The rise of plant-based eating has brought about renewed interest in the long-term effects of dietary choices on overall health. Among the many questions posed by both health professionals and individuals considering a switch to a vegan lifestyle is this: can a vegan diet affect bone health? Specifically, concerns have emerged around the relationship between the vegan diet and osteoporosis, a condition characterized by reduced bone density and increased fracture risk. With more people adopting plant-based eating patterns for ethical, environmental, or health reasons, understanding how this lifestyle might influence skeletal integrity is both timely and essential. This article explores the scientific evidence surrounding osteoporosis in vegans, evaluates key nutrients for bone health, and offers practical strategies for maintaining strong bones on a vegan diet.
You may also like: Best Plant-Based Carbs for Energy and Health: What Science Says About Vegetarian Carbohydrates
Understanding Osteoporosis and Its Risk Factors
Osteoporosis is a chronic condition marked by the weakening of bones, which makes them fragile and more likely to break. It is often referred to as a “silent disease” because it progresses without obvious symptoms until a fracture occurs. This condition is especially prevalent among older adults, particularly postmenopausal women, but it can affect individuals of all ages. Risk factors include aging, hormonal changes, certain medications, low physical activity levels, smoking, and poor dietary intake of bone-supporting nutrients such as calcium, vitamin D, magnesium, and protein.
Bone is a living tissue that undergoes constant remodeling, with old bone being broken down and new bone being formed. Throughout childhood and early adulthood, bone formation outpaces breakdown, leading to increased bone mass. However, after peak bone mass is reached—typically around the age of 30—bone loss gradually exceeds bone formation. When bone loss becomes significant, osteoporosis can develop. Nutrition plays a pivotal role in maintaining bone density across the lifespan, and diets lacking in essential nutrients can accelerate bone loss, regardless of other risk factors.
Nutritional Considerations in a Vegan Diet
A vegan diet excludes all animal products, including meat, dairy, and eggs. While such a diet is associated with numerous health benefits—including lower risks of heart disease, type 2 diabetes, and certain cancers—it also requires careful planning to ensure adequate intake of specific nutrients. Calcium and vitamin D are the most well-known nutrients involved in bone health, and their bioavailability in plant-based diets has been a subject of much debate.
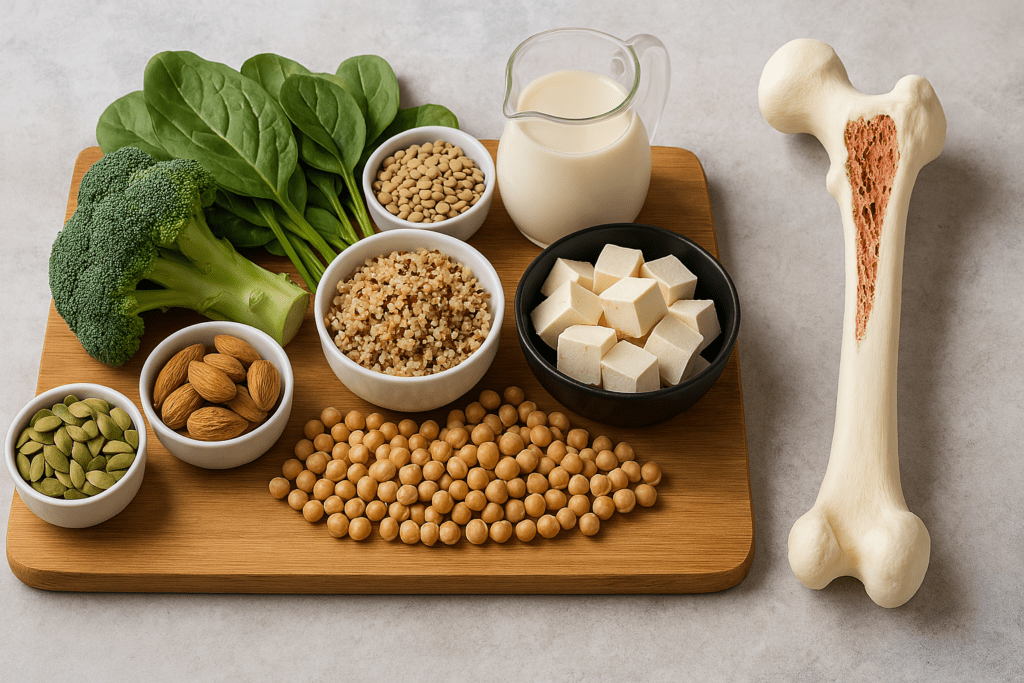
Calcium is found in plant foods like leafy green vegetables, fortified plant milks, tofu, almonds, and sesame seeds. However, the presence of compounds such as oxalates and phytates in some plant foods can inhibit calcium absorption. Vitamin D, which helps regulate calcium absorption and bone mineralization, is primarily synthesized in the skin through sunlight exposure. Few plant-based foods naturally contain vitamin D, so supplementation or the use of fortified foods may be necessary for vegans, particularly those living in regions with limited sunlight.
