Understanding Fatty Liver Disease and Its Importance
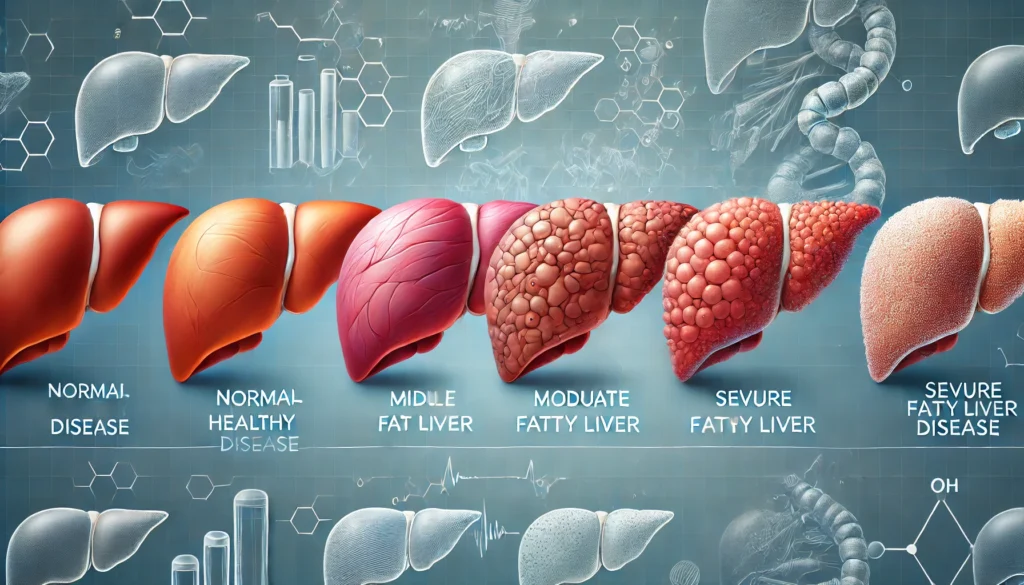
Fatty liver disease is a growing health concern worldwide, affecting millions of people. It occurs when excessive fat accumulates in liver cells, leading to potential liver damage if left untreated. While many individuals with fatty liver disease remain asymptomatic, early detection is crucial to prevent progression to more severe liver conditions such as fibrosis, cirrhosis, or even liver cancer. Recognizing the signs and risk factors early on can help individuals take preventive measures and seek appropriate medical intervention.
You may also like: The Best Liver Detox Supplements: How to Choose Safe and Effective Support for Your Liver
The liver plays a fundamental role in metabolism, detoxification, and overall health. However, when excessive fat accumulates in this vital organ, it can impair its function. The two primary types of fatty liver disease are nonalcoholic fatty liver disease (NAFLD) and alcoholic fatty liver disease (AFLD). NAFLD is commonly associated with obesity, insulin resistance, and metabolic syndrome, while AFLD results from excessive alcohol consumption. Both conditions can progress to more severe forms, making early recognition essential.
Early detection is challenging because fatty liver disease does not always present obvious symptoms. However, understanding its risk factors and identifying potential signs can aid in timely diagnosis. Healthcare professionals often rely on imaging techniques, such as ultrasound and MRI, to detect fatty liver disease visually. Additionally, blood tests measuring liver enzymes may indicate liver damage. By raising awareness about the condition and its early signs, individuals can take proactive steps toward liver health and overall well-being.

Risk Factors for Developing Fatty Liver Disease
Fatty liver disease does not develop in isolation; several lifestyle and genetic factors contribute to its onset. One of the most significant risk factors is obesity, as excess body fat correlates with fat accumulation in the liver. Individuals with a high body mass index (BMI) are more likely to develop NAFLD, particularly when excess weight is concentrated around the abdomen. Similarly, insulin resistance and type 2 diabetes increase the risk of fatty liver disease due to their impact on glucose metabolism and fat storage.
Poor dietary habits, including high consumption of refined carbohydrates, sugary beverages, and saturated fats, play a critical role in fatty liver development. Diets rich in processed foods, excessive sugar intake, and trans fats contribute to liver fat accumulation. Conversely, a diet high in fiber, healthy fats, and lean proteins can help prevent fatty liver disease by promoting optimal liver function and reducing inflammation.
