Eating disorders are among the most complex and misunderstood mental health conditions affecting individuals today. Despite increasing awareness, the statistics reveal that these disorders remain pervasive and deeply rooted in American society. From adolescents navigating social pressures to adults grappling with lifelong struggles, eating disorders cross boundaries of age, gender, socioeconomic status, and ethnicity. In unpacking the current data, we gain insight not only into prevalence and treatment outcomes but also into societal trends and systemic gaps in care. Understanding the reality behind the numbers is essential for anyone interested in mindful eating, holistic wellness, or advocating for better mental health support.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
Defining Eating Disorders: A Clinical and Cultural Overview
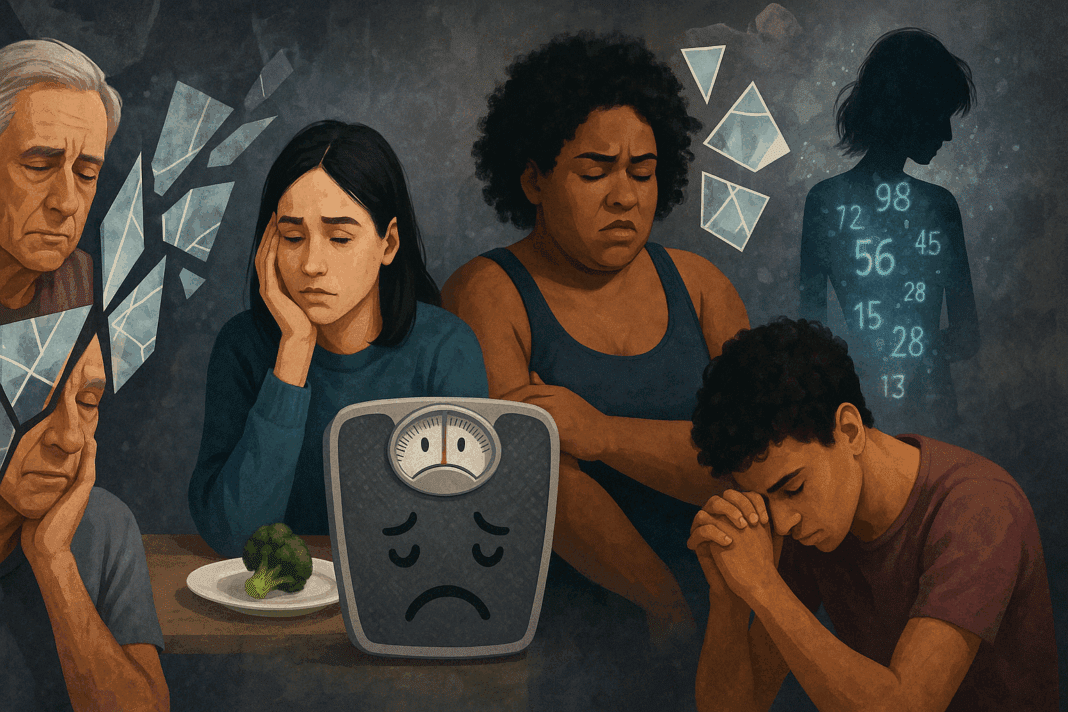
To truly grasp the implications of eating disorder statistics, one must first understand what these disorders are. Eating disorders (EDs) are psychiatric conditions characterized by severe disturbances in eating behaviors and related thoughts and emotions. The most recognized types of ED include anorexia nervosa, bulimia nervosa, and binge-eating disorder, though several other variants and subclinical presentations exist. When examining how many eating disorders are there, the answer includes not only the officially recognized diagnoses in the DSM-5 but also emerging classifications such as Avoidant/Restrictive Food Intake Disorder (ARFID), Other Specified Feeding or Eating Disorder (OSFED), and Night Eating Syndrome.
