Bradycardia, defined as a resting heart rate below 60 beats per minute, can be either a normal variant in well-trained athletes or a concerning condition tied to the heart’s electrical system. For those navigating life with this slower-than-average heartbeat, questions about physical exertion and dietary choices often surface. Is exercise safe? Which routines are beneficial versus risky? And how can nutrition support or hinder heart rhythm stability?
This comprehensive guide explores how individuals with bradycardia can engage in safe and effective exercise routines to enhance endurance and cardiovascular function. It also outlines which dietary choices may worsen symptoms, emphasizing the most important bradycardia foods to avoid and highlighting the best exercise for bradycardia for optimal heart performance and overall wellness.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice
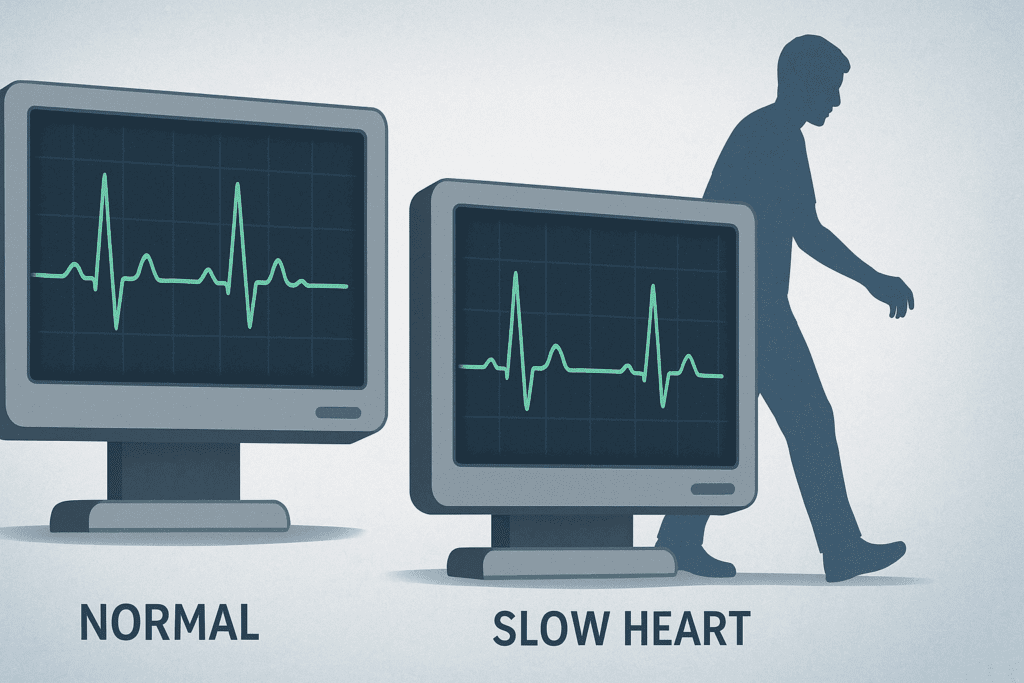
Understanding Bradycardia and Its Effects on Physical Activity
Bradycardia often sparks concern because a slow heart rate may imply the heart isn’t pumping enough blood to meet the body’s needs—especially during physical exertion. This can lead to symptoms like lightheadedness, fatigue, and even fainting. However, not all forms of bradycardia are inherently dangerous. In athletes, a low heart rate can reflect efficiency. In contrast, in the general population or those with underlying heart disease, bradycardia can indicate a conduction problem such as sick sinus syndrome or AV block.
Physical activity increases oxygen demand, so a heart that beats too slowly may struggle to keep up. For individuals with symptomatic bradycardia, this presents a challenge. Nonetheless, being sedentary carries its own risks. That’s why it’s crucial to differentiate between safe forms of bradycardia and those that require medical management. A full cardiac evaluation, including stress testing or Holter monitoring, is essential before beginning a structured fitness plan. Once cleared, patients can safely participate in exercise—when it is tailored to their capabilities and monitored appropriately.

