For many people living with diabetes, one of the most frustrating and confusing symptoms isn’t high blood sugar itself—it’s the constant and overpowering hunger that seems to come out of nowhere. You might eat a full meal, only to find yourself starving again within the hour. Or perhaps you wake up in the middle of the night with an urgent need to eat, even though you had dinner not long ago. If you’ve ever wondered, “Why does diabetes make you so hungry?” or asked yourself how to stop diabetes hunger, you’re not alone.
This experience, often referred to as diabetes hunger, is more than just a nuisance. It reflects deeper biological mechanisms related to blood sugar control, insulin resistance, hormonal signaling, and even sleep and stress. People who find themselves super hungry all the time as a diabetic may feel like they’re stuck in a loop of eating, crashing, and craving all over again. Understanding what’s driving this intense hunger—and how to manage it naturally—can be empowering and life-changing.
This article dives deep into why diabetes triggers such persistent hunger, what it means when you’re waking up hungry in the middle of the night with diabetes, and how to regain control through science-backed, natural strategies that support better metabolic health.
You may also like: Why Am I Craving Sweets All of a Sudden? Expert-Backed Reasons and How to Stop Sugar Cravings Naturally

The Science Behind Diabetes Hunger: Why It Happens
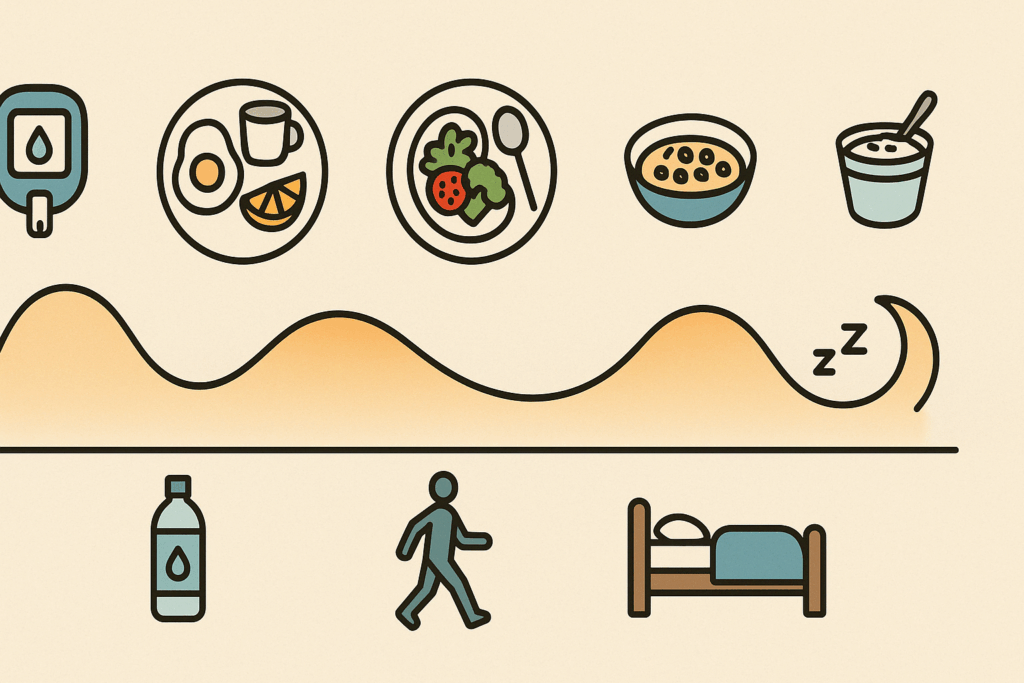
The root of diabetes hunger lies in how the body regulates and responds to blood sugar. Glucose is our primary source of energy, and insulin—the hormone produced by the pancreas—is essential for transporting glucose into cells. In people without diabetes, insulin works effectively to keep blood sugar balanced and hunger at bay. But in diabetes, either insulin is missing (as in type 1 diabetes) or the body becomes resistant to its effects (as in type 2 diabetes). This means that even when glucose is circulating in the blood, cells can’t absorb it properly and remain “starved.”
This creates a paradox: despite high levels of sugar in the bloodstream, the body signals hunger because it isn’t getting the fuel it needs at the cellular level. This internal imbalance results in diabetes hunger—a form of excessive appetite also known as polyphagia. It’s why people living with diabetes might feel super hungry all the time, even when they’re eating regularly.
