The liver is an essential organ responsible for numerous vital functions, including detoxification, protein synthesis, and fluid regulation. However, when the liver is compromised due to disease, these functions can become impaired, leading to a cascade of complications. One such complication is hepatic edema, a condition characterized by swelling in the feet and face due to fluid retention. This article explores the mechanisms behind hepatic edema, its causes, symptoms, and management strategies to help individuals understand the impact of liver disease on fluid balance in the body.
You may also like: The Best Liver Detox Supplements: How to Choose Safe and Effective Support for Your Liver
The Role of the Liver in Fluid Regulation
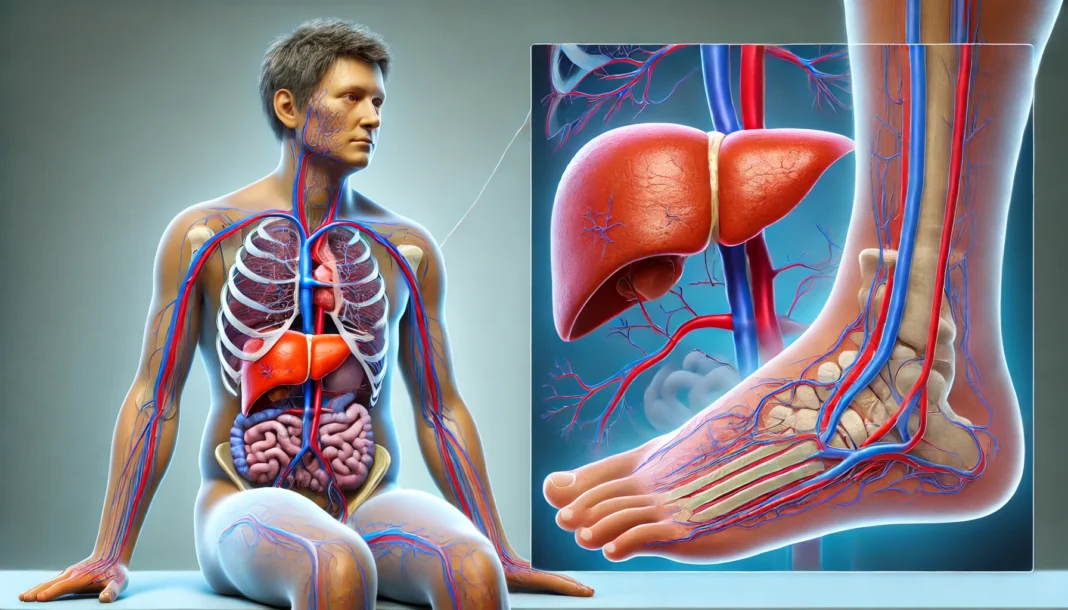
The liver plays a critical role in maintaining the body’s fluid balance by regulating proteins such as albumin, which helps retain fluid within the blood vessels. When liver function declines, albumin levels drop, leading to fluid leakage into surrounding tissues. This process results in edema, often seen in the lower extremities and face. Additionally, the liver is involved in the production of hormones and enzymes that influence kidney function and blood pressure. Impairments in these processes contribute to excessive fluid accumulation, exacerbating swelling in various parts of the body.
Portal hypertension, a condition commonly associated with advanced liver disease, further disrupts normal fluid regulation. Increased pressure in the portal vein leads to fluid leakage into the abdominal cavity, a condition known as ascites. As fluid accumulates, the body compensates by retaining more water and sodium, ultimately exacerbating swelling in the feet and face. These interconnected physiological processes highlight the intricate relationship between liver health and systemic fluid balance.
Causes of Hepatic Edema
Hepatic edema is primarily caused by underlying liver diseases such as cirrhosis, hepatitis, and fatty liver disease. Cirrhosis, the most common culprit, results from chronic liver damage and fibrosis, which progressively impair liver function. As cirrhosis advances, the liver’s ability to produce albumin and regulate vascular pressure diminishes, leading to persistent swelling.
