Aging is often accompanied by a gradual decline in cardiovascular function, a process that many accept as inevitable. However, emerging science is challenging this assumption, particularly in the field of endurance and stamina training. As researchers dig deeper into the mechanisms of heart disease and the effects of aging, a growing body of evidence suggests that specific types of physical activity, especially endurance training, may offer a powerful buffer against the development of coronary artery disease (CAD). This revelation has major implications not only for those who are aging but also for healthcare providers seeking proactive strategies to maintain cardiovascular health well into the later decades of life. Understanding how age and coronary artery disease intersect, and what can be done to mitigate the risks, is an essential step toward building a longer, healthier life.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice
The Aging Heart: Why Cardiovascular Risk Increases Over Time
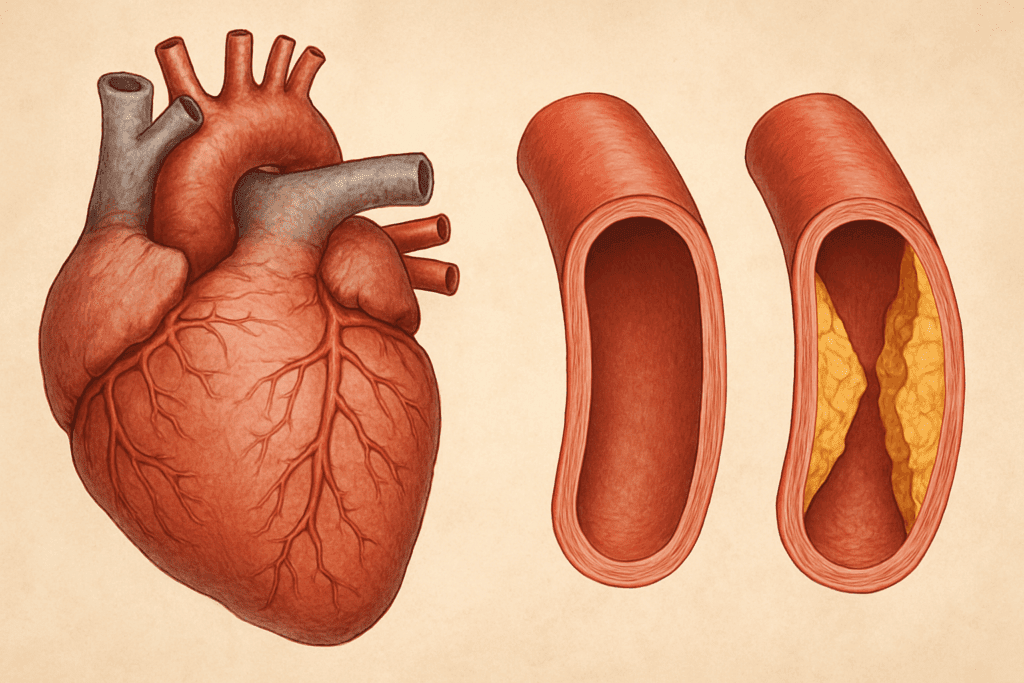
As we age, our cardiovascular system undergoes a series of structural and functional changes. The elasticity of blood vessels decreases, the walls of arteries thicken, and the heart muscle itself may stiffen. These changes contribute to higher systolic blood pressure, reduced maximum heart rate, and decreased cardiac output during exertion. All these factors elevate the risk of developing heart-related conditions, particularly coronary artery disease, which occurs when the arteries supplying blood to the heart become narrowed or blocked due to plaque buildup.
The term “aging heart disease” is not a clinical diagnosis per se, but rather a description of the cumulative effects of aging on the heart that can lead to disease. It includes a higher incidence of arrhythmias, heart failure, and ischemic heart disease among older adults. The association between age and coronary artery disease is particularly strong because the progression of atherosclerosis—a slow buildup of cholesterol-laden plaques—tends to accelerate with age. The longer one lives, the more likely these deposits are to impair blood flow to the heart, increasing the risk of heart attacks and other serious complications.
Inflammation, oxidative stress, and endothelial dysfunction play significant roles in the age-related progression of CAD. These processes are exacerbated by sedentary behavior, poor diet, smoking, and other lifestyle factors. However, emerging data suggest that endurance exercise may counteract many of these effects, not only preserving cardiovascular function but also reversing some of the damage previously thought to be permanent.