Why Physical Activity Supports a Healthy Heart, Even in Bradycardia
Exercise remains a cornerstone of cardiovascular health. For those with bradycardia, physical activity helps increase stroke volume—the amount of blood pumped per beat—enhancing circulation even at slower pulse rates. Over time, regular exercise also supports the development of new blood vessels (collateral circulation), which can improve oxygen delivery to vital tissues.
Beyond the cardiovascular benefits, regular movement contributes to metabolic efficiency, glucose regulation, and improved mood. Many individuals with bradycardia are hesitant to engage in workouts due to fear of overexertion, but with the right plan, they can harness the mood-lifting and stamina-building effects of exercise. These psychological benefits can reduce stress and anxiety, which, in turn, support autonomic balance and promote healthier heart rhythms.
In many cases, physicians actually recommend structured movement for patients with bradycardia, especially when the condition is mild or associated with age or medication. The key is customizing the type, duration, and intensity of each session and integrating close monitoring practices.

Finding the Best Exercise for Bradycardia: What Works and Why
Determining the best exercise for bradycardia involves selecting routines that support cardiovascular fitness without triggering symptoms. The most effective forms of physical activity for individuals with bradycardia include low- to moderate-intensity aerobic exercises like walking, swimming, elliptical training, or cycling. These activities can be sustained for longer periods and allow for gradual cardiovascular adaptation.
Gentle interval training may also be appropriate when structured correctly. This doesn’t mean high-intensity interval training (HIIT), but rather alternating between light and moderate intensity to keep the heart engaged without overwhelming it. Activities like yoga and tai chi are ideal complements, as they emphasize breathing, mindfulness, and gradual transitions in physical exertion—all elements that support heart rate variability and nervous system regulation.
Strength training also has its place, especially for preserving muscle mass and promoting metabolic health. However, breath control is vital—holding the breath during a lift (the Valsalva maneuver) can dangerously lower heart rate and blood pressure in those with bradycardia. Lifting lighter weights with higher repetitions helps mitigate that risk.
Consistency and heart rate monitoring are crucial. Individuals should be able to speak comfortably during most of their workouts. Investing in a heart rate monitor can help detect when the heart rate dips too low, providing real-time cues to rest or modify intensity.
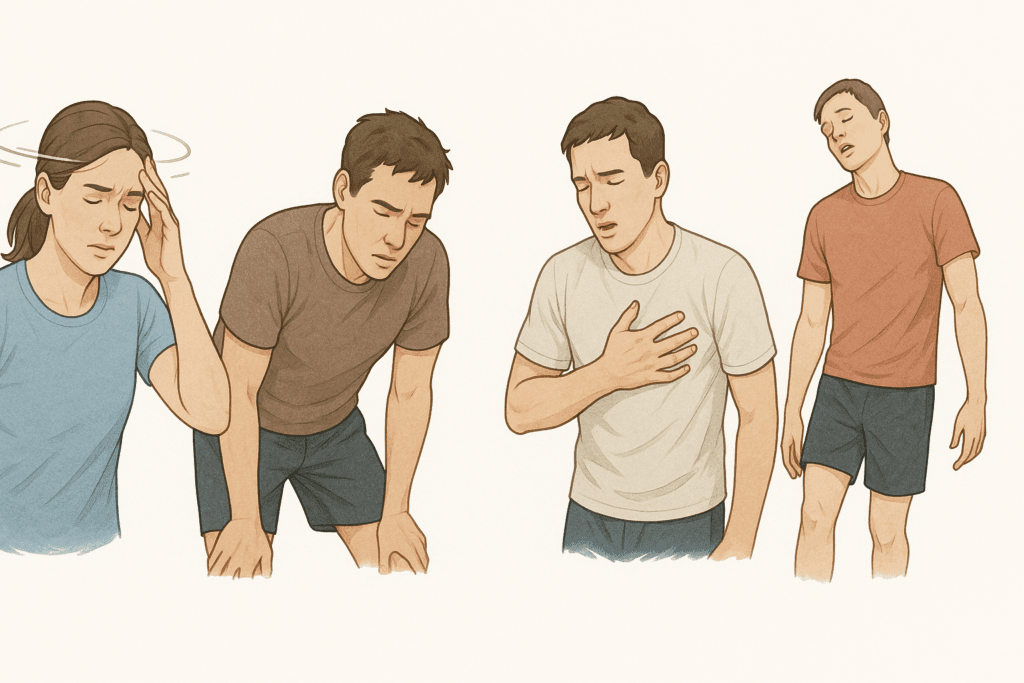
Identifying Symptoms and Avoiding Overexertion
Exercise should never leave you dizzy, breathless, or disoriented. Individuals with bradycardia need to pay close attention to early warning signs of overexertion. Symptoms like chest tightness, faintness, extreme fatigue, or palpitations suggest that the heart may be struggling to keep up with the body’s demand for oxygen. When any of these occur, activity should stop immediately, and medical advice should be sought before resuming.