Insulin resistance also plays a role in disrupting the communication between hormones that regulate hunger and satiety, such as leptin and ghrelin. This hormonal dysregulation further confuses the brain’s hunger signals, intensifying cravings and making it harder to feel full after meals. This cycle becomes especially challenging when blood sugar levels remain unbalanced.

Why You Still Feel Hungry Even After Eating
A common concern among those with diabetes is feeling hungry immediately after eating a meal that would normally be satisfying. This lingering hunger is often rooted in how insulin and blood glucose behave after food is consumed. When blood sugar spikes from a high-carb or high-sugar meal, insulin is released—sometimes in large amounts, especially if medication is involved. If the body is insulin resistant, it may respond inefficiently, causing the glucose to remain in the bloodstream and not reach the cells where it’s needed.
As a result, the body continues to perceive an energy shortage and sends out hunger signals. People may find themselves eating again, not because they need the calories, but because their body is stuck in a feedback loop driven by insulin dysfunction. It’s no wonder so many people with diabetes wonder, “Does diabetes make you hungry even when you’re full?” The answer, quite simply, is yes—and it’s a physiological issue, not a lack of willpower.
These blood sugar swings are not only frustrating but can also affect mood, focus, and decision-making. Over time, eating in response to blood sugar crashes can lead to a pattern of overeating, weight gain, and worsened insulin resistance, which perpetuates the hunger cycle.
Waking Up Hungry in the Middle of the Night: A Red Flag for Glucose Imbalance
If you’ve ever experienced waking up hungry in the middle of the night with diabetes, you may be dealing with nocturnal hypoglycemia. This condition occurs when blood sugar drops too low during sleep, often due to a mismatch between evening insulin doses, physical activity earlier in the day, or an imbalanced dinner. The body reacts by triggering hunger, stress hormones, and sometimes even cold sweats, shakiness, or a racing heartbeat.
This nighttime hunger is especially common in people who go to bed with borderline-low blood glucose levels or who eat dinner several hours before sleeping without a bedtime snack. In these situations, the body simply runs out of glucose fuel overnight. Once again, the cells send emergency signals for energy, leading to intense hunger that wakes you up and compels you to eat—often carbs—to raise blood sugar quickly.
Interestingly, nighttime eating can create a cascade of challenges: disrupted sleep, increased appetite the next day, and difficulty maintaining steady glucose levels. People may also struggle with poor sleep quality, which itself can exacerbate insulin resistance and hunger hormones, creating a vicious cycle that can be hard to break.
Why Some Diabetics Are Super Hungry All the Time
If you feel like you’re constantly eating but never satisfied, you’re not imagining things. Many people report being super hungry all the time as a diabetic, and this ongoing hunger can take a toll on both physical and emotional health. Beyond insulin resistance and glucose fluctuations, several other factors may be at play.
For one, high levels of inflammation—common in poorly managed diabetes—can impair how cells communicate with hunger and satiety signals. Chronic inflammation affects the hypothalamus, the part of the brain responsible for regulating appetite, further muddying the internal cues that should guide eating behavior.
Emotional stress is another culprit. Living with diabetes is a daily mental and emotional challenge, and stress itself can trigger cravings, particularly for high-carb or comfort foods. Cortisol, the body’s stress hormone, not only raises blood sugar but also stimulates appetite. This makes it more likely that someone with diabetes who is under stress will reach for food even if their body doesn’t truly need it.
Another factor is poor dietary composition. Meals that are high in simple carbs or low in fiber, protein, and healthy fats are digested quickly and lead to spikes and drops in blood sugar, which intensify hunger. By contrast, meals that promote stable glucose release can keep hunger in check for hours. In other words, it’s not just how much you eat—it’s what you eat and how it’s balanced that matters.
Natural Ways to Stop Diabetes Hunger Without Medications
While medications are an important part of diabetes management for many, there are also natural, lifestyle-based ways to reduce hunger and improve blood sugar control. Learning how to stop diabetes hunger without relying on artificial suppressants involves restoring balance to the body’s internal signals and addressing the root causes of constant cravings.