Understanding Endurance Training: What It Involves and Why It Matters
Endurance training, often referred to as aerobic exercise, encompasses activities that elevate the heart rate and maintain it over an extended period. Running, cycling, swimming, brisk walking, and rowing are all prime examples. What sets endurance training apart from other forms of exercise, such as strength training or high-intensity interval training (HIIT), is its sustained engagement of large muscle groups, which boosts oxygen utilization and cardiovascular efficiency.
The benefits of endurance training extend well beyond improved athletic performance. For aging individuals, endurance training can significantly increase mitochondrial density in cardiac and skeletal muscle cells, enhance endothelial function, and reduce systemic inflammation. These adaptations are critical for mitigating the impact of aging heart disease. Research indicates that older adults who engage in regular endurance training exhibit better arterial compliance, improved lipid profiles, and reduced markers of systemic inflammation compared to their sedentary counterparts.
Additionally, endurance training promotes angiogenesis—the formation of new blood vessels—which can help bypass blockages in coronary arteries and improve perfusion to cardiac tissue. These physiological changes collectively contribute to a decreased likelihood of developing or exacerbating coronary artery disease. Thus, endurance training stands out as a scientifically validated intervention for addressing the complex relationship between age and coronary artery disease.
Endurance Training and Its Protective Mechanisms Against Coronary Artery Disease
One of the most compelling reasons endurance training is being recommended as a protective strategy against CAD is its multifactorial impact on cardiovascular risk factors. First, endurance exercise has a potent effect on lipid metabolism. Regular aerobic activity increases levels of high-density lipoprotein (HDL) cholesterol—the so-called “good” cholesterol—while reducing low-density lipoprotein (LDL) cholesterol and triglycerides. These changes play a significant role in slowing the progression of atherosclerosis.
Second, endurance training has a well-documented effect on blood pressure regulation. By improving arterial elasticity and endothelial function, regular aerobic exercise can lead to long-term reductions in both systolic and diastolic blood pressure. For aging individuals, who are often dealing with hypertension or prehypertensive states, this benefit cannot be overstated.
Another crucial mechanism involves glucose metabolism. Endurance exercise enhances insulin sensitivity and improves glucose uptake in muscle tissues, thereby reducing the risk of type 2 diabetes—a major risk factor for coronary artery disease. This is particularly important for older adults, who are more susceptible to metabolic disorders that compound cardiovascular risk.
Finally, endurance training stimulates the production of nitric oxide, a molecule that relaxes blood vessels and promotes better blood flow. Nitric oxide availability tends to decline with age, contributing to endothelial dysfunction and arterial stiffness. By upregulating nitric oxide synthesis, endurance exercise helps maintain vascular health and reduces the risk of cardiac events.

Age-Specific Considerations for Endurance Training
While the benefits of endurance training are well-established, it is important to recognize that older adults may face specific challenges when beginning or maintaining a training regimen. Joint issues, preexisting conditions, and reduced exercise tolerance can make high-impact activities difficult. However, the beauty of endurance training lies in its adaptability. Activities such as walking, swimming, and cycling can be modified to suit different fitness levels and physical limitations, making them accessible even to individuals with limited mobility or chronic conditions.
One of the key strategies for success is gradual progression. Starting with low-intensity activities and slowly increasing duration and intensity over weeks or months can help reduce the risk of injury and improve long-term adherence. Consulting with a healthcare provider or exercise physiologist can also help create a personalized plan that accounts for individual health status, medication use, and fitness goals.
Moreover, consistency is more important than intensity when it comes to reaping the cardiovascular benefits of endurance training. Even moderate activity performed regularly—such as brisk walking for 30 minutes a day, five days a week—can yield substantial improvements in heart health and help counter the effects of aging heart disease.
Scientific Evidence Supporting Endurance Training for Aging Hearts
A growing number of longitudinal studies and randomized controlled trials support the notion that endurance training can slow or even reverse some of the cardiovascular changes associated with aging. In a landmark study published in the Journal of the American College of Cardiology, researchers found that lifelong endurance athletes had significantly greater arterial compliance, lower coronary artery calcium scores, and superior heart rate variability compared to age-matched sedentary peers.
Another study, published in Circulation, demonstrated that individuals over the age of 60 who engaged in six months of structured endurance training experienced marked improvements in VO2 max, resting blood pressure, and left ventricular function. These improvements are particularly noteworthy given that VO2 max—a measure of the body’s ability to use oxygen during exercise—is a strong predictor of mortality in older adults.
Importantly, these benefits were observed across different demographics, including women and individuals with preexisting cardiovascular conditions. This reinforces the idea that age and coronary artery disease are not fixed outcomes but can be modified through targeted, evidence-based interventions like endurance training. As such, incorporating regular aerobic exercise into daily life represents a low-cost, high-reward strategy for enhancing longevity and quality of life.