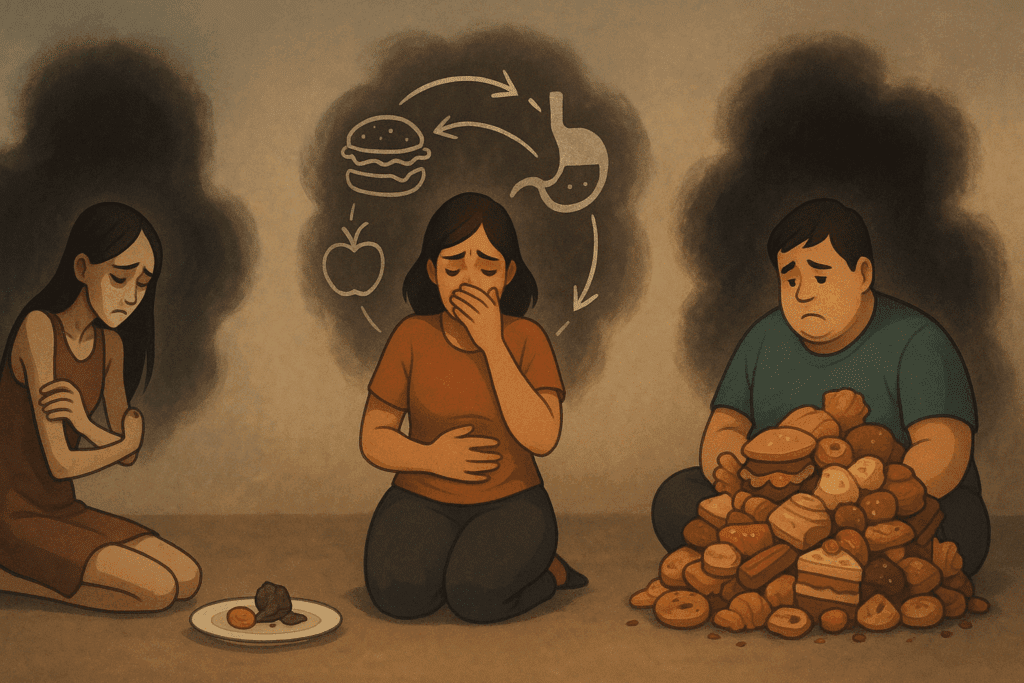
Each eating disorder name reflects distinct behavioral patterns and psychological underpinnings. Anorexia nervosa is marked by extreme food restriction and an intense fear of gaining weight, despite being underweight. Bulimia nervosa involves cycles of binge eating followed by compensatory behaviors such as vomiting or excessive exercise. Binge-eating disorder is characterized by episodes of excessive food intake without the purging that typically follows in bulimia. Knowing the types of ED and their nuances is critical for interpreting the broader eating disorder statistics available.
The Scope of the Problem: How Many People Have Eating Disorders?
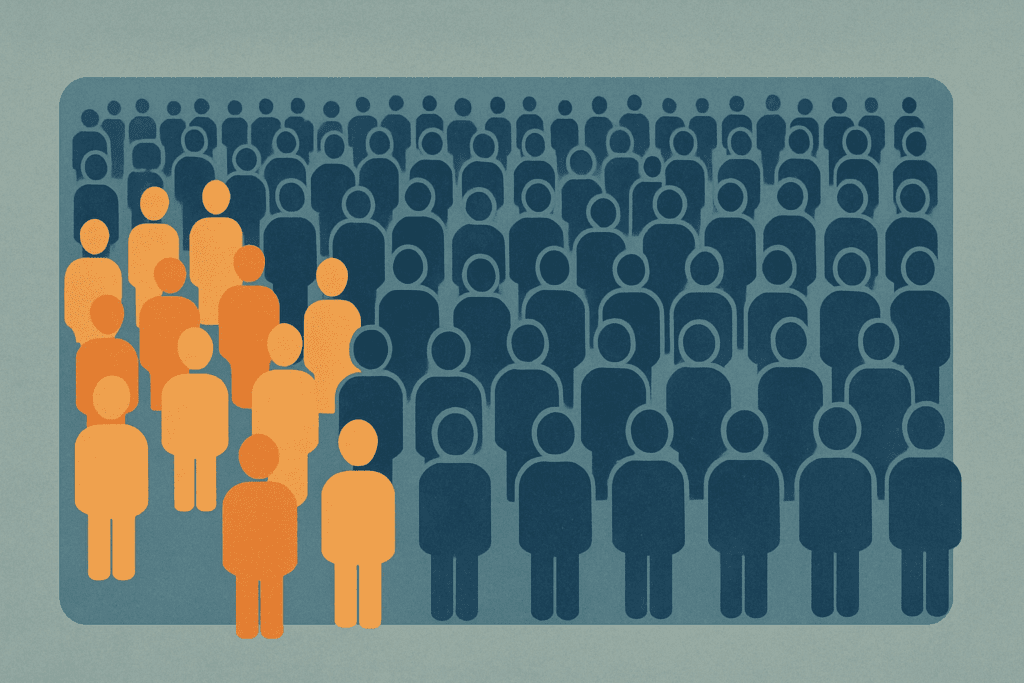
One of the most frequently asked questions in both clinical and public health circles is: how many people have eating disorders in the United States? According to current estimates from the National Association of Anorexia Nervosa and Associated Disorders (ANAD) and other research institutions, approximately 9% of the U.S. population will experience an eating disorder in their lifetime. This figure represents millions of individuals whose lives are affected by these conditions, highlighting the urgency of early detection, intervention, and support.