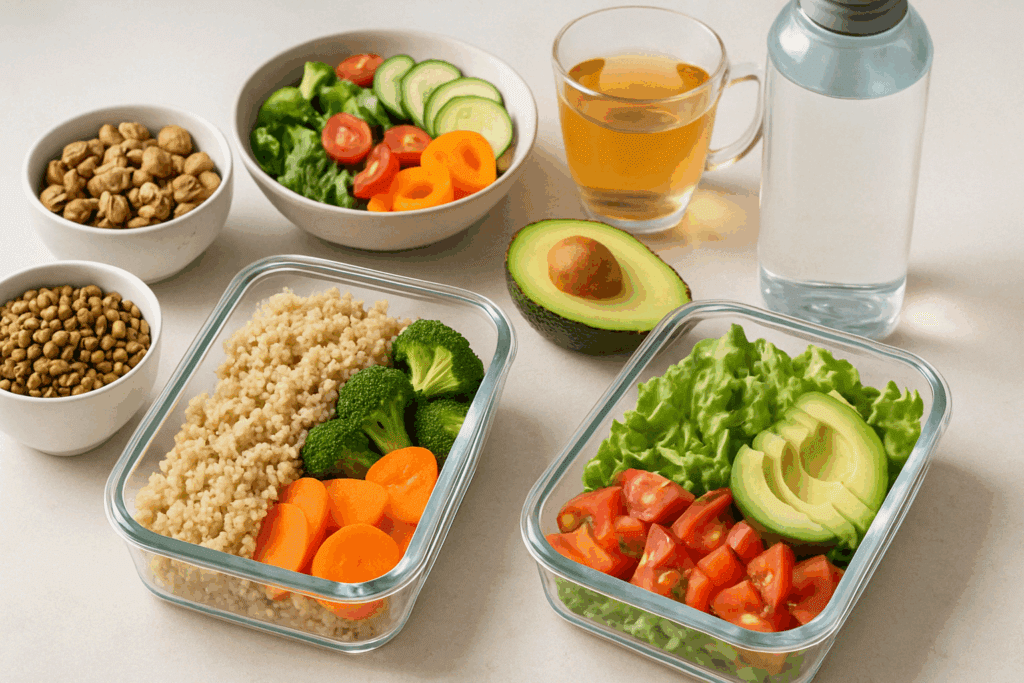
One of the most effective strategies is to eat meals rich in fiber, plant-based proteins, and healthy fats. These nutrients slow digestion, reduce blood sugar spikes, and promote a sense of fullness that lasts. For instance, a lunch with lentils, quinoa, leafy greens, and avocado is likely to keep you satisfied far longer than one made with white bread and processed deli meats.
Eating smaller, frequent meals throughout the day can also help prevent blood sugar dips and spikes that lead to hunger. Instead of three large meals, aim for three balanced meals and two snacks that include fiber and protein. A handful of almonds, a boiled egg, or a small serving of hummus with raw veggies are examples of nutrient-dense snacks that help curb hunger naturally.
Physical activity plays a critical role as well. Exercise increases insulin sensitivity, meaning your body becomes better at utilizing glucose, which reduces the risk of cells “feeling” starved. Even moderate activities like walking or yoga can make a noticeable difference in appetite regulation.
Hydration is often overlooked but essential. Mild dehydration can mimic feelings of hunger, leading people to eat when what they really need is water. Aim to drink throughout the day, especially between meals, to help distinguish true hunger from thirst.

Mindful Strategies to Address Emotional Eating and Stress-Driven Cravings
Hunger in diabetes isn’t always physical. Emotional and psychological factors can lead to cravings that feel just as intense as biological ones. For those who feel super hungry all the time, it’s worth exploring whether emotional eating is contributing to the pattern.
Mindfulness practices such as meditation, deep breathing, and even journaling can help bring awareness to emotional triggers that drive hunger. When you feel a craving coming on, pause and ask: Am I physically hungry, or am I feeling stressed, anxious, bored, or tired? This moment of awareness can interrupt automatic eating patterns and help redirect behavior in a healthier direction.
Establishing regular routines around meals, sleep, and movement can also improve hormone regulation. Sleep deprivation, for instance, increases ghrelin (the hunger hormone) and decreases leptin (the fullness hormone), setting the stage for increased appetite. Prioritizing sleep and managing stress through calming rituals can reduce the frequency and intensity of hunger, particularly at night.
Support also matters. Whether it’s a dietitian, diabetes coach, therapist, or support group, having someone to talk to can make it easier to manage hunger-related challenges. There’s no shame in seeking help, especially when appetite is affecting your quality of life or diabetes management.
Balancing Blood Sugar to Prevent Nighttime Hunger and Daytime Cravings
If you’re regularly waking up hungry in the middle of the night with diabetes, your blood sugar levels may be too low during sleep. A bedtime snack with protein and complex carbohydrates—like Greek yogurt with a sprinkle of oats or a slice of whole grain toast with peanut butter—can help provide slow-releasing energy to stabilize glucose overnight.