Hepatitis, particularly chronic viral hepatitis B and C, can also contribute to hepatic edema. These infections cause long-term liver inflammation and damage, reducing the organ’s ability to maintain fluid balance. Additionally, non-alcoholic fatty liver disease (NAFLD) has emerged as a significant contributor to hepatic dysfunction. Characterized by fat accumulation in liver cells, NAFLD can progress to cirrhosis, ultimately resulting in fluid retention and swelling.
Another factor leading to hepatic edema is liver cancer, which disrupts normal liver function and contributes to abnormal fluid dynamics. Additionally, excessive alcohol consumption accelerates liver damage, increasing the risk of cirrhosis and, consequently, hepatic edema. Understanding these underlying causes is essential in addressing fluid retention associated with liver disease.
Symptoms and Presentation of Hepatic Edema
Hepatic edema presents with noticeable swelling, primarily in the feet, ankles, and face. This swelling occurs due to excessive fluid accumulation in the interstitial spaces of the body. Individuals with hepatic edema may also experience pitting edema, where pressing on the swollen area leaves a temporary indentation. Swelling in the face is particularly evident in the morning due to overnight fluid redistribution.
In addition to swelling, other symptoms of liver disease often accompany hepatic edema. These may include jaundice, a yellowing of the skin and eyes due to bilirubin buildup; fatigue, stemming from the liver’s reduced ability to metabolize toxins; and unexplained weight gain due to fluid retention. Patients may also experience shortness of breath if fluid accumulation extends to the lungs, a condition known as pleural effusion.
Ascites, another manifestation of hepatic fluid imbalance, often accompanies lower extremity swelling. Individuals with significant ascites may notice abdominal distension and discomfort. The presence of these symptoms underscores the need for medical intervention, as they indicate advanced liver dysfunction requiring prompt management.
Diagnosis and Medical Evaluation
Diagnosing hepatic edema involves a combination of clinical evaluation, imaging studies, and laboratory tests. Physicians assess swelling patterns, medical history, and potential risk factors, such as alcohol use or viral hepatitis exposure. Blood tests play a crucial role in evaluating liver function, with key markers including albumin levels, liver enzymes (AST, ALT), and bilirubin.
Imaging studies, such as ultrasound and CT scans, help visualize liver abnormalities, including cirrhosis, fatty deposits, or tumors. Doppler ultrasound may also be used to assess blood flow in the portal vein and detect signs of portal hypertension. Additionally, a liver biopsy may be performed to confirm the extent of liver damage and determine the underlying cause of hepatic dysfunction.
In cases where fluid accumulation is significant, paracentesis, a procedure that involves extracting fluid from the abdominal cavity, may be performed. This procedure helps relieve discomfort and allows for further analysis of fluid composition to rule out infections or malignancies. Comprehensive diagnostic approaches enable healthcare providers to develop targeted treatment plans tailored to the severity and underlying cause of hepatic edema.
Treatment and Management Strategies
Managing hepatic edema requires addressing the underlying liver disease while implementing strategies to reduce fluid retention. Lifestyle modifications play a crucial role in improving liver health and minimizing swelling. Reducing sodium intake is one of the most effective dietary changes, as excessive sodium exacerbates fluid retention. Patients are advised to follow a low-sodium diet, avoiding processed foods and incorporating fresh, whole foods rich in nutrients.
Diuretics, such as spironolactone and furosemide, are commonly prescribed to help the body eliminate excess fluid. These medications work by promoting urine production and reducing fluid accumulation in tissues. However, diuretic use must be carefully monitored, as excessive dehydration or electrolyte imbalances can occur.
For individuals with significant ascites or severe swelling, therapeutic paracentesis may be performed to remove excess fluid. In advanced cases of cirrhosis, liver transplantation may be considered as a long-term solution. Patients with hepatic edema should also be monitored for potential complications, including spontaneous bacterial peritonitis (SBP), a life-threatening infection that can occur in ascitic fluid.
