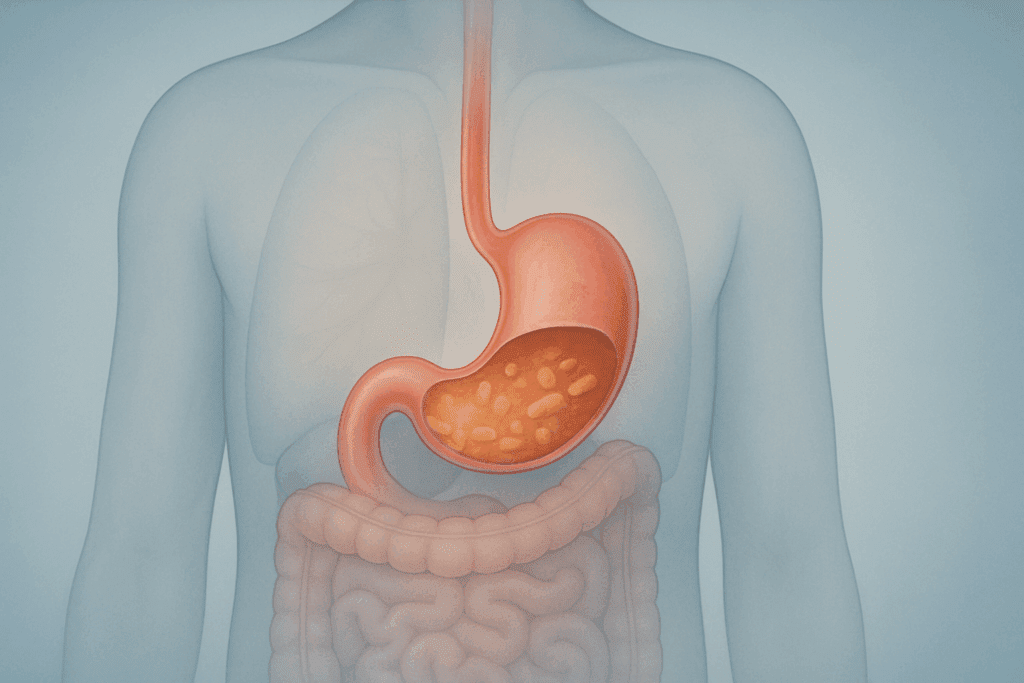
Living with gastroparesis presents unique challenges that affect not only digestive comfort but also long-term nutritional health. For many individuals, adopting a medically sound and well-balanced gastroparesis diet becomes essential for managing symptoms and improving quality of life. This condition, characterized by delayed stomach emptying without any obvious blockage, disrupts the normal movement of food through the digestive tract. Consequently, those affected often experience bloating, nausea, early satiety, and even unintentional weight loss. Developing a dietary approach that reduces discomfort while optimizing gut function is crucial to supporting overall well-being.
You may also like: The Ultimate Guide to Gut Healthy Meals: Best Meals for Gut Health and Nourishing Recipes You’ll Love
Understanding Gastroparesis and the Need for Specialized Nutrition
Gastroparesis is more than just an inconvenience; it’s a complex gastrointestinal disorder that can significantly interfere with daily life. The condition is often associated with underlying causes such as diabetes, neurological disorders, or post-surgical complications. In idiopathic cases, the root cause remains unclear. Regardless of the origin, the result is similar: the stomach’s motility is impaired, preventing food from moving efficiently into the small intestine.
This delayed gastric emptying can make it difficult to consume enough calories and essential nutrients. Therefore, implementing a gastroparesis diet tailored to the individual’s symptoms and needs is a foundational step in managing the condition. Since the digestive system’s ability to handle certain foods is compromised, dietary strategies focus on reducing meal volume, increasing meal frequency, and selecting easily digestible foods that minimize gastric burden. With the right dietary framework, many people with gastroparesis can avoid complications and maintain nutritional adequacy.