When considering what percent of people in the U.S. suffer from anorexia specifically, data suggests that roughly 0.9% of American women and 0.3% of men will meet the criteria for anorexia nervosa at some point. These anorexia statistics are particularly alarming given the high mortality rate associated with the disorder—among the highest of any mental illness. The statistics of bulimia tell a similarly concerning story, with prevalence rates estimated at 1.5% for women and 0.5% for men.
Which Eating Disorder Is Prominent in America?
While anorexia nervosa and bulimia nervosa are often spotlighted in media and research, the most common eating disorder in the U.S. is actually binge-eating disorder. This condition affects approximately 3.5% of women and 2% of men, surpassing the prevalence of both anorexia and bulimia. These statistics on most common eating disorders shed light on a public health issue that often goes unrecognized due to social stigma and limited awareness. Many individuals with binge-eating disorder may not seek treatment, believing their struggles do not constitute a “real” eating disorder.
The question of what eating disorder is prominent in America also prompts a closer examination of co-occurring mental health issues. Anxiety, depression, and trauma are frequently linked to eating disorders, complicating the clinical picture and often delaying effective intervention. The data suggests that eating disorders do not occur in isolation but are part of a larger pattern of emotional distress and psychological imbalance.
Gender and Age Trends: What the Data Tells Us
It is a common misconception that eating disorders predominantly affect teenage girls. While adolescent females do represent a significant portion of the diagnosed population, eating disorder stats reveal a broader demographic impact. Adult women, middle-aged individuals, and even seniors can experience disordered eating. Additionally, research shows rising rates among children under the age of 12, prompting serious concern among pediatricians and child psychologists.
A key resource in understanding these trends is the growing body of women eating disorder graphs, which illustrate longitudinal data on prevalence, diagnosis rates, and recovery outcomes. These visual tools often show spikes in eating disorder diagnoses during transitional life phases such as puberty, college, pregnancy, and menopause. This suggests that hormonal changes and social stressors may play a significant role in triggering or exacerbating ED symptoms.
Men, too, are increasingly recognized as vulnerable. Historically underdiagnosed and underrepresented in research, male eating disorders are finally receiving more attention. Current eating disorder statistics indicate that roughly one-third of individuals with an eating disorder are male, challenging outdated gender stereotypes and underscoring the need for inclusive screening and treatment protocols.

Analyzing Treatment Success: Do Eating Disorder Treatments Work?