Excessive alcohol consumption is the primary cause of AFLD, as alcohol metabolism produces harmful byproducts that damage liver cells. While moderate alcohol consumption may not necessarily lead to fatty liver disease, chronic heavy drinking significantly increases the risk. Additionally, genetic predisposition may influence susceptibility to fatty liver disease. Some individuals may have a genetic tendency to store fat in the liver, making them more prone to developing the condition despite having a healthy lifestyle.
Recognizing Symptoms of Fatty Liver Disease
Many individuals with fatty liver disease remain asymptomatic for years, making it difficult to detect without medical evaluation. However, as the condition progresses, certain signs and symptoms may become more apparent. One of the most common early symptoms is persistent fatigue, which results from impaired liver function and metabolic disturbances. Individuals may also experience mild discomfort or pain in the upper right abdomen, where the liver is located.
Unexplained weight gain or difficulty losing weight can be indicative of metabolic imbalances associated with fatty liver disease. The liver plays a crucial role in metabolism, and when its function is compromised, it can lead to weight fluctuations. Additionally, some individuals may develop dark patches of skin, particularly on the neck or underarms, known as acanthosis nigricans. This condition is often associated with insulin resistance, a common risk factor for NAFLD.
As fatty liver disease progresses, individuals may notice more severe symptoms such as jaundice, which causes yellowing of the skin and eyes due to impaired bilirubin processing. Other signs include swelling in the legs and abdomen, indicating fluid retention. In advanced stages, liver cirrhosis may develop, leading to significant complications such as liver failure and an increased risk of liver cancer. Recognizing these symptoms early can prompt timely medical intervention and lifestyle modifications.
Diagnostic Methods for Identifying Fatty Liver Disease
Healthcare professionals use various diagnostic tools to confirm the presence of fatty liver disease. One of the most commonly used imaging techniques is ultrasound, which provides visual evidence of fat accumulation in the liver. Ultrasound is a non-invasive, widely available, and cost-effective method for detecting fatty liver disease. However, it may not always differentiate between simple fatty liver and more advanced stages of liver disease.
Magnetic resonance imaging (MRI) and computed tomography (CT) scans offer more detailed images of the liver, allowing for a precise assessment of fat accumulation. These advanced imaging techniques can help determine the severity of fatty liver disease and detect fibrosis or cirrhosis. In some cases, healthcare providers may recommend a liver biopsy, where a small tissue sample is taken for microscopic examination. Although invasive, a liver biopsy provides definitive information about liver health and the extent of damage.
Blood tests measuring liver enzyme levels, such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), can indicate liver inflammation and damage. Elevated liver enzyme levels often suggest an underlying liver condition, prompting further evaluation. Other blood markers, including fasting glucose levels and lipid profiles, help assess metabolic health and determine the presence of insulin resistance or dyslipidemia, both of which are associated with fatty liver disease.
Preventive Measures and Treatment Strategies
Prevention and management of fatty liver disease primarily revolve around lifestyle modifications. Adopting a balanced diet rich in whole foods, including vegetables, fruits, whole grains, and lean proteins, can significantly reduce liver fat accumulation. Reducing intake of processed foods, added sugars, and unhealthy fats is essential for liver health. Incorporating omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, can help reduce liver inflammation and improve lipid metabolism.
Regular physical activity plays a crucial role in preventing and managing fatty liver disease. Engaging in at least 150 minutes of moderate-intensity exercise per week can improve insulin sensitivity, reduce liver fat, and enhance overall metabolic health. Activities such as brisk walking, cycling, swimming, and strength training contribute to weight management and liver function optimization. Additionally, maintaining a healthy weight through a combination of diet and exercise is one of the most effective ways to prevent fatty liver disease.
Avoiding excessive alcohol consumption is critical in preventing AFLD and reducing the risk of liver damage. For individuals diagnosed with fatty liver disease, complete alcohol abstinence is often recommended to prevent further liver complications. Hydration also plays a vital role in liver health, as adequate water intake supports detoxification and metabolic processes. Limiting exposure to environmental toxins and medications that may strain the liver can further contribute to liver protection.