The Science Behind the Gastroparesis Diet
Unlike general dietary guidelines, a gastroparesis diet is grounded in clinical evidence and structured around physiological limitations. The stomach’s reduced ability to contract and propel food forward requires that foods be broken down into simpler, more manageable forms. Research in gastroenterology supports several modifications to reduce symptoms and enhance nutrient absorption.
Smaller, more frequent meals help bypass the stomach’s sluggish response and prevent overfilling, which can trigger nausea and discomfort. Low-fat and low-fiber foods are recommended because they are less likely to slow gastric emptying. While fiber is generally beneficial for gut health, certain types, especially insoluble fiber, can be problematic for gastroparesis patients. Instead, soluble fiber sources that do not form indigestible residue are preferred.
Liquids and pureed foods are another cornerstone of the gastroparesis diet. Since liquids empty from the stomach more quickly than solids, they provide a valuable means of delivering nutrients without exacerbating symptoms. Nutritional shakes, broths, and blended meals can help maintain calorie intake, particularly when solid foods become intolerable.
Gastroparesis Diet Modification for Long-Term Gut Support
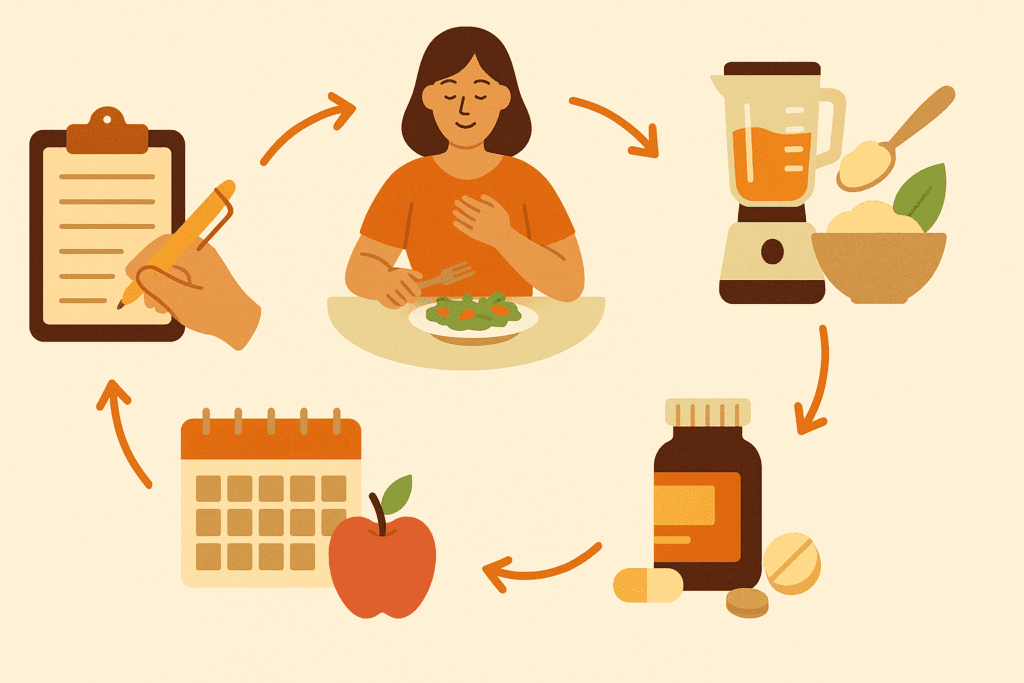
Over time, dietary strategies may need to evolve based on symptom severity, weight changes, and gastrointestinal tolerance. Gastroparesis diet modification is not a one-size-fits-all approach. Instead, it involves continuous adaptation in collaboration with healthcare providers such as gastroenterologists and registered dietitians.
Early-stage interventions often focus on eliminating foods that trigger symptoms. As individuals begin to understand their unique digestive responses, adjustments can be made to reintroduce certain foods in tolerable forms or quantities. This personalization is essential for maintaining dietary variety and preventing nutritional deficiencies.