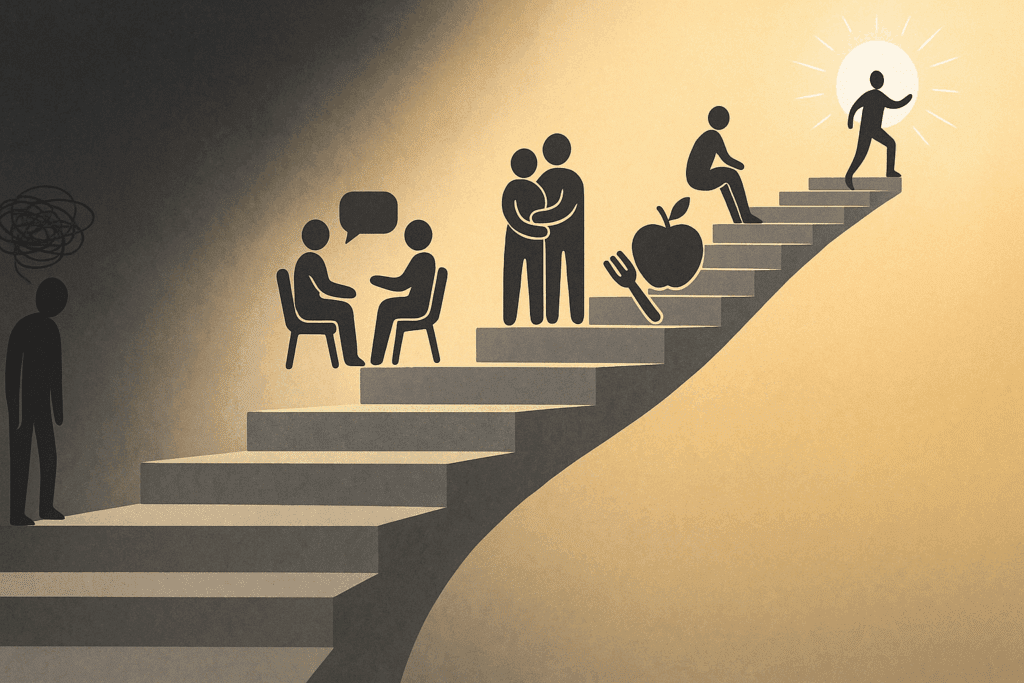
Given the serious nature of these conditions, a pressing concern remains: do treatments for eating disorders actually work? Fortunately, recent treatment for eating disorders work statistics are encouraging, though they also reveal significant challenges. Evidence-based therapies such as Cognitive Behavioral Therapy (CBT), Family-Based Treatment (FBT), and Dialectical Behavior Therapy (DBT) have demonstrated efficacy, particularly when initiated early and delivered by trained specialists.
However, treatment outcomes vary widely depending on factors such as age of onset, duration of illness, co-occurring disorders, and access to care. Studies show that full recovery is possible, especially with early intervention, but relapse rates remain high—up to 50% for some disorders. These sobering figures highlight the importance of ongoing support, comprehensive treatment plans, and long-term monitoring.
Accessibility also plays a crucial role. Many individuals never receive the care they need due to cost, stigma, or geographic limitations. Expanding insurance coverage and increasing the number of trained professionals are vital steps toward improving national recovery rates. By interpreting treatment for eating disorders work statistics within the broader context of healthcare accessibility, we gain a more nuanced understanding of what effective recovery truly entails.
The Cost of Silence: Social Stigma and Misconceptions
Beyond the clinical data, the societal response to eating disorders profoundly shapes outcomes. Stigma, misinformation, and cultural ideals often delay diagnosis and treatment. Many individuals hide their symptoms due to shame or fear of judgment. This silence can be deadly, particularly in cases of anorexia nervosa, where delayed treatment significantly increases the risk of long-term complications or death.
Media portrayals have historically glamorized thinness and equated self-worth with appearance, perpetuating harmful stereotypes. These narratives not only skew public perception but also influence healthcare policy and funding priorities. Eating disorder stats consistently show that early intervention leads to better outcomes, yet many people wait years before seeking help—if they seek help at all.
Education is one of the most effective tools for dismantling stigma. By sharing accurate information and amplifying diverse stories, we can shift the narrative from shame to support. Schools, workplaces, and healthcare providers all have a role to play in fostering environments where individuals feel safe disclosing their struggles and accessing care.
Emerging Trends and Future Directions in Eating Disorder Research
The landscape of eating disorder research is rapidly evolving, with new studies shedding light on genetic, neurological, and environmental contributors. Advances in brain imaging and genetic testing are helping scientists understand the biological underpinnings of disordered eating. These developments hold promise for personalized treatment approaches and early identification strategies.
Digital health tools, including virtual therapy and mobile apps, are also transforming how treatment is delivered. These innovations increase accessibility for individuals in rural or underserved areas, particularly relevant given the disparities in eating disorder statistics across geographic regions. Telehealth has shown particular efficacy in reaching young adults and adolescents who may feel more comfortable engaging in therapy from the privacy of their homes.
The future also lies in better data collection. While much progress has been made, questions like how many eating disorder are there or how many people have anorexia continue to elicit varied responses depending on methodology and population sampling. Establishing national registries, improving diagnostic criteria, and investing in longitudinal studies will yield more accurate prevalence data and inform policy decisions that align with actual needs.

Why Accurate Data Matters: From Awareness to Action
Understanding statistics of bulimia or interpreting anorexia nervosa statistics isn’t just an academic exercise—it’s a critical tool for advocacy and reform. Data informs funding decisions, influences public health campaigns, and shapes the training of medical professionals. Accurate statistics on most common eating disorders provide the evidence base needed to advocate for policy changes, such as increased insurance coverage for mental health or inclusion of eating disorder screenings in primary care settings.