Frequently Asked Questions (FAQ) About Fatty Liver Disease
1. What are some early warning signs of fatty liver disease?
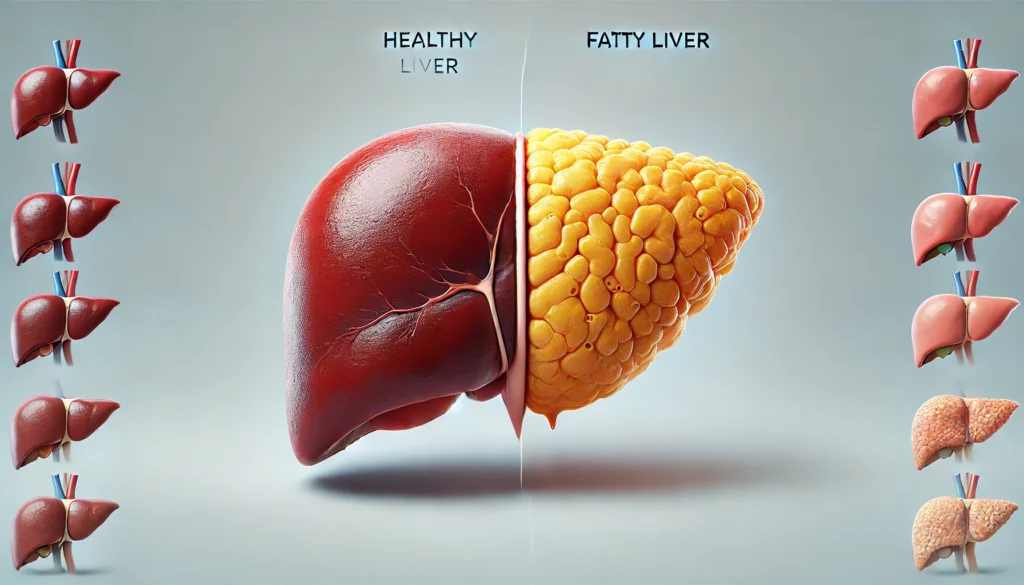
Early warning signs of fatty liver disease can be subtle and often go unnoticed. Many individuals experience fatigue, mild abdominal discomfort, or a feeling of fullness in the upper right side of the abdomen. Some people notice unexplained weight gain or difficulty losing weight, as fatty liver disease is often linked to metabolic syndrome. While blood tests may indicate elevated liver enzymes, imaging techniques such as fatty liver images and fatty liver pictures provide a clearer view of fat accumulation in the liver. If left unchecked, these early signs can progress into more severe symptoms, including inflammation and fibrosis.
2. Can fatty liver disease be reversed, and if so, how?
Yes, fatty liver disease can often be reversed, especially in its early stages. The most effective way to reverse it is through lifestyle modifications, such as adopting a healthy diet, engaging in regular physical activity, and reducing sugar and alcohol intake. Studies show that even a modest 5-10% reduction in body weight can significantly decrease liver fat levels. Regular monitoring using pictures of fatty liver disease can help track improvement over time. Additionally, maintaining balanced blood sugar and cholesterol levels plays a crucial role in liver recovery.
3. How does diet impact the development of fatty liver disease?
Diet plays a critical role in both the development and reversal of fatty liver disease. Diets high in processed foods, refined sugars, and saturated fats contribute to excessive fat storage in liver cells. On the other hand, a diet rich in whole foods, such as leafy greens, lean proteins, and healthy fats, supports liver function. Certain foods, like coffee, green tea, and omega-3 fatty acids, have been shown to reduce liver fat accumulation. By examining fatty liver images before and after dietary interventions, healthcare providers can visually confirm the impact of dietary changes. Avoiding fructose-laden beverages is also essential in preventing further liver damage.
4. Are there any specific exercises that help reduce liver fat?
Both aerobic exercise and resistance training have been proven effective in reducing liver fat. Activities such as brisk walking, cycling, and swimming help burn excess fat and improve insulin sensitivity. Strength training, including weight lifting and resistance bands, helps increase muscle mass, which in turn enhances metabolism and fat-burning capacity. Research has shown that even moderate-intensity workouts can significantly lower liver fat when performed consistently. Comparing fatty liver pictures before and after a structured exercise routine often demonstrates visible reductions in liver fat deposits. It’s important to find an exercise routine that is sustainable and enjoyable to maintain long-term liver health.
5. What role does alcohol play in fatty liver disease?
Alcohol consumption is a major factor in liver disease, particularly alcoholic fatty liver disease (AFLD). Even in cases of non-alcoholic fatty liver disease (NAFLD), drinking alcohol can accelerate liver damage. Alcohol contributes to inflammation, oxidative stress, and fat accumulation in liver cells, worsening the condition. Individuals diagnosed with fatty liver disease are often advised to eliminate or significantly reduce alcohol intake. Reviewing fatty liver pictures of individuals who drink regularly versus those who abstain can reveal stark differences in liver health over time. Moderation or complete avoidance of alcohol can improve liver function and slow disease progression.