Cooking methods also play a crucial role in diet modification. Steaming, boiling, and blending can significantly reduce the fiber and fat content of foods while preserving nutrients. By softening textures and altering compositions, these techniques make it easier for the stomach to process meals. Equally important is the inclusion of high-nutrient-density foods in forms that are easy to digest. Smoothies made with nut butters, avocado, and fortified milk alternatives are excellent examples of modified meals that support both gut health and energy needs.

Proven Food Strategies in a Gastroparesis Diet for Gut Health
Navigating the dietary landscape of gastroparesis can be overwhelming, but proven strategies offer a guiding light for those seeking balance and relief. Central to these strategies is the careful selection of foods that are gentle on the stomach while offering robust nutritional profiles.
Lean proteins such as poultry, fish, and eggs are typically well-tolerated and can be incorporated into meals with soft textures or blended into soups. Carbohydrates should come from refined grains and peeled, cooked fruits and vegetables. While this may seem counterintuitive to general gut health recommendations, these foods reduce digestive workload and are more suitable for gastroparesis management.
Hydration is another critical component. Adequate fluid intake supports digestion, prevents constipation, and helps move food through the gastrointestinal system more effectively. However, carbonated beverages and high-sugar drinks should be avoided, as they may worsen bloating and nausea.
For individuals experiencing severe symptoms, incorporating oral nutrition supplements can help bridge nutritional gaps. These supplements are designed to be calorie- and nutrient-dense while being easy to consume and digest. As tolerance improves, these can be slowly phased out in favor of whole-food alternatives.

Creating a Diet Plan for Gastroparesis to Gain Weight Safely
Weight loss is a common challenge for individuals with gastroparesis, often due to poor appetite, nausea, and the inability to tolerate large meals. Developing a diet plan for gastroparesis to gain weight requires a delicate balance between calorie density and gastrointestinal tolerance.
Frequent, small meals enriched with calorie-dense ingredients are essential. Adding healthy fats in easily digestible forms—such as oils, smooth nut butters, and pureed avocados—can significantly increase caloric intake without increasing meal volume. Protein powders, meal replacement drinks, and full-fat dairy or non-dairy alternatives can also provide needed calories in liquid forms.
In addition, timing plays a strategic role. Some individuals find that consuming their most substantial meals earlier in the day, when symptoms are typically milder, allows for better intake. Incorporating gentle movement after meals can aid digestion and reduce postprandial discomfort.
Tracking food intake and weight can help identify patterns and fine-tune dietary strategies. Consultation with a registered dietitian specializing in gastrointestinal conditions ensures that weight gain efforts do not come at the expense of symptom control or nutritional quality.