Magnesium and potassium, abundant in whole plant foods, support bone structure and help neutralize acid load from protein metabolism, which can otherwise leach calcium from bones. Protein, although historically linked to calcium loss, is now understood to be essential for bone matrix formation. Plant-based protein sources such as legumes, soy products, quinoa, nuts, and seeds can provide adequate protein when consumed in sufficient quantities. Thus, the vegan diet and osteoporosis connection depends greatly on how well the diet is planned and executed.
What the Research Says About Osteoporosis in Vegans
Scientific studies investigating osteoporosis in vegans have yielded mixed results. Some research suggests that vegans may have lower bone mineral density (BMD) compared to omnivores, while other studies show no significant differences when nutrient intake is adequate. A 2009 study published in Osteoporosis International found that vegetarians, particularly vegans, had lower BMD at the spine and hip than non-vegetarians, though the clinical significance of these differences was unclear. The researchers noted that when calcium and protein intake were sufficient, the gap in BMD narrowed considerably.
More recent studies have reinforced the idea that nutrient intake, rather than diet type alone, determines bone health. A 2021 study in BMC Medicine evaluated over 26,000 participants and found that vegans had a slightly higher risk of fractures, particularly in the hip, compared to meat-eaters. However, this risk was significantly reduced in vegans who consumed adequate protein and calcium. These findings suggest that the association between a vegan diet and osteoporosis is not straightforward but depends on several modifiable factors.
The use of DEXA (dual-energy X-ray absorptiometry) scans to measure bone mineral density in various populations has helped clarify these relationships. Some cross-sectional studies show that long-term vegans can maintain healthy BMD levels if they consume well-balanced diets rich in bone-supporting nutrients. Therefore, the risk of osteoporosis in vegans is not an inevitable consequence of avoiding animal products but may result from inadequate nutritional planning.
Calcium: More Than Just Dairy
One of the most common concerns about vegan osteoporosis risk is calcium deficiency. While dairy products are widely recognized for their high calcium content, several plant-based alternatives can meet calcium needs effectively. Fortified plant milks (such as almond, soy, oat, and rice milk) often contain calcium levels comparable to cow’s milk. Tofu prepared with calcium sulfate is another excellent source, along with leafy greens like kale, bok choy, and collard greens, which are lower in oxalates and offer more bioavailable calcium than spinach.
It’s important to note that calcium absorption varies based on the source and accompanying nutrients. For instance, vitamin D enhances calcium absorption, while excess sodium and caffeine can increase calcium excretion. A balanced vegan diet that includes a variety of calcium-rich foods, along with vitamin D from sunlight or supplements, can provide sufficient calcium for bone health. It’s also advisable for vegans to spread calcium intake throughout the day rather than consuming it in a single large dose, as this supports better absorption and utilization by the body.
The Role of Vitamin D in Vegan Bone Health
Vitamin D deficiency is a widespread issue that affects both vegans and non-vegans, particularly in regions with limited sunlight. However, individuals following a vegan diet may be at higher risk due to the lack of natural dietary sources of vitamin D. This fat-soluble vitamin plays a critical role in bone mineralization and helps maintain calcium balance in the bloodstream.
There are two main forms of vitamin D supplements: D2 (ergocalciferol), which is plant-derived, and D3 (cholecalciferol), which is typically sourced from lanolin in sheep’s wool but also available in vegan forms from lichen. Studies show that D3 is more effective at raising and maintaining vitamin D levels in the blood, but both forms can be useful, especially when taken consistently. For vegans, choosing a high-quality supplement or consuming fortified foods is essential, particularly during the winter months or in areas with limited sun exposure.