6. How can fatty liver disease affect other parts of the body?
Fatty liver disease is not just a liver condition—it has systemic effects on the entire body. It increases the risk of cardiovascular diseases, as excess liver fat contributes to high cholesterol and blood pressure. It is also closely linked to insulin resistance, raising the risk of type 2 diabetes. Chronic inflammation caused by fatty liver disease can affect the gut microbiome, leading to digestive issues and immune dysfunction. By examining fatty liver images alongside cardiovascular scans, medical professionals often find correlations between liver fat and artery health. Addressing fatty liver disease early can help prevent broader metabolic complications.
7. What medical tests are used to diagnose fatty liver disease?
Fatty liver disease is typically diagnosed through a combination of blood tests, imaging studies, and sometimes liver biopsies. Blood tests measure liver enzyme levels, which can indicate liver stress or damage. Imaging techniques, such as ultrasound, CT scans, and MRI scans, provide clear fatty liver pictures that reveal fat accumulation. In more severe cases, a liver biopsy may be performed to assess inflammation and fibrosis. Advanced imaging, such as elastography, can help evaluate liver stiffness and the presence of fibrosis, allowing for a non-invasive assessment of liver health.
8. How does stress influence fatty liver disease?
Chronic stress plays a significant role in the progression of fatty liver disease by contributing to inflammation, hormonal imbalances, and poor dietary choices. Stress triggers the release of cortisol, which promotes fat storage, particularly in the liver and abdomen. It also influences cravings for unhealthy, high-sugar foods that can exacerbate liver fat accumulation. Mindfulness practices, such as meditation, yoga, and deep breathing, have been shown to improve stress management and support liver health. Individuals who implement stress-reducing techniques often see improvements in their liver function, which can be verified through changes in fatty liver images over time.
9. Are there any new treatments or research developments for fatty liver disease?
Recent research has focused on developing targeted medications and advanced diagnostic techniques for fatty liver disease. Some promising treatments include GLP-1 receptor agonists, originally developed for diabetes, which have shown potential in reducing liver fat. Clinical trials are also exploring anti-inflammatory drugs that may slow fibrosis progression. Non-invasive imaging technologies are improving the accuracy of diagnosing and monitoring fatty liver disease, reducing the need for biopsies. In addition to medical interventions, dietary advancements, such as precision nutrition plans, are being tailored to individual metabolic needs. By tracking progress with pictures of fatty liver disease, researchers can assess the effectiveness of new treatments over time.
10. How can someone prevent fatty liver disease from developing?
Preventing fatty liver disease involves adopting a healthy lifestyle before any signs of liver damage appear. This includes maintaining a balanced diet, exercising regularly, avoiding excessive alcohol consumption, and managing stress effectively. Ensuring proper hydration and sleep quality also supports liver function and prevents fat buildup. Regular health check-ups and monitoring through fatty liver pictures can help identify early changes and allow for timely intervention. By taking proactive steps, individuals can protect their liver health and reduce the risk of long-term complications.
Conclusion: Taking Charge of Liver Health
Recognizing fatty liver disease early is essential for preventing its progression and associated complications. By understanding the risk factors, identifying early symptoms, and utilizing appropriate diagnostic tools, individuals can take proactive steps toward liver health. Adopting a nutritious diet, engaging in regular physical activity, and making informed lifestyle choices can significantly reduce the risk of developing fatty liver disease.
Awareness and early intervention can make a substantial difference in liver health outcomes. Regular medical check-ups, liver function tests, and imaging studies can help detect fatty liver disease in its early stages. By prioritizing liver health, individuals can enhance their overall well-being and reduce the likelihood of severe liver complications in the future.
fatty liver prevention, liver health strategies, early signs of liver disease, nonalcoholic fatty liver, alcohol-induced liver damage, metabolic health and liver, diet for fatty liver, exercise for liver health, liver function tests, liver detoxification methods, healthy liver diet, symptoms of liver disease, weight management for fatty liver, fatty liver risk factors, lifestyle changes for liver health, how to reduce liver fat, best foods for liver health, ultrasound for fatty liver, liver disease awareness, fatty liver management tips
Further Reading:
Non-alcoholic fatty liver disease
Non-alcoholic fatty liver disease: a practical approach to diagnosis and staging
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.