Gastroparesis Foods to Avoid: What to Eliminate for Comfort and Gut Stability
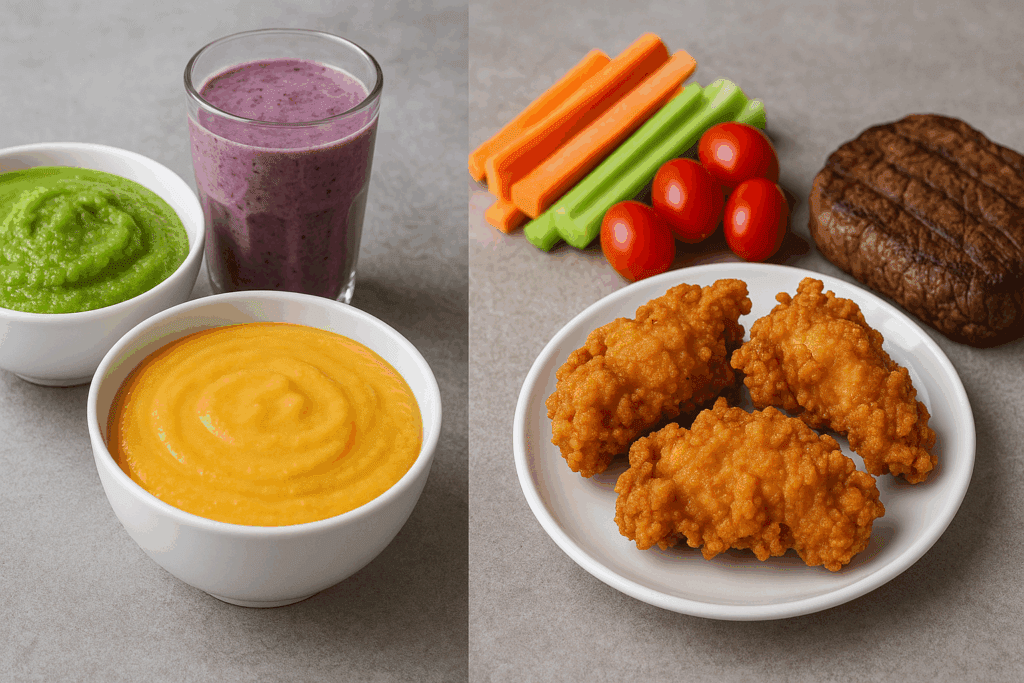
Understanding which gastroparesis foods to avoid is essential to minimizing flare-ups and enhancing daily comfort. While individual tolerances may vary, certain food categories are consistently associated with symptom exacerbation and should be limited or eliminated from the diet.
High-fat foods, particularly those from fried and greasy sources, tend to delay stomach emptying and should be avoided. These include fast food, heavy cream sauces, and processed meats. Similarly, high-fiber foods such as raw vegetables, legumes, and whole grains can pose challenges due to their dense and fibrous nature.
Tough meats, nuts, seeds, and foods with skins or peels are also problematic. Their coarse textures can irritate the stomach lining and slow down gastric processing. In some cases, even seemingly healthy foods such as broccoli, cabbage, and corn can provoke discomfort due to their insoluble fiber content.
Avoiding carbonated beverages is equally important. These drinks introduce excess air into the stomach, increasing bloating and pressure. Caffeinated and alcoholic beverages should be limited as well, as they can irritate the stomach lining and interfere with motility.
List of Foods You Can Eat with Gastroparesis for Gut Support
While restrictions are necessary, there’s still a variety of foods you can eat with gastroparesis that support gut health and provide essential nutrients. The key is focusing on texture, fat content, and digestibility.
Cooked, peeled, and pureed vegetables such as carrots, zucchini, and squash are gentle on the stomach and provide important vitamins and minerals. Fruits like bananas, applesauce, and canned peaches (packed in juice, not syrup) are generally well-tolerated. White rice, pasta, and white bread are easier to digest than whole grain alternatives and can form the carbohydrate base of many meals.
Protein sources that are soft and lean, such as poached chicken, scrambled eggs, and baked white fish, offer essential amino acids without overburdening the stomach. Dairy or dairy substitutes that are low in fat and lactose can contribute calcium and vitamin D without causing bloating.
Broths, smoothies, and pureed soups are versatile and can be tailored to include a range of nutrients. These liquids provide hydration while making it easier to consume calories in a tolerable format. Flavored with herbs rather than spices, these meals can be both satisfying and symptom-friendly.
