Endurance athletes—whether recreational runners, cyclists, or long-distance swimmers—require a finely tuned balance of nutrition, energy, and cardiovascular health. When managing chronic conditions like diabetes or heart disease, the stakes are even higher. Choosing the right diet is no longer a matter of preference; it’s essential for safe, effective performance. A diabetic heart healthy diet supports both stamina and health by stabilizing blood sugar, protecting arteries, and fueling sustained exertion.
Today, more people with chronic conditions are embracing physical activity not just for enjoyment, but to improve long-term wellness. However, nutrition must adapt accordingly. For individuals living with diabetes and those at risk of cardiovascular complications, fueling the body correctly requires a tailored plan. A diabetes and heart disease diet is designed to reduce inflammation, regulate insulin response, and protect the heart during physical stress. When aligned with an endurance-focused lifestyle, this dietary approach can help athletes of all levels perform better while managing or even reversing risk factors associated with their conditions.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice
The Science Behind Endurance, Blood Sugar, and Cardiovascular Health
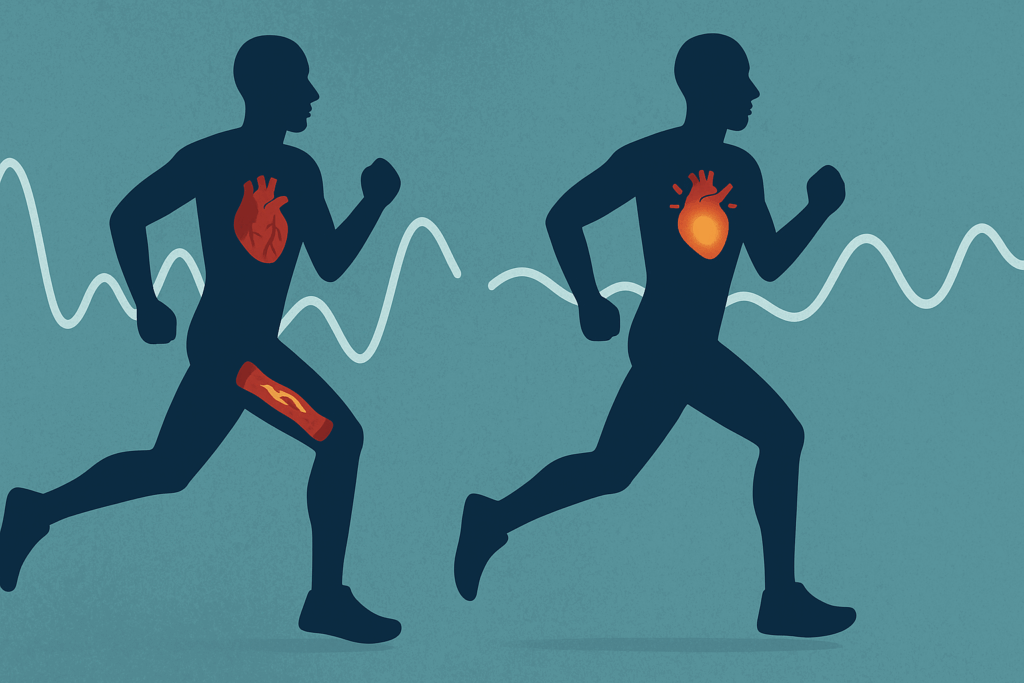
Endurance training places significant metabolic demands on the body, especially when it comes to glucose regulation. Muscles rely heavily on glucose for fuel, but in those with diabetes, insulin resistance can impair this uptake, making it difficult to maintain energy. The danger isn’t just fatigue—it’s the increased risk of hypoglycemia during exercise or dangerous post-workout spikes. A diabetic heart healthy diet addresses these challenges by providing a steady stream of low-glycemic carbohydrates that prevent blood sugar crashes without overloading the body with refined sugars.
Simultaneously, heart health plays a foundational role in oxygen transport and muscular endurance. Narrowed arteries, high blood pressure, and elevated cholesterol levels all compromise the cardiovascular system’s ability to support exercise. Fortunately, food can act as medicine. A diet that emphasizes heart-friendly fats, fiber-rich vegetables, and lean proteins can reduce LDL cholesterol, lower inflammation, and keep blood vessels flexible and efficient. When athletes combine endurance training with a diabetes and heart disease diet, the result is improved circulatory function and longer-lasting energy.
These benefits extend well beyond the gym or race track. Improved blood sugar control and better cardiac output support cognitive clarity, immune function, and mood—key elements for anyone pursuing long-term athletic goals while managing chronic illness.