Moreover, data empowers individuals. When people learn that millions of others share their struggles, the isolation of disordered eating begins to diminish. Awareness fosters community, and community fosters healing. It is only through a data-driven, empathetic, and inclusive approach that we can hope to reduce the prevalence of bulimia nervosa, anorexia, and other eating disorders in meaningful ways.
A Final Word on Eating Disorder Names, Labels, and Humanity
While statistics are essential, they must not overshadow the human stories behind the numbers. Every percentage point represents real lives, real pain, and real hope for recovery. It is easy to become desensitized to data points, but behind each mention of how many people have eating disorders or the prevalence of bulimia nervosa lies a person navigating one of the most difficult challenges of their life.
The terminology we use—whether clinical terms like anorexia nervosa or broader categories like types of ED—should serve to illuminate, not alienate. Compassionate language and inclusive dialogue can transform the way we approach mental health, encouraging more people to seek help without fear of judgment.
Frequently Asked Questions (FAQ): Understanding Eating Disorder Statistics and Trends in the U.S.
1. Why is it difficult to determine how many people have eating disorders in the U.S.?
Accurately measuring how many people have eating disorders is complicated by underreporting, stigma, and evolving diagnostic criteria. Many individuals struggling with disordered eating never receive a formal diagnosis due to limited access to care or fear of judgment. Additionally, differences in how studies define eating disorders can lead to inconsistent estimates, which makes answering questions like how many eating disorder are their or how many eating disorders are there more complex than they seem. Some people may not meet full diagnostic criteria but still suffer from significant impairment, which often excludes them from official eating disorder stats. Emerging research also shows that eating disorders frequently co-occur with other mental health conditions, which can mask or complicate detection.
2. What percent of people in the U.S. suffer from anorexia, and why might that number be underestimated?
When asking what percent of people in the U.S. suffer from anorexia, studies typically estimate between 0.3% and 0.9% of the population. However, this number may be lower than the reality due to diagnostic challenges. For instance, individuals with atypical anorexia exhibit all the psychological traits of anorexia nervosa but maintain a weight considered “normal” or higher, and thus may not be counted in official anorexia nervosa statistics. Furthermore, anorexia can manifest subtly, especially in high-functioning individuals who mask their symptoms behind socially accepted behaviors like clean eating or excessive exercise. These hidden cases mean that existing anorexia statistics likely underrepresent the actual prevalence.
3. How many eating disorders are there beyond the commonly discussed ones?
The question of how many eating disorders are there expands far beyond the traditional three. While anorexia nervosa, bulimia nervosa, and binge-eating disorder are the most well-known, mental health professionals now recognize several other types of ED. These include ARFID (Avoidant/Restrictive Food Intake Disorder), OSFED (Other Specified Feeding or Eating Disorder), Pica, and Rumination Disorder. OSFED alone encompasses many subtypes, capturing those who don’t meet strict diagnostic criteria but still experience serious symptoms. As our understanding of the human psyche deepens, clinicians are identifying new patterns of disordered eating, which continues to evolve the list of valid eating disorder names.
4. What eating disorder is prominent in America, and how does it impact treatment focus?
Despite media emphasis on anorexia and bulimia, the eating disorder that is most prominent in America is binge-eating disorder. This condition affects more individuals than anorexia and bulimia combined, according to recent statistics on most common eating disorders. Its high prevalence is reshaping treatment priorities, especially in community-based clinics and primary care settings. Unlike other disorders that often result in noticeable weight loss, binge-eating disorder can go undetected for years because individuals may appear healthy or overweight. This disconnect between visibility and prevalence makes it especially important for healthcare providers to incorporate screening for all types of ED, not just the ones associated with extreme weight changes.
5. What role do social media and cultural trends play in eating disorder statistics?
Eating disorder statistics are increasingly influenced by the digital age. Platforms like Instagram and TikTok often promote unrealistic beauty standards, glorify restrictive diets, or subtly endorse disordered behaviors. These trends are reflected in women eating disorder graphs, which show spikes in ED diagnoses during the rise of appearance-focused content. Social comparison theory suggests that individuals—particularly young women—are more likely to develop negative body image when repeatedly exposed to idealized bodies. These societal pressures exacerbate both the development and the persistence of eating disorders, making social media regulation and digital literacy vital components of public health strategy.