Integrating Endurance Training into Everyday Life
For many people, especially those juggling work, caregiving responsibilities, or chronic health issues, the idea of adding regular endurance training into their routine may seem daunting. However, there are numerous ways to integrate aerobic activity into daily life without it feeling like a burden. Walking meetings, weekend hikes, dance classes, or cycling to work are just a few examples of how endurance training can be folded into regular activities.
Technology can also play a supportive role. Fitness trackers, mobile apps, and wearable heart rate monitors can provide real-time feedback and motivation, helping individuals track progress and stay committed to their fitness goals. Group classes or walking clubs can add a social component that enhances accountability and enjoyment, making it more likely that the activity becomes a sustainable part of one’s lifestyle.
Importantly, the goal should not be perfection but progress. Even small increments of aerobic activity can contribute to improved cardiovascular health over time. Encouragingly, research shows that the benefits of endurance training are cumulative—meaning the more consistently you engage in it, the greater the protective effects against aging heart disease.
What Healthcare Professionals Should Know
Healthcare providers play a pivotal role in guiding patients toward cardiovascular health, especially as they age. While prescribing medications for cholesterol, blood pressure, and glucose management remains important, incorporating exercise prescriptions into patient care can yield synergistic benefits. Providers should feel empowered to discuss endurance training as a validated, science-backed intervention that addresses the root causes of age-related cardiovascular decline.
Incorporating questions about physical activity into routine checkups, offering referrals to cardiac rehabilitation or physical therapy, and recommending community resources can all help patients take the first steps toward an active lifestyle. For patients already managing coronary artery disease, supervised endurance training programs can provide a safe environment to rebuild stamina and improve heart function.
Medical education should also emphasize the role of exercise physiology in preventing and treating chronic disease. By expanding the clinical toolkit to include lifestyle medicine, healthcare professionals can offer more comprehensive and effective care, particularly for aging populations at heightened risk for cardiovascular disease.
Frequently Asked Questions (FAQ): Endurance Training and Heart Health in Aging
1. Can endurance training actually reverse some signs of aging heart disease? Yes, emerging research suggests that endurance training may help reverse certain physiological changes associated with aging heart disease, though not in a curative sense. It primarily works by improving cardiovascular efficiency, restoring endothelial function, and promoting mitochondrial rejuvenation, all of which slow down the heart’s aging process. While age-related structural damage such as advanced arterial calcification may not be fully reversible, the functional improvements in oxygen delivery and heart rate variability are significant. These changes can enhance not only longevity but also the quality of life in older adults. Understanding how to apply endurance principles safely is key to gaining these benefits.
2. What role does endurance training play in mental health for aging adults with coronary risk? The psychological benefits of endurance training are substantial and often overlooked in discussions about aging heart disease. Regular aerobic activity helps regulate cortisol levels, reduces anxiety, and improves sleep, which in turn positively impacts heart rate and blood pressure regulation. For individuals facing the emotional toll of age and coronary artery disease diagnoses, endurance exercise can restore a sense of agency and reduce feelings of helplessness. Group-based endurance programs also offer social engagement, an important factor in mental and cardiovascular health for seniors. Thus, the mental and emotional resilience gained through endurance training is a powerful complement to its physical benefits.
3. Are there technological tools that support endurance training for those with aging heart disease? Absolutely. The rise of wearable fitness devices has revolutionized how older adults manage their cardiovascular health. Smartwatches and fitness trackers can monitor heart rate zones, detect arrhythmias, and provide feedback on exertion levels—allowing individuals with aging heart disease to train safely and efficiently. Some advanced tools even sync with telehealth platforms, enabling remote cardiac rehabilitation programs. This technology empowers patients by offering data-driven insights into their exercise routines, promoting consistency and safety for those managing age and coronary artery disease.
4. How can someone with joint pain safely engage in endurance training to protect their heart? Joint pain is a common barrier for older adults aiming to prevent or manage aging heart disease through exercise. Low-impact endurance options such as aquatic aerobics, elliptical machines, and recumbent bikes provide cardiovascular benefits while minimizing joint strain. These activities still stimulate circulation and improve heart function, making them ideal for people with arthritis or past injuries. It’s also advisable to work with a physical therapist or certified trainer familiar with age and coronary artery disease limitations. They can create a personalized program that reduces pain while maximizing cardiovascular gains.