Testing vitamin D levels through a blood test can help determine whether supplementation is necessary. Optimal serum levels of 25-hydroxyvitamin D typically range between 30 and 50 ng/mL. Maintaining these levels may reduce the risk of bone loss and contribute to overall skeletal resilience. Therefore, understanding the role of vitamin D is crucial in the context of the vegan diet and osteoporosis prevention.
Protein Intake and Bone Matrix Integrity
Protein is a vital structural component of bone tissue, and inadequate intake can compromise bone strength over time. While some early research suggested that high protein diets could lead to calcium loss and increase fracture risk, more recent findings highlight the importance of protein in maintaining bone health. Amino acids are needed for collagen formation, which constitutes the flexible framework of bone tissue.
For vegans, meeting protein needs requires attention to both quantity and quality. Legumes, lentils, soy products, quinoa, nuts, seeds, and whole grains provide a diverse array of amino acids. While plant proteins may have lower bioavailability than animal proteins, consuming a variety of sources throughout the day can ensure adequate intake. The Recommended Dietary Allowance (RDA) for protein is 0.8 grams per kilogram of body weight, though some experts suggest higher intakes—around 1.0 to 1.2 grams per kilogram—may be beneficial for bone and muscle maintenance, especially in older adults.
Moreover, soy foods such as tofu and tempeh have been shown to contain isoflavones, plant compounds that mimic estrogen and may support bone health in postmenopausal women. Research into soy’s impact on osteoporosis in vegans has shown promising results, with some studies indicating improved BMD among those who regularly consume soy-based foods. This reinforces the idea that plant-based proteins can play a protective role when thoughtfully integrated into the diet.
Magnesium, Potassium, and Other Micronutrients
While calcium and vitamin D receive much of the attention, several other nutrients are indispensable for bone health. Magnesium is involved in bone structure and helps convert vitamin D into its active form. Leafy greens, whole grains, legumes, and nuts are rich in magnesium, and most vegans consume these foods regularly. However, some individuals may still fall short, particularly if they rely heavily on processed plant-based foods.
Potassium, found in abundance in fruits and vegetables, helps buffer acid in the body and reduces calcium loss through the urine. Diets high in fruits and vegetables are generally associated with greater bone density, suggesting that the overall pattern of plant-based eating—rich in whole, minimally processed foods—can support bone health. Zinc and vitamin K are also relevant; they contribute to collagen synthesis and bone metabolism, respectively. Nutritional yeast, seeds, and fermented plant foods are good sources of these nutrients.
Omega-3 fatty acids, particularly DHA and EPA, may also play a role in bone health by modulating inflammation and supporting bone remodeling. While these fats are typically found in fish, vegans can obtain them from algae-based supplements or through the conversion of ALA (found in flaxseeds, chia seeds, and walnuts) to EPA and DHA. Although the conversion rate is low, regular intake of ALA-rich foods and supplementation can ensure adequate levels for those concerned about vegan osteoporosis.
Lifestyle Factors That Influence Bone Health
Beyond nutrition, several lifestyle behaviors significantly influence bone health. Weight-bearing and resistance exercises stimulate bone formation and increase bone density. Activities such as walking, running, dancing, and strength training are particularly beneficial. For vegans and non-vegans alike, maintaining an active lifestyle is crucial in the prevention of osteoporosis.
Avoiding smoking and limiting alcohol intake also contribute to stronger bones. Smoking interferes with calcium absorption and reduces blood flow to bone tissue, while excessive alcohol consumption impairs the function of bone-forming cells. Sleep quality, stress management, and hormonal balance further influence skeletal health. For example, chronic stress can elevate cortisol levels, which in turn can lead to bone loss over time.
While diet is a foundational element, these lifestyle practices serve as important adjuncts in reducing the risk of osteoporosis in vegans. Incorporating these habits alongside a nutrient-rich plant-based diet creates a holistic approach to bone preservation.
Monitoring Bone Health as a Vegan
Regular monitoring of bone health can help detect early signs of bone loss and guide nutritional or lifestyle adjustments. Bone mineral density tests, such as DEXA scans, are non-invasive and can provide valuable insights into skeletal strength. While these tests are often reserved for older adults or those with specific risk factors, younger individuals following restrictive diets may also benefit from early screening.
Blood tests for vitamin D, calcium, and other relevant markers can complement imaging assessments and identify potential deficiencies. Working with a healthcare provider, particularly one familiar with plant-based nutrition, ensures that concerns related to the vegan diet and osteoporosis are addressed proactively rather than reactively. Supplementation, dietary modification, and exercise prescriptions can all be tailored based on individual needs and lab results.