How to Personalize a Gastroparesis Diet Without Sacrificing Nutrition
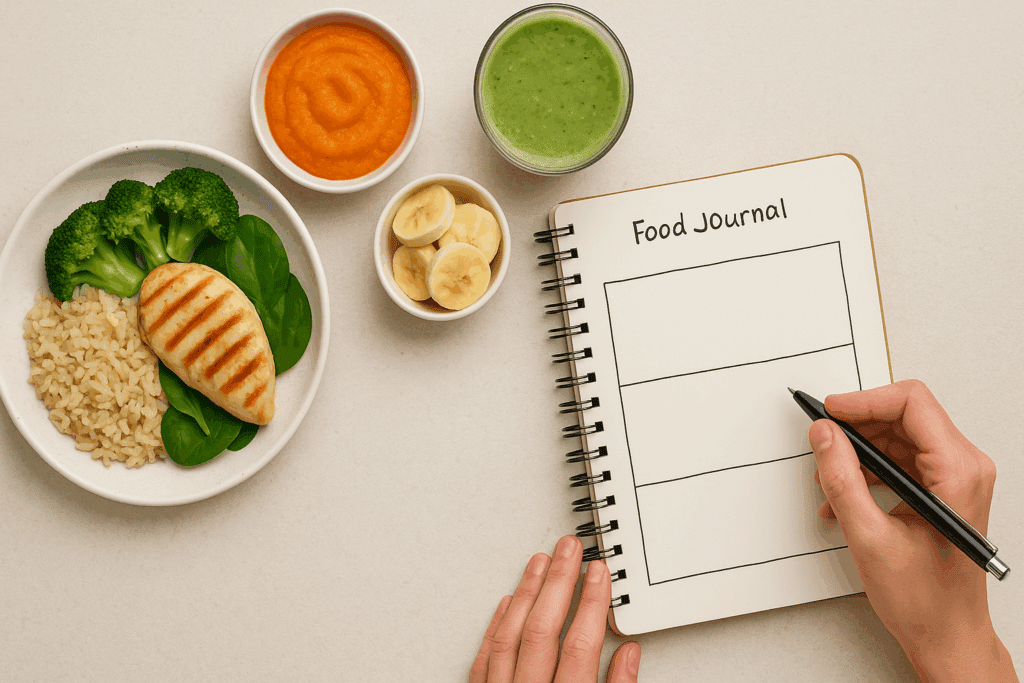
Personalizing a gastroparesis diet requires careful observation, dietary tracking, and an understanding of how different foods interact with the body. While foundational guidelines exist, no two individuals with gastroparesis will have identical dietary needs or responses.
Maintaining a food journal that records meals, symptoms, and energy levels is a practical starting point. This practice allows for pattern recognition and helps identify foods that are either helpful or harmful. Over time, patients and healthcare professionals can use this information to craft a more sustainable and enjoyable diet.
It’s also important to adapt the diet as symptoms change. During periods of symptom relief, a broader range of foods may be tolerable, allowing for improved nutritional variety. During flare-ups, a return to a more restrictive, liquid-based diet may be necessary.
Nutritional supplementation should be personalized as well. For individuals with specific deficiencies, targeted supplementation of nutrients such as iron, vitamin B12, and magnesium can be recommended by a healthcare provider. This ensures nutritional adequacy even when food choices are limited.
The Role of Holistic Supplements in a Gastroparesis Diet
Incorporating holistic supplements into a gastroparesis diet can provide additional support, particularly when nutrient absorption is impaired or dietary intake is insufficient. However, any supplementation should be evidence-based and carefully monitored.
Digestive enzymes may assist in breaking down food more effectively, reducing the burden on the stomach. Similarly, ginger supplements have been shown to promote gastric motility and may alleviate nausea when used appropriately. Probiotics, while not a cure, may support gut microbiota and overall digestive health.
Vitamins and minerals in chewable, liquid, or powdered forms are often better tolerated than tablets or capsules. A registered dietitian or physician can help determine appropriate formulations and dosages. It is essential to ensure that supplements do not interact negatively with medications or exacerbate symptoms.
While holistic supplements can play a supportive role, they are not substitutes for dietary therapy. Their greatest benefit lies in enhancing the foundation of a well-constructed gastroparesis diet, not replacing it.