Warm-ups and cool-downs are essential components of a bradycardia-friendly workout. Abrupt starts and stops can confuse the cardiovascular system, especially in the presence of an underlying rhythm disturbance. Stretching, slow walking, and breathing exercises prepare the heart and body for transitions.
Environmental conditions also matter. Heat, humidity, and dehydration can amplify bradycardia symptoms, so hydration should be a top priority. Monitoring fluid intake before, during, and after exercise reduces the risk of low blood pressure and heart rate instability during workouts.
Working closely with a healthcare provider helps fine-tune your routine, especially if medications or implanted devices like pacemakers are part of your treatment plan. Individualized advice ensures you’re not just safe, but progressing in ways that enhance your quality of life.

Bradycardia Foods to Avoid: Nutritional Triggers of Rhythm Imbalance
Nutrition plays a powerful role in heart rhythm stability. For individuals managing bradycardia, avoiding certain foods can reduce symptom frequency and severity. One of the most important categories is high-sodium foods. Excess sodium can raise blood pressure and cause fluid retention, placing added stress on a heart that already beats slowly. Processed and packaged foods—such as frozen dinners, canned soups, cured meats, and chips—are common culprits.
Another group of bradycardia foods to avoid includes those high in saturated and trans fats. These fats contribute to arterial plaque buildup, reduce blood flow, and impair oxygen delivery. Fried foods, butter-heavy dishes, and commercially baked goods should be minimized or replaced with healthier fat sources like nuts, seeds, and olive oil.
Stimulants like caffeine are a gray area. While they may temporarily increase heart rate, the effect is inconsistent and potentially risky in those with bradycardia. Some people may tolerate a morning cup of coffee without issue, while others experience palpitations or irregular heartbeats. Alcohol, similarly, can depress the nervous system and exacerbate low heart rates. Moderation is essential, and elimination may be necessary for those with heightened sensitivity.
Potassium-rich foods can also become problematic for bradycardic patients, particularly if kidney function is impaired or if medications influence potassium levels. Overconsumption of bananas, potatoes, or supplements without medical supervision may lead to dangerous imbalances.

Designing a Heart-Supportive Meal Plan for Bradycardia
An optimal diet for bradycardia management emphasizes whole, unprocessed foods rich in nutrients that support cardiac function. Fresh fruits, vegetables, whole grains, lean proteins, and plant-based fats form the backbone of a heart-healthy meal plan. These foods not only avoid triggering symptoms but actively nourish the heart muscle and support stable electrical activity.
Magnesium and calcium play important roles in nerve transmission and muscle contraction, including the heart. Foods like leafy greens, yogurt, almonds, and beans provide these minerals in balanced quantities. Meanwhile, omega-3 fatty acids from fatty fish like salmon or flaxseeds are known to reduce inflammation and support heart rhythm.
Meal size and timing are also key considerations. Large meals can increase vagal tone—the influence of the vagus nerve on the heart—which may slow heart rate further. Instead, smaller meals eaten throughout the day can help maintain stable blood sugar and minimize sudden shifts in heart rhythm.
Hydration is another cornerstone. Even mild dehydration reduces blood volume, which can impair circulation and exacerbate symptoms. Drinking water regularly throughout the day—not just during workouts—ensures the cardiovascular system is well supported.