An increasing number of dietitians and healthcare professionals are knowledgeable about plant-based nutrition and can help design a well-balanced vegan diet that supports bone health. Emphasizing prevention rather than waiting for complications to arise is a critical strategy in maintaining long-term skeletal health.
Frequently Asked Questions: Vegan Diet and Osteoporosis
1. Are vegans more likely to experience fractures even if they exercise regularly?
While physical activity strengthens bones and reduces fracture risk, it doesn’t entirely offset nutritional deficits. Emerging evidence suggests that exercise alone may not fully mitigate the risk of fractures associated with inadequate intake of calcium, vitamin D, and protein among vegans. The link between a vegan diet and osteoporosis becomes especially relevant when high-impact activities place greater mechanical stress on the skeletal system. Without proper nutrient support, bones may not remodel effectively in response to exercise. For individuals following a plant-based lifestyle, combining resistance training with intentional nutritional strategies is essential to reduce the likelihood of fractures.
2. How does gut health affect bone density in those on a vegan diet?
Recent studies have highlighted the gut-bone axis, a complex communication network linking gut microbiota and bone metabolism. In vegans, who often consume a high-fiber diet rich in prebiotics, gut microbial composition can shift in ways that support mineral absorption and reduce inflammation. However, the interplay between the vegan diet and osteoporosis risk may depend on how well the gut microbiome is nurtured. Fermented foods, fiber diversity, and probiotic supplementation may enhance the bioavailability of nutrients critical for bone health. Future research is expected to explore how specific strains of bacteria influence bone density in plant-based populations.
3. Can a vegan diet support bone healing after a fracture or surgery?
Recovery from fractures or orthopedic surgery demands a robust supply of nutrients involved in collagen synthesis, bone matrix formation, and inflammation control. For vegans, this presents a unique challenge that can be met with mindful dietary planning. The healing process may be slightly delayed if the individual has suboptimal levels of zinc, vitamin C, or lysine—nutrients that are essential for tissue repair. Addressing vegan osteoporosis in the context of post-injury recovery requires particular attention to nutrient-dense legumes, nuts, seeds, and fortified products. Additionally, medical professionals may recommend short-term supplementation to accelerate healing.
4. Are there regional or cultural differences in how the vegan diet and osteoporosis risk are managed?
Yes, geographical and cultural factors significantly influence how well a vegan diet supports bone health. For example, in Northern Europe and Canada, limited sunlight exposure makes vitamin D supplementation more critical for vegans. In contrast, regions with sun year-round may see lower rates of osteoporosis in vegans due to natural vitamin D synthesis. Cultural food patterns also affect access to calcium-rich plant-based foods like tofu, tempeh, or fortified plant milks. Community education on region-specific strategies for preventing vegan osteoporosis could improve health outcomes globally.
5. How do hormonal changes interact with plant-based diets in relation to osteoporosis?
Hormonal fluctuations—especially those related to menopause or thyroid disorders—can significantly influence bone health. For individuals following a vegan diet, osteoporosis risk can be compounded when estrogen levels drop, as in menopause, without compensatory dietary adjustments. Isoflavones found in soy foods may offer mild estrogen-like effects that help preserve bone density in postmenopausal women. However, this benefit is dose-dependent and varies between individuals. Consulting with a plant-based dietitian who understands hormonal dynamics can help tailor dietary interventions more effectively.
6. Are vegan athletes at greater risk for bone injuries, and how can they protect themselves?
Athletes following plant-based diets often have higher nutrient demands due to their intense training regimens. The relationship between vegan osteoporosis and athletic performance is complex, as inadequate intake of calcium, vitamin D, and total energy can increase the risk of stress fractures. Plant-based athletes can mitigate this risk by consuming energy-dense whole foods, ensuring proper recovery, and using blood markers to monitor nutrient levels. Some elite vegan athletes also use wearable bone health trackers or schedule regular DEXA scans to monitor bone density. Preventative strategies tailored to training intensity and lifestyle can offer meaningful protection.