Foods to Eat with Gastroparesis for Energy, Healing, and Digestive Ease
Prioritizing foods to eat with gastroparesis involves selecting options that are nutrient-rich, easy to digest, and energy-boosting. These foods support not only symptom relief but also long-term healing and resilience.
Mashed sweet potatoes, oatmeal (made with extra liquid), and well-cooked cereals can provide complex carbohydrates for sustained energy. Eggs, tofu, and soft cheeses contribute protein while being gentle on the digestive system. Blended fruits such as papaya and mango offer vitamins and antioxidants with minimal fiber.
Including fermented foods like yogurt (if tolerated) can promote microbial diversity in the gut, although this should be done gradually. Incorporating bone broth and collagen-rich foods may support gut lining integrity and overall digestive comfort.
When creating meals, combining food groups—such as protein and carbohydrates with a bit of healthy fat—can help balance blood sugar levels and provide lasting satiety. Presentation also matters; appealing textures, temperatures, and flavors can make meals more enjoyable and encourage better intake.
Frequently Asked Questions About the Gastroparesis Diet: Practical Insights and Advanced Strategies
What are some overlooked challenges when starting a gastroparesis diet?
Many patients initially focus on what foods are safe or unsafe, but they often underestimate the emotional toll and social isolation that can accompany these dietary restrictions. For example, eating out with friends or attending family gatherings can become stressful, especially when unfamiliar food is involved. Navigating these situations with grace requires planning and communication. It’s also easy to overlook the mental energy needed to prepare multiple small meals each day, which can be taxing without adequate support. Creating a structured routine and finding community support can ease this transition and help individuals sustain their gastroparesis diet over time.
How can I optimize a gastroparesis diet modification plan for both nutrition and convenience?
Efficiency is key when dealing with fatigue and fluctuating energy levels. Batch cooking and freezing tolerated meals can be a lifesaver for individuals undergoing gastroparesis diet modification. Consider preparing blended soups or puréed vegetable sauces in advance and storing them in portion-sized containers. Also, investing in a high-quality blender can make it easier to create texture-modified meals that retain their nutritional value. To simplify grocery shopping, maintain a core list of foods you can eat with gastroparesis and build meal plans around them each week.
Can a gastroparesis diet support athletic activity or exercise goals?
Yes, but it requires careful planning. For active individuals, balancing caloric needs with symptom management can be tricky. Pre-exercise snacks should be low in fat and fiber but rich in easily digestible carbohydrates, such as a ripe banana or a small portion of applesauce. Post-exercise recovery drinks can be customized with protein powders and tolerated liquid bases to aid muscle repair. If structured thoughtfully, a gastroparesis diet can complement moderate exercise without causing gastric distress.
Is there a difference between short-term symptom management and long-term gastroparesis diet planning?
Absolutely. Short-term symptom management often involves reverting to a liquid or soft diet during flare-ups, while long-term planning focuses on gradual reintroduction of tolerated foods and maintaining nutritional diversity. Over time, a gastroparesis diet must evolve based on tolerance levels, lifestyle changes, and overall health status. Long-term strategies also consider micronutrient intake and supplementation, as chronic dietary limitations can lead to deficiencies. A dietitian can help guide this evolution to maintain both digestive health and whole-body wellness.
How can I creatively diversify a list of foods you can eat with gastroparesis without triggering symptoms?
It’s important not to fall into the trap of eating the same few safe foods every day. Flavor and variety can be achieved by rotating seasonings that don’t irritate the stomach, such as ginger, cinnamon, and turmeric. Experimenting with different cooking methods, like baking, steaming, or slow-cooking, can also enhance taste and texture. Infusing meals with natural broths or low-fat sauces can keep them appealing while still aligning with a gastroparesis diet. Even small variations, such as swapping sweet potatoes for white potatoes or trying new fruit purées, can reinvigorate your menu without overwhelming your digestion.
What are common misconceptions about a diet plan for gastroparesis to gain weight?