Preventative Measures and Lifestyle Considerations
Preventing hepatic edema involves proactive liver health maintenance. Limiting alcohol consumption is essential, as alcohol-related liver damage significantly contributes to fluid retention. Engaging in regular physical activity supports liver function by reducing the risk of fatty liver disease and promoting overall cardiovascular health.
Maintaining a healthy weight is also crucial, particularly for individuals at risk of NAFLD. Obesity is a major contributor to liver dysfunction, and weight management strategies, including balanced nutrition and regular exercise, can prevent disease progression. Additionally, staying hydrated while avoiding excessive fluid intake helps balance electrolytes and prevent further swelling.
For individuals with chronic liver conditions, regular medical check-ups are essential for monitoring liver function and detecting potential complications early. Vaccination against hepatitis A and B can also protect against viral infections that contribute to liver disease. By prioritizing liver health and implementing preventive measures, individuals can reduce the risk of hepatic edema and its associated complications.
Frequently Asked Questions (FAQ) About Hepatic Edema and Liver-Related Swelling
1. What causes swelling in the feet due to liver disease? Swelling in feet from liver disease, known as hepatic edema, is often caused by a combination of fluid retention and poor circulation. When liver function declines, it can lead to low levels of albumin, a protein that helps regulate blood volume and prevent fluid leakage into surrounding tissues. Additionally, increased pressure in the veins due to portal hypertension—a condition common in advanced liver disease—forces fluid out into the lower extremities. Many patients experience gradual swelling that worsens throughout the day, particularly if they remain standing or seated for long periods. Lifestyle modifications, such as elevating the legs and reducing sodium intake, can help manage the condition, but medical intervention is often necessary to address the underlying liver dysfunction.
2. How does liver disease contribute to facial swelling? Liver disease can cause facial swelling through a similar mechanism as swelling in the feet, primarily due to fluid retention and protein imbalances. When the liver fails to produce enough albumin, fluid can accumulate not only in the lower extremities but also in the face, leading to noticeable puffiness. In some cases, liver disease swollen face symptoms may be more prominent in the morning due to fluid redistribution during sleep. Certain liver conditions, such as cirrhosis, can also cause facial blood vessels to dilate, giving the face a flushed or swollen appearance. Managing facial swelling often requires addressing liver health through dietary changes, medication, and, in severe cases, medical procedures to remove excess fluid.
3. Are swollen feet always a sign of liver disease? Not necessarily—swollen feet can result from various conditions, including heart failure, kidney disease, and prolonged standing or sitting. However, when swelling in feet liver disease is present, it is typically accompanied by other symptoms, such as jaundice, fatigue, or abdominal swelling (ascites). Liver-related swelling tends to worsen over time and may not respond well to simple remedies like compression socks or increased movement. If swelling in the feet is persistent, occurs alongside liver dysfunction symptoms, or does not improve with elevation, a healthcare provider should be consulted to rule out hepatic edema as a cause.
4. How can hepatic edema be managed at home? Managing hepatic edema at home requires a multifaceted approach to reduce fluid buildup and support liver function. First, reducing salt intake is essential, as excess sodium can exacerbate fluid retention. Staying hydrated and engaging in light physical activity, such as walking, can help promote circulation and minimize swelling in feet from liver disease. Additionally, elevating the legs when resting and wearing compression stockings can help prevent fluid from pooling in the lower extremities. However, since hepatic edema is a symptom of underlying liver dysfunction, medical treatment aimed at improving liver health is the most effective way to address long-term swelling.
5. Can hepatic edema be reversed? The reversibility of hepatic edema depends on the severity of the underlying liver disease. If caught early, swelling in feet liver disease symptoms can improve with lifestyle changes, medication, and proper medical care. However, in cases of advanced liver disease, such as cirrhosis, the damage may be irreversible, requiring more aggressive interventions like diuretics or even liver transplantation. Regular monitoring by a healthcare provider and adherence to a liver-friendly diet and lifestyle can help slow disease progression and manage symptoms effectively.