Avoid high-sugar evening snacks, which may cause a spike followed by a rapid drop during the night. Instead, focus on meals and snacks that support a steady glucose curve. Keeping a food journal or using a continuous glucose monitor (CGM) can help you identify patterns and pinpoint whether nighttime hunger is related to dietary habits or medication timing.
Your body’s internal clock also plays a role. Eating dinner too late or skipping meals earlier in the day can disrupt your circadian rhythm and alter how your body processes glucose during sleep. Aim for consistent meal timing and make sure you’re not under-eating during the day, which can trigger compensatory hunger at night.
FAQ: Understanding and Managing Diabetes Hunger
This standalone FAQ is designed to expand on the insights from the article “Why Does Diabetes Make You So Hungry?” and offers advanced, reader-focused answers that address common concerns while incorporating new perspectives, practical solutions, and natural approaches to managing diabetes-related hunger. Each answer aligns with SEAT standards and integrates the focus keyword phrases naturally, without redundancy.
1. Can dehydration worsen diabetes hunger or mimic hunger symptoms?
Absolutely, and it’s a commonly overlooked factor. Dehydration can intensify or even mimic feelings of hunger, leading people with diabetes to eat more when what their body actually needs is water. Because high blood glucose can cause frequent urination, people with diabetes are more prone to dehydration, especially if their blood sugar isn’t well managed. When you’re super hungry all the time as a diabetic, it’s worth first checking your fluid intake. Drinking a glass of water and waiting 15 minutes can help differentiate true diabetes hunger from thirst-driven cravings. This strategy is particularly helpful for those seeking practical methods for how to stop diabetes hunger without immediately turning to food.
2. How does stress management help reduce diabetes-related hunger?
Stress significantly influences appetite regulation through hormonal pathways, especially by increasing cortisol levels. Chronic stress not only raises blood sugar but also disrupts insulin sensitivity and heightens cravings—usually for sugary, high-calorie comfort foods. For someone asking, “Why does diabetes make you hungry during stressful times?”, the answer lies in this biochemical response. Implementing daily stress-reduction techniques like deep breathing, short walks, or mindfulness practices can curb diabetes hunger before it spirals into overeating. For individuals who feel super hungry all the time as a diabetic, stress management may be a missing link in their blood sugar and hunger regulation strategy.
3. Could nutrient deficiencies contribute to diabetes hunger?
Yes, emerging evidence suggests that deficiencies in key nutrients—such as magnesium, chromium, and vitamin D—may impact hunger cues and insulin efficiency. Magnesium, in particular, supports glucose metabolism and insulin signaling, and low levels have been linked to increased appetite and insulin resistance. If you’re waking up hungry in the middle of the night with diabetes, or struggling to feel full during the day, it may be worth checking your micronutrient status. Incorporating foods rich in these nutrients or using medically guided supplementation could help rebalance satiety hormones and reduce diabetes hunger naturally. This approach adds another layer to understanding how to stop diabetes hunger by addressing its nutritional root causes.
4. Why does exercise sometimes increase appetite in diabetics, and how can it be managed?
While regular physical activity improves insulin sensitivity and helps control blood glucose, some people notice increased appetite post-workout. This can be confusing, especially when trying to curb diabetes hunger. The key lies in the type and timing of exercise. High-intensity or prolonged workouts may deplete glycogen stores and stimulate hunger, while light to moderate activity like walking or resistance training tends to stabilize appetite. If you’re super hungry all the time as a diabetic after workouts, consider adjusting your pre- and post-exercise meals to include complex carbs, fiber, and protein to avoid blood sugar crashes. Smart fueling strategies can help prevent waking up hungry in the middle of the night with diabetes due to energy deficits from earlier activity.
5. Can medication timing or type affect nighttime hunger in people with diabetes?
Yes, and this is a critical but often under-discussed topic. Certain diabetes medications—particularly long-acting insulins or sulfonylureas—can cause blood sugar to dip overnight if taken too late in the evening or without adequate food. This drop can lead to waking up hungry in the middle of the night with diabetes due to a hypoglycemic response. Adjusting medication timing or discussing alternative treatment plans with your healthcare provider may reduce these overnight hunger episodes. Understanding how to stop diabetes hunger in this context may involve more precise medication management rather than dietary changes alone. Always consult a diabetes specialist when modifying any aspect of your medication routine.