Building the Foundation: What Makes a Diabetic Heart Healthy Diet?
The ideal diabetic heart healthy diet isn’t about rigid restrictions; it’s about making thoughtful, strategic choices that support metabolic efficiency and cardiovascular wellness. The cornerstone of this dietary pattern is a focus on whole, minimally processed foods—especially complex carbohydrates such as oats, brown rice, quinoa, and legumes. These foods provide sustained energy without triggering insulin spikes, making them ideal for pre- and post-workout meals.
Protein plays a central role in recovery and muscle maintenance, particularly for those training consistently. Lean options like chicken, turkey, tofu, eggs, and fish offer essential amino acids without the saturated fat found in red meat. These proteins also help regulate post-meal blood sugar, an important consideration for individuals with diabetes. For heart health, fatty fish like salmon and sardines are excellent sources of omega-3 fatty acids, which reduce inflammation and help regulate blood pressure.
Healthy fats—such as those found in avocados, nuts, seeds, and olive oil—should also be embraced. They provide long-lasting energy, promote satiety, and help absorb fat-soluble vitamins that support immune function and muscle repair. Just as importantly, they support vascular health by reducing triglycerides and supporting a balanced lipid profile.
Fresh fruits and vegetables round out this dietary framework, offering fiber, vitamins, minerals, and antioxidants that support recovery and cellular health. While fruit should be consumed in moderation for those with blood sugar concerns, berries, apples, and citrus fruits are often well-tolerated and provide important phytonutrients.
How This Diet Enhances Athletic Performance
While much of the emphasis on a diabetic heart healthy diet focuses on disease prevention and management, it also directly enhances athletic performance. Stable blood sugar means more consistent energy output, allowing athletes to perform at higher levels for longer durations without fatigue. It also reduces the risk of dizziness, brain fog, or energy crashes mid-exercise—issues that can not only limit training but pose safety risks.
The cardiovascular benefits of this diet are equally profound. Improved blood flow translates to better oxygen delivery and waste removal from working muscles. This allows athletes to recover more efficiently and train more frequently, both of which are essential for endurance gains. Foods that reduce systemic inflammation—like leafy greens, berries, turmeric, and fatty fish—help mitigate the oxidative stress associated with long workouts, lowering the risk of injury and muscle breakdown.
Cognitive endurance also receives a boost. Stable glucose supports neurotransmitter balance and focus, which is critical during long training sessions or competitions that demand mental as well as physical stamina. Athletes report better concentration, fewer mood swings, and more resilience under stress when following a diabetes and heart disease diet designed with performance in mind.
Tailoring the Diet for Training Cycles and Individual Needs
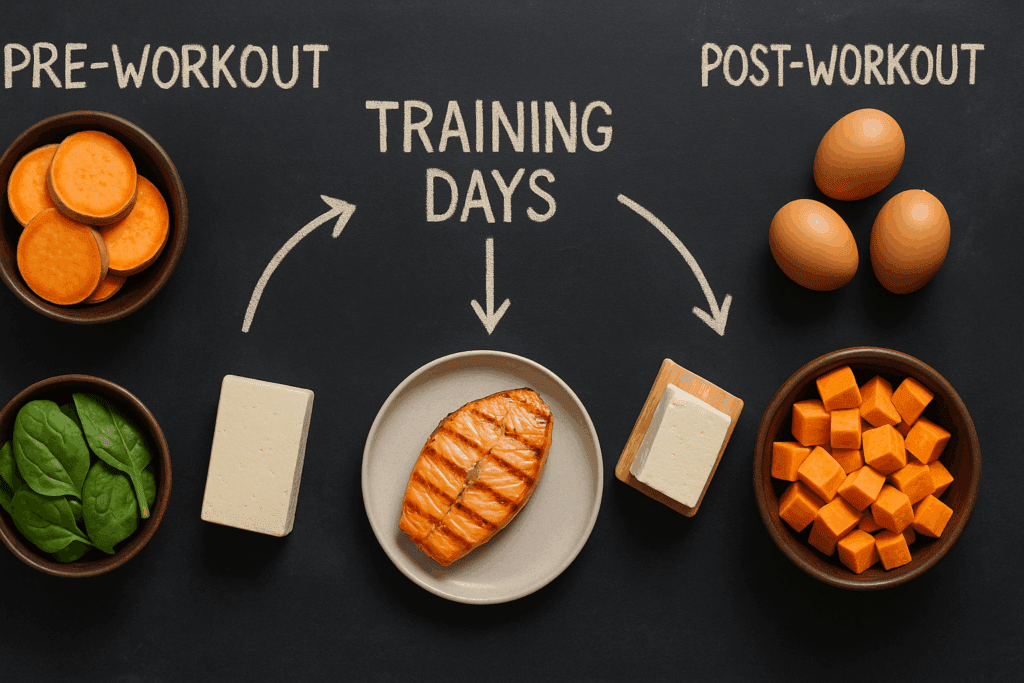
No two athletes are exactly alike, and the same is true for people managing chronic conditions. A successful diabetic heart healthy diet must be adapted based on training volume, intensity, and goals. During periods of heavy training, carbohydrates may need to be increased to maintain glycogen stores—but they should come from slow-burning sources. Adding extra servings of lentils, whole grains, or starchy vegetables like sweet potatoes can help meet this need.