6. Does liver disease swollen face indicate a severe condition? Facial swelling due to liver disease can indicate significant liver dysfunction, particularly if accompanied by other symptoms like jaundice, fatigue, or cognitive impairment (hepatic encephalopathy). A swollen face may be a sign that the body is struggling to regulate fluid balance and that liver function has declined significantly. While some swelling can be mild and manageable, persistent or severe swelling should prompt a medical evaluation to assess liver health. Treatments may include diuretics, lifestyle modifications, or addressing the underlying liver disease through targeted medical interventions.
7. What medical treatments are available for hepatic edema? Medical treatments for hepatic edema focus on reducing fluid retention and improving liver function. Diuretics, such as spironolactone or furosemide, may be prescribed to help the body eliminate excess fluid. In cases where fluid accumulation is severe, a procedure called paracentesis may be performed to remove excess fluid from the abdomen. Addressing the underlying cause of liver disease—whether through medication, dietary changes, or, in some cases, liver transplantation—is crucial for long-term management. Patients with hepatic edema should work closely with a healthcare provider to determine the best course of treatment.
8. Can lifestyle changes prevent swelling in the feet from liver disease? While lifestyle changes alone may not completely prevent swelling in feet liver disease cases, they can help minimize symptoms and slow disease progression. Reducing salt intake, staying hydrated, and engaging in regular physical activity can support circulation and reduce fluid retention. Avoiding alcohol and maintaining a balanced diet rich in protein and essential nutrients can also help support liver function. Additionally, regular medical check-ups can ensure that any worsening symptoms are addressed early, improving the chances of effective management.
9. How does diet impact hepatic edema? Diet plays a crucial role in managing hepatic edema, as certain foods can either worsen or alleviate fluid retention. A low-sodium diet is essential to prevent excessive fluid buildup, while adequate protein intake helps maintain albumin levels and reduce swelling. Processed foods, alcohol, and high-fat meals should be avoided, as they can strain the liver and exacerbate liver disease swollen feet symptoms. Incorporating potassium-rich foods, such as bananas and leafy greens, can help balance electrolytes and support healthy fluid regulation. Working with a nutritionist or healthcare provider can help tailor a diet plan that meets individual liver health needs.
10. When should someone seek medical help for swelling related to liver disease? Anyone experiencing persistent or worsening swelling in the feet, face, or abdomen should seek medical attention, especially if accompanied by other liver disease symptoms. Sudden increases in swelling, difficulty breathing, confusion, or severe fatigue may indicate worsening liver function and require immediate medical care. Since hepatic edema is often a sign of advanced liver disease, early intervention is crucial to prevent complications. Regular check-ups and proactive management can help individuals maintain a better quality of life while addressing liver health concerns. If swelling does not improve with home management strategies, a healthcare provider can assess the need for further treatment or intervention.
Conclusion: Addressing Hepatic Edema for Better Health
Hepatic edema is a significant complication of liver disease, characterized by swelling in the feet and face due to fluid retention. Understanding the underlying mechanisms, causes, and symptoms of this condition is crucial for effective management and prevention. Early detection through medical evaluation and lifestyle modifications can improve outcomes and enhance quality of life for individuals with liver disease. By adopting healthy habits, seeking timely medical intervention, and prioritizing liver function, individuals can take proactive steps to minimize fluid retention and maintain overall well-being.
swelling from liver disease, liver dysfunction fluid retention, cirrhosis and swollen feet, ascites and liver disease, chronic liver disease symptoms, how liver disease affects the body, portal hypertension complications, managing edema in liver disease, fatty liver disease swelling, alcoholic liver disease symptoms, hepatic dysfunction and swelling, liver cirrhosis swelling, detoxifying the liver naturally, liver disease weight gain, facial swelling liver disease, signs of liver disease, liver health and fluid balance, swollen feet due to liver, reducing liver disease swelling
Further Reading:
Brain and the Liver: Cerebral Edema, Hepatic Encephalopathy and Beyond
Brain Edema in Chronic Hepatic Encephalopathy
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.