6. How does poor sleep quality influence diabetes hunger the next day?
Disrupted or insufficient sleep impairs the regulation of ghrelin and leptin—two key hormones that control appetite and fullness. When these hormones are unbalanced, you may wake up craving high-carb foods or experience diabetes hunger that seems unrelated to your actual energy needs. This explains why people with erratic sleep patterns often feel super hungry all the time as a diabetic, even with a balanced diet. Additionally, poor sleep can lead to insulin resistance, making glucose control more difficult. Improving sleep hygiene may be one of the most overlooked yet effective strategies for how to stop diabetes hunger, especially when paired with consistent meal timing and stress reduction.
7. Is it possible to retrain your body’s hunger signals if you have diabetes?
Yes, and this concept is at the core of mindful eating practices. Chronic blood sugar dysregulation can dull the body’s ability to accurately signal hunger and fullness, but these signals can often be retrained through conscious, consistent effort. By tracking how different meals impact your energy and appetite levels, and by slowing down during meals to assess satiety, you begin to recalibrate internal cues. This is especially helpful for those who are super hungry all the time as a diabetic and unsure when hunger is real versus habitual. For those wondering how to stop diabetes hunger long-term, cultivating body awareness through journaling, glucose monitoring, and structured meal planning can be transformative.
8. Can gut health affect how hungry you feel with diabetes?
Absolutely. The gut microbiome plays a major role in regulating blood sugar, insulin sensitivity, and appetite. An imbalance in gut bacteria—commonly caused by a low-fiber diet, antibiotics, or chronic stress—can lead to increased inflammation and abnormal hunger signaling. This disruption may contribute to diabetes hunger that feels constant or hard to manage. Adding more prebiotic-rich foods like garlic, onions, and asparagus, or fermented foods like sauerkraut and kefir, can support a healthier microbiome. For anyone who is super hungry all the time as a diabetic, gut health should not be overlooked as part of a comprehensive strategy for how to stop diabetes hunger naturally.
9. How do hormonal fluctuations outside of insulin influence hunger in diabetics?
In addition to insulin, hormones like cortisol, glucagon, and even estrogen and testosterone can influence hunger patterns in people with diabetes. For example, elevated cortisol from chronic stress can increase fat storage and cravings, while low testosterone or estrogen may disrupt metabolic efficiency and satiety signals. These hormonal imbalances may help explain why some individuals experience waking up hungry in the middle of the night with diabetes, even if blood sugar appears stable. Working with an endocrinologist to assess hormonal health can uncover hidden contributors to persistent diabetes hunger. Integrating hormonal balance into your wellness strategy is another sophisticated approach to how to stop diabetes hunger at its root.
10. Are there emerging technologies that can help monitor and reduce diabetes hunger?
Yes, continuous glucose monitors (CGMs) and AI-driven nutrition apps are revolutionizing how people manage their hunger and blood sugar in real time. CGMs allow users to see exactly how different foods and activities affect their glucose levels, helping them identify patterns that contribute to diabetes hunger. Some advanced apps even use this data to suggest meal timing and composition to prevent blood sugar crashes that lead to cravings. For those who feel super hungry all the time as a diabetic, these tools offer unprecedented insight and personalization. By combining technology with mindful habits, many are discovering new pathways for how to stop diabetes hunger effectively and sustainably.
Conclusion: Reclaiming Balance by Understanding and Managing Diabetes Hunger
Living with diabetes can be a constant balancing act, and when hunger becomes relentless, it can feel like your body is working against you. But by understanding the biology behind diabetes hunger, you can begin to address the root causes and implement natural, sustainable strategies to take back control. Whether you’re feeling super hungry all the time as a diabetic or waking up hungry in the middle of the night, these signals are your body’s way of asking for better balance—not punishment or restriction.
Learning how to stop diabetes hunger naturally means moving away from cycles of sugar spikes and crashes, and toward steady, nourishing habits that support your metabolic and emotional well-being. This includes balanced meals, mindful eating, stress reduction, proper hydration, and quality sleep. And while no single change will solve everything overnight, small, consistent improvements can transform how you feel—and how your body responds.
If you’ve been asking, “Does diabetes make you hungry?” the answer is yes, but it doesn’t have to stay that way. With awareness, education, and intentional choices, you can reduce constant cravings, improve energy, and build a lifestyle that supports long-term health—naturally and powerfully.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Why Do Diabetic Patients Always Feel Hungry ?
Diabetic Hyperphagia: Why You’re Always Hungry
Understanding your body’s appetite drive
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.