7. Is there a psychological component to managing osteoporosis risk on a vegan diet?
Absolutely. For individuals deeply committed to ethical veganism, the idea of supplementation or consuming fortified products may conflict with their values. This internal conflict can influence decisions that impact bone health, especially if there’s resistance to adopting synthetic vitamin D3 or calcium-fortified products. The emotional and psychological dimensions of vegan osteoporosis management are often underexplored in clinical settings. Support groups, therapy, or consultations with vegan-informed healthcare professionals can help address this tension constructively. A psychologically balanced approach ensures that nutritional adequacy doesn’t feel like a compromise of core values.
8. Are there any promising innovations for preventing osteoporosis in vegans?
Yes, the field of nutritional science is rapidly evolving to meet the needs of plant-based populations. New algae-based calcium supplements and vitamin D3 derived from lichen are gaining popularity as clean-label, vegan-friendly alternatives. Food tech startups are also working on biofortified produce and functional beverages designed to support bone health in vegans. Mobile apps now integrate dietary tracking with bone health monitoring, offering predictive analytics for osteoporosis risk in vegans. These innovations make it easier to personalize prevention strategies without deviating from plant-based ethics.
9. How does long-term veganism affect bone health in older adults compared to younger individuals?
The impact of long-term veganism on bone health varies by age and life stage. While younger adults typically have higher bone remodeling capacity, older vegans may experience accelerated bone loss if nutrient intake is inadequate. The link between a vegan diet and osteoporosis becomes more pronounced with aging, particularly if physical activity levels decline and hormonal changes intensify. Regular assessments, including BMD testing and dietary reviews, become increasingly important with age. Preventing osteoporosis in vegans over 60 requires not only dietary diligence but also medical oversight and individualized supplementation.
10. What are the long-term public health implications if vegan osteoporosis risk is not addressed?
If the intersection between a vegan diet and osteoporosis risk is not addressed at the public health level, we may see a rise in fracture-related healthcare burdens in aging plant-based populations. As veganism continues to grow, especially among younger generations, education around skeletal health will become critical. National dietary guidelines may need to adapt to include bone-specific recommendations tailored to vegan populations. Healthcare systems should also consider integrating bone density screenings for long-term vegans, much like routine cholesterol checks. Proactive public health campaigns could help mitigate the long-term consequences of osteoporosis in vegans while promoting sustainable, nutrient-rich eating habits.

Conclusion: Safeguarding Bone Health on a Vegan Diet—What the Evidence Really Says
The intersection of the vegan diet and osteoporosis risk is a nuanced topic that deserves thoughtful exploration rather than blanket conclusions. While some studies suggest that vegans may be at increased risk for lower bone mineral density or fractures, the bulk of scientific evidence points to modifiable factors—particularly nutrient intake and lifestyle behaviors—as the primary determinants of bone health. Osteoporosis in vegans is not an inevitable outcome of eliminating animal products, but rather a potential risk when diets are poorly planned or lacking in essential nutrients.
By focusing on calcium, vitamin D, protein, and other supportive nutrients, along with incorporating regular weight-bearing exercise and avoiding harmful habits, vegans can maintain strong, healthy bones throughout their lives. Monitoring health markers and staying informed about the latest nutritional science empowers individuals to make proactive choices. The key is not whether a person eats animal products or not, but how intentionally and knowledgeably they construct their diet. In the broader picture, a well-planned vegan lifestyle can be entirely compatible with excellent bone health—and may even offer protective benefits when paired with whole-food, nutrient-dense choices.
As the popularity of plant-based diets continues to grow, so too does the need for accurate, evidence-based guidance on long-term health outcomes. By applying the principles of experience, expertise, authoritativeness, and trustworthiness, this article aims to provide a comprehensive, balanced, and actionable perspective on the complex relationship between vegan diets and bone health. With thoughtful planning, ongoing education, and personalized care, the path to strong bones and vibrant health is well within reach—even without animal products on the plate.
Further Reading:
The American Journal of Clinical Nutrition
6 real-life questions about vegan diets and bone health, answered
plant-based bone health, calcium sources for vegans, vegan nutrition for strong bones, bone density in plant-based diets, vitamin D alternatives for vegans, plant-based sources of protein, magnesium and bone strength, bone health over 50, soy isoflavones and bone health, vegan athletes and bone care, vegan diet nutrient deficiencies, plant-based recovery nutrition, vegan menopause support, holistic bone health strategies, vegan lifestyle and aging, nutrient absorption on a vegan diet, resistance training for bone density, vegan-friendly supplements, fermented foods and bone health, personalized vegan nutrition plans
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.