Pre-workout meals should emphasize a balance of low-glycemic carbs and protein to maintain energy without spiking blood sugar. Post-workout nutrition is critical for recovery and should include lean protein, a moderate amount of carbohydrate, and hydration. For example, a post-run meal might include grilled salmon, quinoa, sautéed spinach, and a glass of unsweetened almond milk with cinnamon.
Some individuals may benefit from advanced strategies like intermittent fasting or carbohydrate periodization—but these must be approached with caution and professional guidance, particularly when managing diabetes. Blood sugar monitoring, whether through finger sticks or continuous glucose monitors, can help fine-tune meal timing and content.
It’s also important to factor in other medical conditions. Individuals with kidney disease may need to limit protein or potassium-rich foods. Those with high blood pressure must manage sodium intake carefully. This is where a registered dietitian or sports nutritionist becomes invaluable—helping to create a plan that supports performance while keeping the individual’s health history front and center.

The Psychological and Lifestyle Dimension of Nutrition
Beyond macronutrients and meal timing lies an often overlooked component of endurance nutrition: the emotional and psychological aspects of food. Committing to a diabetes and heart disease diet while training for an event can feel restrictive or overwhelming without the right mindset. But with support and planning, it becomes a sustainable lifestyle rather than a temporary challenge.
Stress, poor sleep, and negative self-talk all have measurable impacts on blood sugar control and heart health. Cortisol, the body’s stress hormone, raises blood sugar and contributes to fat storage, particularly around the abdomen—a risk factor for heart disease. Incorporating stress management techniques like mindfulness, yoga, or nature walks can improve both mental well-being and metabolic outcomes.
Sleep is equally critical. It is during deep sleep that the body repairs itself, regulates insulin, and recharges for the next day’s activities. Diet plays a role here too. Foods high in magnesium—like legumes, leafy greens, and seeds—can help promote restful sleep, while avoiding caffeine and sugar near bedtime supports circadian rhythm alignment.
Social connection also impacts dietary success. Athletes often do better when their family, training partners, or coaches understand and support their dietary needs. Sharing meals, prepping food together, or participating in nutrition-focused groups creates accountability and helps individuals stay on track, especially during periods of fatigue or temptation.
Partnering with Experts for Safe and Effective Outcomes
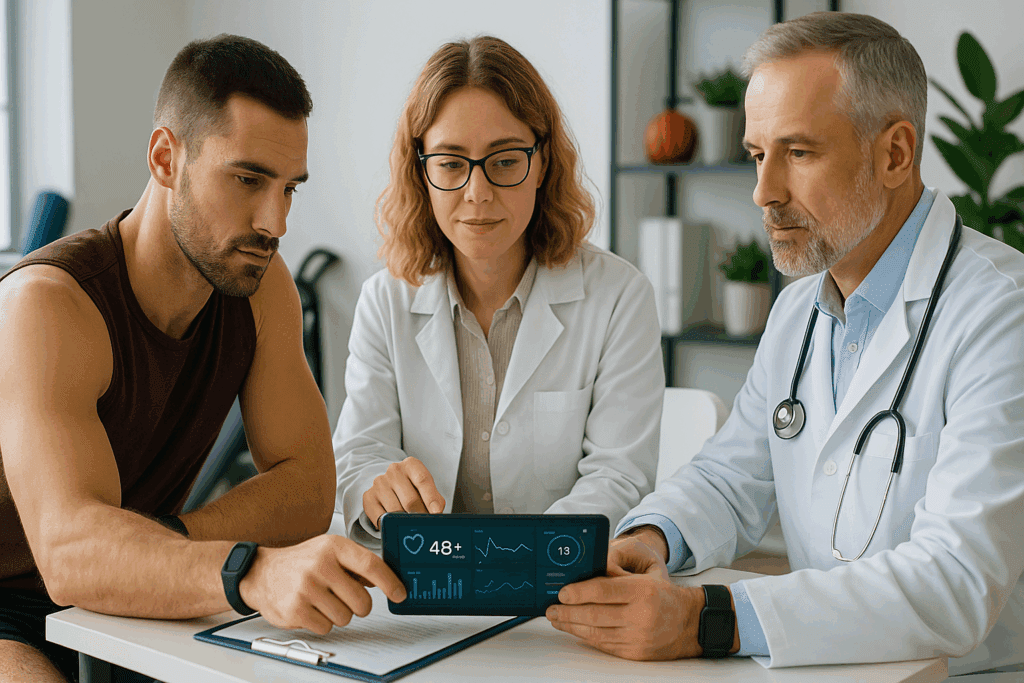
Even the most informed athlete can benefit from professional guidance. For those managing chronic illness, the stakes are higher, and small mistakes can have big consequences. Working with healthcare professionals—endocrinologists, cardiologists, registered dietitians, and certified exercise physiologists—ensures that dietary choices are aligned with medication needs, lab results, and performance goals.
