early and sustained intervention, many individuals with rumination syndrome can experience full remission of symptoms and return to a healthy, balanced lifestyle. Long-term outcomes often depend on the presence of coexisting mental health conditions and the degree of nutritional rehabilitation achieved. While flare-ups may occasionally recur during times of stress, most patients can manage these episodes effectively with learned behavioral tools. Developing a robust support system and continuing therapeutic engagement—even during remission—can significantly reduce relapse risk. Ultimately, rumination syndrome treatment offers not just symptom relief but the potential for improved self-awareness and lifelong wellness habits.
Conclusion: Fostering Awareness and Wellness Through Understanding Rumination Syndrome
Rumination syndrome, though often misunderstood and misdiagnosed, is a genuine and treatable eating disorder that significantly affects nutritional health and overall wellness. Through a careful exploration of its causes, symptoms, and treatment pathways, we gain valuable insights into how this condition disrupts daily life and what can be done to restore balance. Recognizing the behavioral nature of rumination disorder is key to developing effective, individualized rumination syndrome treatment plans that integrate medical, nutritional, and psychological care.
As awareness grows, so too does the opportunity for early intervention, compassionate support, and lasting recovery. For those navigating the challenges of rumination eating disorder, knowledge is not just empowering—it is a vital part of healing. By fostering a greater understanding of rumination food behaviors and their consequences, we move closer to a more informed and inclusive approach to health and nutrition.
In the broader context of mindful eating and a healthier lifestyle, acknowledging and addressing rumination syndrome affirms the importance of seeing each individual’s experience with compassion, expertise, and clarity. Through education, empathy, and evidence-based care, we can ensure that those affected by this complex condition are no longer overlooked—and that they receive the help and hope they deserve.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.