Medication, Pacemakers, and Monitoring During Exercise
Many individuals with bradycardia are prescribed medications that can influence heart rate. Beta blockers, calcium channel blockers, and other drugs may intentionally slow the heart. While beneficial for blood pressure or arrhythmia control, these medications can compound bradycardia symptoms, especially during exercise. Regular follow-up with a cardiologist ensures that prescriptions are optimized based on how your body responds to physical exertion.
For patients with implanted pacemakers, exercise is not only safe but encouraged. Pacemakers regulate rhythm and can be programmed to respond to physical activity. However, their settings should be reviewed periodically to match your fitness goals and ensure compatibility with your exercise regimen.
Fitness trackers and heart rate monitors can serve as real-time feedback tools. These devices help users recognize when their heart rate is in a safe zone and when it’s time to rest. While not substitutes for clinical evaluation, they add a valuable layer of awareness and motivation.
A symptom journal—tracking perceived exertion, meals, medications, and heart rate patterns—can offer rich insights for both patients and physicians. Over time, this data supports more personalized care and helps create an evolving fitness and wellness plan tailored to your heart.
Frequently Asked Questions: Exercise and Nutrition for Bradycardia
1. Can people with bradycardia safely engage in competitive sports or endurance events?
Yes, but this requires careful evaluation. While some endurance athletes naturally have bradycardia due to high cardiovascular efficiency, not all individuals with bradycardia are suited for competitive sports without medical oversight. For someone with symptomatic or pathological bradycardia, participating in endurance events can pose risks, especially if the heart is unable to increase its rate in response to increased demand. The best exercise for bradycardia in such cases often involves low-impact endurance training with close monitoring. Before training for marathons or triathlons, athletes with bradycardia should undergo exercise stress testing to ensure safe cardiac response and rule out underlying conduction issues.
2. How does emotional stress impact heart rate in people with bradycardia?
Emotional stress can have paradoxical effects on heart rate. In some individuals, stress triggers a fight-or-flight response, increasing sympathetic nervous system activity and potentially counteracting bradycardia. However, others may experience heightened parasympathetic tone, which can actually slow the heart rate further. This can make managing stress essential for maintaining stability in those prone to bradycardia. Activities like deep breathing, mindfulness, or yoga not only serve as the best exercise for bradycardia due to their calming effect but also help regulate the autonomic nervous system. Stress management should be viewed as both a psychological and cardiovascular strategy.
3. Are wearable heart monitors reliable for people with bradycardia during exercise?
Most consumer-grade heart monitors are generally accurate for tracking heart rate in people with bradycardia, but they do have limitations. Wrist-based monitors can sometimes miss very low or irregular heart rhythms, especially during slow or static exercises. Chest strap monitors tend to provide more reliable data and are recommended for those needing consistent monitoring during workouts. Accurate readings help determine whether the current routine qualifies as the best exercise for bradycardia, based on real-time data. When choosing a device, users should look for features that support ECG-quality readings and allow data export for healthcare review.
4. Can intermittent fasting affect heart rate stability in bradycardia?
Intermittent fasting may influence electrolyte levels and hydration status, which in turn can affect heart rate stability in individuals with bradycardia. During fasting periods, reductions in glucose and fluid intake may trigger a stronger parasympathetic response, potentially worsening slow heart rhythms. While some may tolerate fasting well, others may feel fatigued, dizzy, or lightheaded—symptoms that signal inadequate cardiac output. For those experimenting with dietary routines, it’s important to be aware of bradycardia foods to avoid, especially those that deplete potassium or magnesium during fast-breaking meals. Always consult a physician before integrating fasting into a bradycardia management plan.
5. What are some overlooked bradycardia foods to avoid that people may not realize are harmful?
While common culprits like processed meats and salty snacks are well-known, many people overlook seemingly healthy items like sports drinks, plant-based meat substitutes, and frozen vegetable mixes with added sodium. These items often contain preservatives, artificial flavor enhancers, or hidden electrolytes that can disrupt the heart’s electrical balance. For individuals managing bradycardia, even “low-sodium” labeled foods should be read carefully. Another overlooked category includes energy bars and protein powders, which may contain stimulants or added caffeine. Understanding which bradycardia foods to avoid means reading ingredient lists and recognizing that not all “health foods” are heart-friendly.