Tools like continuous glucose monitors (CGMs) provide real-time data that can help fine-tune dietary and training strategies. Athletes can observe how certain foods affect their performance and recovery, making informed adjustments with expert oversight. Lab tests such as cholesterol panels, A1C levels, and inflammatory markers can help track progress and identify dietary blind spots.
Regular check-ins with a dietitian can also help troubleshoot challenges, whether it’s boredom with meals, issues with nutrient timing, or adapting recipes for better glycemic control. This level of personalization helps turn a general diabetic heart healthy diet into a dynamic, individualized performance plan.
Frequently Asked Questions (FAQ): Diabetic Heart Healthy Diet and Endurance Nutrition
1. Can endurance athletes with diabetes safely follow a high-carb diet?
Yes, but it requires careful planning. Endurance athletes typically rely on carbohydrates for sustained energy, but those managing diabetes must focus on low-glycemic options. A diabetic heart healthy diet can include high-quality carbohydrates like legumes, oats, and sweet potatoes that offer sustained energy without causing blood sugar spikes. Rather than following a traditional high-carb model, athletes can benefit from nutrient periodization—timing carbs around workouts when insulin sensitivity is naturally higher. By strategically incorporating carbs into a balanced diabetes and heart disease diet, performance can be optimized without compromising metabolic control.
2. How does stress impact the effectiveness of a diabetic heart healthy diet for endurance training?
Stress is often overlooked, but it can significantly disrupt blood sugar regulation and cardiovascular function. Elevated cortisol levels interfere with insulin sensitivity and may increase cravings for high-sugar foods, undermining a diabetes and heart disease diet. Chronic stress also raises blood pressure and heart rate, placing additional strain on an already vulnerable cardiovascular system. Incorporating stress management techniques—such as breathwork, cognitive behavioral therapy, or nature exposure—can improve the overall success of a diabetic heart healthy diet by aligning physiological and emotional resilience. Athletes who manage stress effectively are more likely to adhere to their nutrition plans and recover faster.
3. Are there new technologies that can enhance the management of a diabetes and heart disease diet during endurance training?
Absolutely. Continuous glucose monitors (CGMs) have revolutionized how athletes with diabetes manage their blood sugar in real time. These devices help users identify how specific foods and exercise routines impact glucose levels, enabling better decisions within a diabetic heart healthy diet. Some CGMs can be paired with mobile apps to provide alerts during endurance events, minimizing the risk of hypoglycemia. Additionally, wearable tech that tracks heart rate variability (HRV) can offer insights into cardiovascular stress and recovery, further informing dietary adjustments. The integration of these tools makes it easier to personalize a diabetes and heart disease diet based on real-world data.
4. What role do supplements play in supporting a diabetic heart healthy diet for athletes?
While food should be the foundation of any nutrition strategy, certain supplements can complement a diabetic heart healthy diet—especially when nutrient needs are elevated due to training. Magnesium and chromium may support blood sugar regulation, while omega-3 fatty acids offer anti-inflammatory benefits that protect heart health. Athletes might also consider CoQ10, which supports mitochondrial energy production and cardiovascular endurance. However, supplementation should always be approached with guidance from a healthcare provider, particularly in the context of a diabetes and heart disease diet where nutrient interactions with medications must be considered.