6. How are treatment for eating disorders work statistics used to inform healthcare policy?
Treatment for eating disorders work statistics play a critical role in shaping healthcare policy and insurance reimbursement guidelines. Policymakers often look at these figures to determine whether therapies like CBT, FBT, or nutritional counseling are cost-effective and should be covered under health plans. They also help prioritize funding for treatment programs that demonstrate long-term recovery success. Unfortunately, many insurance companies still place limits on mental health coverage, often demanding evidence from eating disorder stats before authorizing extended care. Improving transparency in treatment outcomes and refining what counts as “recovery” could make these statistics more impactful in advocating for systemic reform.
7. What can be learned from the statistics of bulimia that isn’t obvious from diagnostic criteria alone?
While diagnostic criteria for bulimia nervosa focus on bingeing and compensatory behaviors, the statistics of bulimia offer deeper insight into the condition’s psychosocial impact. For example, research shows that individuals with bulimia often experience higher rates of impulsivity, self-harm, and substance use. These associations aren’t always captured in clinical descriptions but emerge clearly in data trends and epidemiological studies. Furthermore, the prevalence of bulimia nervosa varies widely across age groups, suggesting that developmental and hormonal factors may play underexplored roles. When interpreting prevalence of bulimia nervosa, it’s essential to consider these multidimensional patterns that extend beyond calorie control or purging frequency.
8. Why do women eating disorder graphs matter for gender-specific research?
Women eating disorder graphs are more than just visual data—they provide a lens into the social, hormonal, and psychological dynamics influencing female health. These graphs often highlight critical life transitions such as puberty, pregnancy, and menopause as periods of increased vulnerability. Researchers also use this data to evaluate the intersection of gender and cultural norms, such as the expectation of thinness or the stigma surrounding emotional expression. While much progress has been made in recognizing male and non-binary ED experiences, women’s data remains vital for understanding the unique interplay between gender roles and mental health. Trends reflected in eating disorder stats specific to women also help guide development of targeted therapies.
9. What emerging trends could change how we classify and treat eating disorders?
The classification of eating disorders is likely to shift as neuroscience, artificial intelligence, and genetic testing continue to evolve. Innovations in brain imaging are beginning to map how specific neural pathways differ in individuals with various types of ED, which could lead to more precise diagnostic tools. For example, what we currently classify under broad eating disorder names might someday be segmented into neurologically distinct subtypes. These advancements could dramatically affect how many eating disorders are there in future medical literature. Additionally, early detection using machine learning algorithms might soon become part of standard screening, particularly in schools and pediatric clinics.
10. How can public education and early intervention shift eating disorder stats in a positive direction?
Improving public education about the warning signs of disordered eating is one of the most powerful strategies to reduce how many people have eating disorders in the future. Early intervention, particularly in schools, sports programs, and digital platforms, can lead to earlier diagnoses and better long-term outcomes. Eating disorder statistics show that the earlier a person receives treatment, the higher their chance of full recovery. When children and adolescents are educated on body positivity, media literacy, and emotional resilience, they are less likely to develop severe forms of disordered eating. As society continues to embrace mental health awareness, we may see a decline in concerning figures like anorexia statistics and a more hopeful shift in overall eating disorder stats.
Conclusion: Reflecting on Eating Disorder Statistics to Support a Healthier Lifestyle
Understanding eating disorder statistics in America is more than an academic endeavor; it is a necessary step toward cultivating a healthier, more mindful society. The data provides a window into the silent battles millions face, offering clarity about the prevalence, risk factors, and potential paths to recovery. From answering how many eating disorders are there to examining treatment for eating disorders work statistics, the insights gathered form a roadmap for prevention, education, and advocacy.
By recognizing what eating disorder is prominent in America and exploring the full spectrum of eating disorder names, we equip ourselves with the knowledge to support others—and ourselves—more compassionately. These figures are not abstract; they are the foundation for actionable change. Whether you’re a healthcare provider, educator, policymaker, or simply a concerned individual, understanding these numbers is the first step in creating a world where every person struggling with an eating disorder can access the care, respect, and hope they deserve.
Let the data not only inform but also inspire. The journey toward mental wellness begins with awareness, grows with understanding, and flourishes in community.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.