6. Does climate or altitude affect how people with bradycardia should exercise?
Absolutely. High altitudes decrease oxygen availability, which can place additional stress on the cardiovascular system. For individuals with bradycardia, this means the heart may need to compensate by increasing stroke volume, a task it may not always manage efficiently. Similarly, hot and humid climates can cause vasodilation and dehydration, compounding bradycardia symptoms. In such cases, the best exercise for bradycardia involves low-exertion indoor routines like stationary cycling, gentle resistance training, or climate-controlled yoga. Adjusting intensity and hydration strategies in response to environmental changes is essential for safety and performance.
7. Are there any supplements that help regulate heart rate in bradycardia?
Some supplements may support autonomic balance and heart rhythm, but they should never replace medical treatment. Magnesium, for example, plays a vital role in cardiac conduction and may help in cases of mild bradycardia linked to deficiency. Coenzyme Q10 and L-carnitine are other nutrients studied for their cardiovascular benefits, particularly in mitochondrial energy production. However, caution must be exercised with herbal stimulants like ginseng or guarana, which may interact negatively with medications or worsen symptoms. Anyone considering supplements should also evaluate bradycardia foods to avoid, since combining supplements with inappropriate foods could lead to unintended imbalances.
8. How can someone with bradycardia build endurance without stressing the heart?
Endurance training with bradycardia requires a gradual and consistent approach. Start with short, low-intensity sessions and prioritize activities that engage large muscle groups in rhythmic motion. Swimming and elliptical training are often considered the best exercise for bradycardia in this regard, as they allow for continuous movement without sharp spikes in demand. Over time, increasing duration and mild resistance helps condition the cardiovascular system. Incorporating breathing techniques and pacing strategies also ensures that heart rate changes remain within a safe and effective range.
9. How do medications for unrelated conditions affect exercise with bradycardia?
Medications prescribed for unrelated conditions can unexpectedly influence heart rate. Antidepressants, for example, particularly SSRIs or tricyclics, may slow the heart or blunt cardiovascular response to exertion. Similarly, certain allergy medications or sedatives can increase vagal tone, intensifying bradycardia. For this reason, when evaluating the best exercise for bradycardia, it is essential to consider the full medication profile. Patients should regularly review their prescriptions with a healthcare provider, especially when making changes to their fitness routine or dietary patterns, including those involving bradycardia foods to avoid.
10. What role does sleep quality play in bradycardia and fitness progress?
Sleep is a crucial but often overlooked factor in managing bradycardia. During deep sleep, heart rate naturally slows, and this nighttime bradycardia can be more pronounced in individuals with existing rhythm issues. Poor sleep can impair recovery, increase inflammation, and disrupt autonomic balance—making it harder for the body to adapt to exercise. Moreover, insufficient sleep may increase reliance on stimulants like caffeine, which rank among the bradycardia foods to avoid for sensitive individuals. Prioritizing sleep hygiene, including consistent bedtime routines, screen-free wind-down time, and comfortable environments, supports both heart rhythm regulation and the benefits of the best exercise for bradycardia.
Conclusion: Stronger Hearts Start with Smarter Choices for Bradycardia
Living with bradycardia does not mean avoiding physical activity or resigning yourself to limitations. In fact, a thoughtful combination of movement, monitoring, and nutrition can empower individuals with this condition to thrive. The best exercise for bradycardia isn’t about pushing limits—it’s about consistency, moderation, and activities that elevate endurance while keeping your heart rhythm safe.
Equally important is attention to diet. Identifying bradycardia foods to avoid, like sodium-rich processed meals, unhealthy fats, and potential stimulants, plays a vital role in rhythm regulation. A heart-smart diet filled with minerals, hydration, and balanced meals complements your exercise routine and creates a foundation for long-term heart health.
With the support of medical guidance, smart monitoring tools, and a personalized wellness strategy, it’s entirely possible to enhance endurance and boost performance—even with a slower heartbeat. The journey to a stronger, healthier heart begins with understanding your unique needs and making choices rooted in science, mindfulness, and confidence.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Is it safe to exercise with bradycardia?