5. Can a diabetes and heart disease diet support muscle growth as well as endurance?
Yes, with the right balance of macronutrients. Many assume that a diabetic heart healthy diet is too restrictive to support muscle development, but this is a misconception. Including adequate protein from sources like eggs, tofu, and fish, along with strength training, allows for lean muscle gains without destabilizing blood sugar. Consuming protein in tandem with low-glycemic carbohydrates post-exercise enhances muscle repair while adhering to the principles of a diabetes and heart disease diet. Strategic meal timing and individualized planning make it entirely possible to build strength and endurance concurrently.
6. How can cultural or social eating habits be adapted to fit a diabetic heart healthy diet?
Cultural and social contexts play a large role in eating behavior, and adapting traditional dishes is both possible and empowering. For example, rice-heavy meals can be balanced with fibrous vegetables and lean proteins, or replaced with lower-glycemic grains like barley or quinoa. Family gatherings or holidays often revolve around food, so preparing diabetes and heart disease diet-compliant alternatives ensures inclusion without sacrifice. Spices, herbs, and traditional cooking methods can often remain intact, allowing individuals to honor their heritage while maintaining health. With education and creativity, a diabetic heart healthy diet can be both culturally respectful and medically sound.
7. What are common mistakes to avoid when starting a diabetes and heart disease diet for endurance?
One common mistake is underfueling before and after workouts, leading to blood sugar imbalances and poor recovery. Some individuals mistakenly cut all carbohydrates, which can impair endurance capacity and mood. Another error is over-relying on “diabetic” or “heart-healthy” packaged foods, which may contain additives or hidden sugars. Neglecting hydration and electrolyte balance—especially important for heart function—is another pitfall. A successful diabetic heart healthy diet emphasizes real, whole foods, personalized macronutrient ratios, and mindful timing based on training demands.
8. How long does it take to see benefits from switching to a diabetic heart healthy diet?
Improvements in energy levels and blood sugar stability can appear within the first one to two weeks, particularly if the transition involves reducing added sugars and processed foods. Cardiovascular improvements, such as lower blood pressure or cholesterol, typically take longer—around six to twelve weeks. Performance gains often align with this timeline, especially when combined with consistent endurance training. However, benefits from a diabetes and heart disease diet are cumulative, building over months and years as the body adapts to sustained nourishment. The key is consistency, not perfection, and tracking metrics like resting heart rate, glucose variability, and perceived exertion can offer early motivation.
9. Is it possible to follow a diabetic heart healthy diet on a budget?
Yes, and it’s more accessible than many assume. Staples like oats, lentils, canned sardines, eggs, and frozen vegetables are nutrient-dense and affordable. Planning meals in advance and buying in bulk can significantly reduce costs while supporting the guidelines of a diabetes and heart disease diet. Cooking at home instead of relying on takeout or processed snacks also reduces expenses and improves nutritional quality. With a little planning and flexibility, a diabetic heart healthy diet can be both budget-friendly and performance-enhancing.
10. What does the future look like for diabetic heart healthy diets in sports nutrition?
The future of sports nutrition is increasingly personalized, and the diabetic heart healthy diet is at the forefront of this evolution. Advances in nutrigenomics—how individual genes affect nutrient metabolism—may soon allow for ultra-tailored diets that support both heart health and blood sugar management. Additionally, the rise of plant-based endurance athletes is driving innovation in diabetes and heart disease diet strategies that are sustainable and performance-oriented. Research is also exploring how gut microbiome health intersects with metabolic and cardiovascular outcomes, suggesting that fermented foods and probiotics may become a larger focus. As science advances, the diabetic heart healthy diet will become more nuanced, adaptive, and essential in the conversation around longevity and athletic success.
Conclusion: Embracing Nutrition as the Key to Endurance and Heart Health
In a world where chronic diseases like diabetes and heart disease are increasingly common, the ability to thrive in endurance sports is not just possible—it’s empowering. A thoughtfully constructed diabetic heart healthy diet offers more than just disease prevention; it provides the fuel for athletic achievement, cognitive clarity, emotional balance, and lifelong vitality.
This way of eating is not a restriction but a strategy—one that celebrates whole foods, supports peak performance, and protects the body’s most vital systems. For anyone managing blood sugar or cardiovascular risk, the right nutrition plan transforms the body into an efficient, resilient machine. With each smart meal choice, individuals take control of their health journey, optimizing not only their athletic goals but their quality of life.
Ultimately, the fusion of performance training and a diabetes and heart disease diet marks a shift from simply surviving with chronic illness to truly thriving. With education, support, and intention, the path to greater endurance and stronger heart health becomes clear, achievable, and deeply rewarding.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
The importance of exercise for glycemic control in type 2 diabetes