5. What are some overlooked indicators that endurance training is improving heart health in older adults? Beyond the obvious markers like lower blood pressure or resting heart rate, endurance training offers subtler signs of improved heart health. Enhanced thermoregulation, improved sleep quality, and increased post-exercise recovery rates can all reflect a more efficient cardiovascular system. Older adults may also notice better digestion, reduced breathlessness during daily tasks, and improved skin tone due to better circulation. These less-discussed indicators point to improved vascular and autonomic function—essential in managing aging heart disease. Recognizing these signs reinforces motivation to maintain an endurance routine.
6. How does endurance training influence medication needs for age and coronary artery disease? In many cases, consistent endurance training can reduce the need for certain cardiovascular medications, especially those for hypertension, cholesterol management, and insulin regulation. Improved vascular function and metabolic control often lead physicians to lower dosages over time. However, adjustments should never be made without medical supervision. For patients with age and coronary artery disease, regular follow-ups allow providers to monitor changes in biomarkers and adjust treatment plans accordingly. The synergy between exercise and pharmacological therapy often results in better long-term outcomes with fewer side effects.
7. Are there any risks of endurance training worsening aging heart disease if done incorrectly? Yes, when done improperly, endurance training can pose risks—especially for those with advanced cardiovascular conditions. Overtraining, insufficient recovery, or ignoring warning signs like chest pain or dizziness can exacerbate underlying issues. This is why medical clearance and gradual progression are essential components of any exercise plan for those managing age and coronary artery disease. Working with professionals who understand cardiac physiology can ensure that the training is both safe and effective. The goal is to harness the protective benefits of endurance activity without introducing unnecessary strain.
8. Can endurance training improve heart rate variability (HRV) in older individuals? Improving heart rate variability (HRV) is one of the lesser-known but critical benefits of endurance training for aging adults. Higher HRV is associated with better autonomic regulation, stress resilience, and reduced cardiovascular risk. In those experiencing aging heart disease, low HRV is often a warning sign of declining heart adaptability. Engaging in regular aerobic exercise, especially with breathing control and mindful pacing, can enhance HRV over time. This makes endurance training a powerful intervention not just for physical stamina but also for neural-cardiac health.
9. What is the long-term economic impact of endurance training for those at risk for coronary artery disease? While often discussed in terms of physical health, endurance training can have substantial long-term economic benefits. By lowering the incidence and severity of age and coronary artery disease, individuals may reduce reliance on costly interventions such as hospitalizations, surgeries, and long-term medications. Preventive exercise routines also contribute to better productivity and independence, potentially delaying the need for assisted living or home care. From a public health standpoint, promoting endurance training among aging populations could ease the financial burden on healthcare systems. Thus, the investment in fitness yields both personal and societal returns.
10. How can caregivers support endurance training for loved ones with aging heart disease? Caregivers play a vital role in helping older adults integrate and maintain endurance training as part of their daily lives. Emotional encouragement, logistical support (such as arranging transportation), and participation in activities can increase adherence. Educating themselves on the basics of age and coronary artery disease also equips caregivers to identify early signs of overexertion or health changes. Involving them in exercise planning, perhaps even joining the activity, can enhance the social and emotional experience of endurance training. Their support often determines whether a person continues or abandons the effort—making them key allies in the fight against aging heart disease.
Conclusion: Embracing Endurance as a Lifelong Strategy to Protect Your Heart
As we age, the risk of developing coronary artery disease inevitably increases, but that trajectory is far from unchangeable. Understanding the relationship between age and coronary artery disease, and recognizing the role of lifestyle interventions, opens the door to preventive strategies that can truly make a difference. Endurance training emerges as one of the most promising approaches to protect against the effects of aging heart disease, offering benefits that extend beyond the cardiovascular system to enhance overall quality of life.
From improved lipid profiles and blood pressure regulation to enhanced insulin sensitivity and endothelial function, the physiological adaptations triggered by consistent aerobic exercise are profound and far-reaching. These changes, validated by a growing body of scientific literature, provide a compelling case for integrating endurance training into daily life—whether through structured workouts, active commuting, or simply walking more often.
Ultimately, the journey toward heart health in older age is not defined by radical interventions or expensive treatments but by consistent, mindful movement. By embracing endurance training as a core component of healthy aging, individuals can reclaim agency over their cardiovascular health and write a new narrative—one in which vitality, not vulnerability, defines the later stages of life. The science is clear, the strategies are accessible, and the potential for transformation is within reach for anyone willing to take the first step.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Coronary Artery Disease Prevention
Physical Activity in the Prevention and Treatment of Coronary Artery Disease
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.