A frequent misconception is that increasing portion sizes is the best approach for weight gain. In reality, patients with gastroparesis must prioritize calorie density over volume to avoid symptoms like bloating or nausea. Nutrient-packed smoothies, fortified cereals, and small bites throughout the day are more effective than large meals. Another misunderstanding is that weight gain equates to abandoning dietary restrictions. A successful diet plan for gastroparesis to gain weight must still align with tolerated food lists and incorporate high-calorie options in a safe and structured way.
How do I avoid nutritional gaps while following gastroparesis diet modification?
Supplementation is often necessary due to the restrictive nature of the diet. Many people with gastroparesis are deficient in key vitamins such as B12, D, and A, as well as minerals like magnesium and potassium. Working with a healthcare provider to regularly monitor these levels is essential. Fortified plant-based milks, pureed legumes in soups, or low-fiber green powders can help mitigate deficiencies. Strategic use of supplements and fortified foods ensures that gastroparesis diet modification doesn’t compromise essential nutrient intake.
What are the psychological impacts of long-term gastroparesis dietary restrictions?
Chronic dietary restriction can lead to feelings of anxiety, isolation, and even disordered eating behaviors. Individuals may develop food aversions due to fear of symptom flare-ups or may feel emotionally disconnected from food as a source of enjoyment. Mindful eating practices, counseling, and support groups can help rebuild a positive relationship with food. It’s also important to celebrate small dietary victories and to shift focus toward what is possible within the gastroparesis diet framework. Psychological resilience is just as important as physical nourishment when managing chronic digestive disorders.
Which foods to eat with gastroparesis offer both nutrition and comfort?
Comfort and nutrition can coexist, even in a restricted diet. Warm, blended soups made from peeled vegetables and lean protein offer satiety and digestibility. Smoothies with lactose-free milk, bananas, and nut butters can be comforting and calorie-rich. Cooked cereals such as cream of rice or oatmeal (if tolerated) provide a warming, grounding meal base. Incorporating flavors or spices associated with positive memories can also enhance comfort. Ultimately, foods to eat with gastroparesis should satisfy both emotional and physiological needs.
Are there any emerging research findings or innovations related to the gastroparesis diet?
Yes, recent research is exploring how personalized nutrition and microbiome profiling might help tailor gastroparesis diet recommendations more precisely. For example, emerging studies suggest that certain probiotic strains may aid in gastric motility, though evidence is still in early stages. Newer medical foods designed for easy digestion are also being tested for efficacy in patients with delayed gastric emptying. Mobile apps for symptom tracking and diet logging are helping patients identify correlations between food intake and symptom severity. These innovations are shaping a more personalized and data-driven future for those following a gastroparesis diet.
Conclusion: Nourishing the Body Naturally Through a Thoughtful Gastroparesis Diet
Living with gastroparesis requires diligence, adaptability, and a compassionate approach to nutrition. By implementing a structured yet flexible gastroparesis diet, individuals can reclaim a sense of control over their health and well-being. Through thoughtful modifications and strategic food choices, it is entirely possible to reduce symptoms, maintain nutritional balance, and even regain lost weight without compromising gut health.
Understanding which gastroparesis foods to avoid and embracing the list of foods you can eat with gastroparesis empowers individuals to eat confidently and comfortably. For those seeking to restore lost weight or enhance energy, a diet plan for gastroparesis to gain weight should emphasize nutrient density and digestibility. Holistic supplements, when integrated appropriately, can provide valuable support in bridging nutritional gaps and reinforcing digestive strength.
Ultimately, the journey toward digestive health is not about rigid restrictions but about informed nourishment. With proper guidance, patience, and commitment, a gastroparesis diet becomes more than a medical necessity—it transforms into a sustainable lifestyle that nurtures both the body and the spirit.
Further Reading:
Is There a Gastroparesis Diet?
How To Follow a Gastroparesis Diet: What To Eat and What To Avoid

