Understanding the Connection Between Diabetes and Sugar Cravings
For many individuals living with diabetes, managing blood sugar levels is a delicate and ongoing process. Yet one of the most perplexing—and often frustrating—symptoms for some is an intense desire for sugary foods. These cravings can feel almost insatiable and may seem paradoxical considering that diabetes is a condition defined by problems with glucose regulation. So, why do diabetics crave sugar? The answer lies in a complex interplay of physiological, psychological, and hormonal factors that are closely tied to insulin resistance, glucose metabolism, and even emotional well-being.
People often assume that craving sugar means diabetes, or wonder, “Is craving sugar a symptom of diabetes?” These questions are not only common, but valid. The link between craving sugar and diabetes is not just anecdotal—it has scientific roots that tie into the very mechanisms by which the body manages energy. When insulin does not function properly, as is the case in both Type 1 and Type 2 diabetes, cells are unable to effectively absorb glucose from the bloodstream. This, in turn, can lead to low cellular energy levels even when blood glucose is high, prompting the brain to signal a desire for more sugar.
Understanding this process is crucial not only for those managing diabetes, but also for individuals concerned about symptoms such as persistent sweet cravings. It raises important questions such as: does diabetes make you crave sugar? Is craving sweets a sign of diabetes? By exploring these connections in depth, we can begin to demystify the biology behind these urges—and offer practical strategies for managing them.
You may also like: Why Am I Craving Sweets All of a Sudden? Expert-Backed Reasons and How to Stop Sugar Cravings Naturally
How Insulin Resistance Fuels Cravings for Sugar
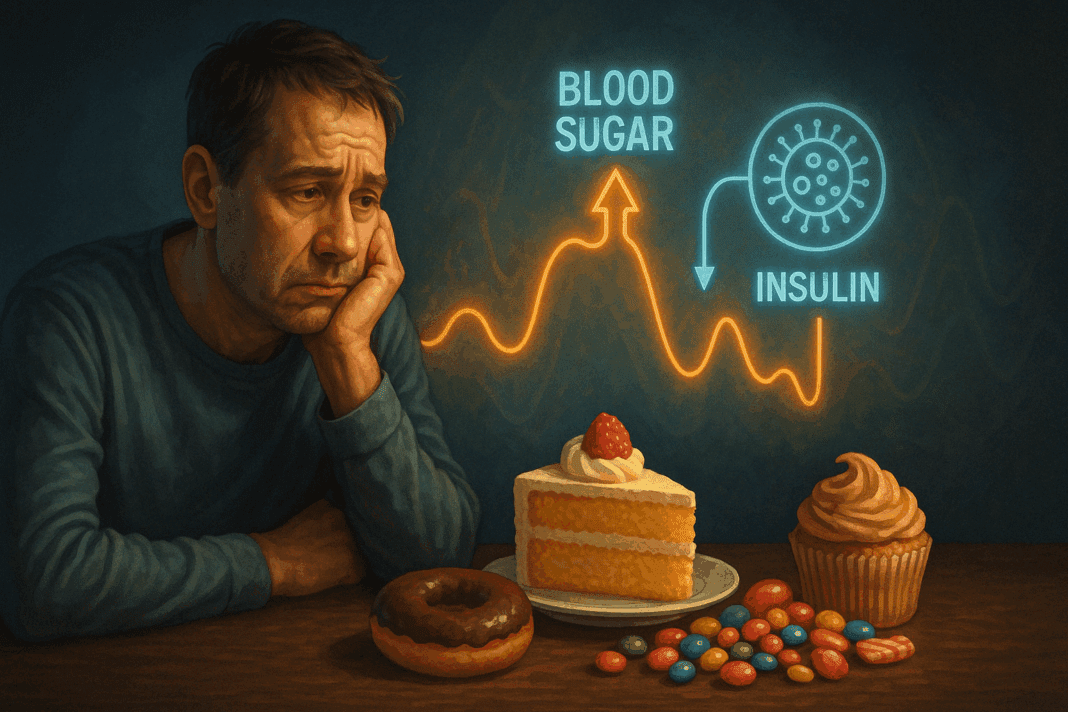
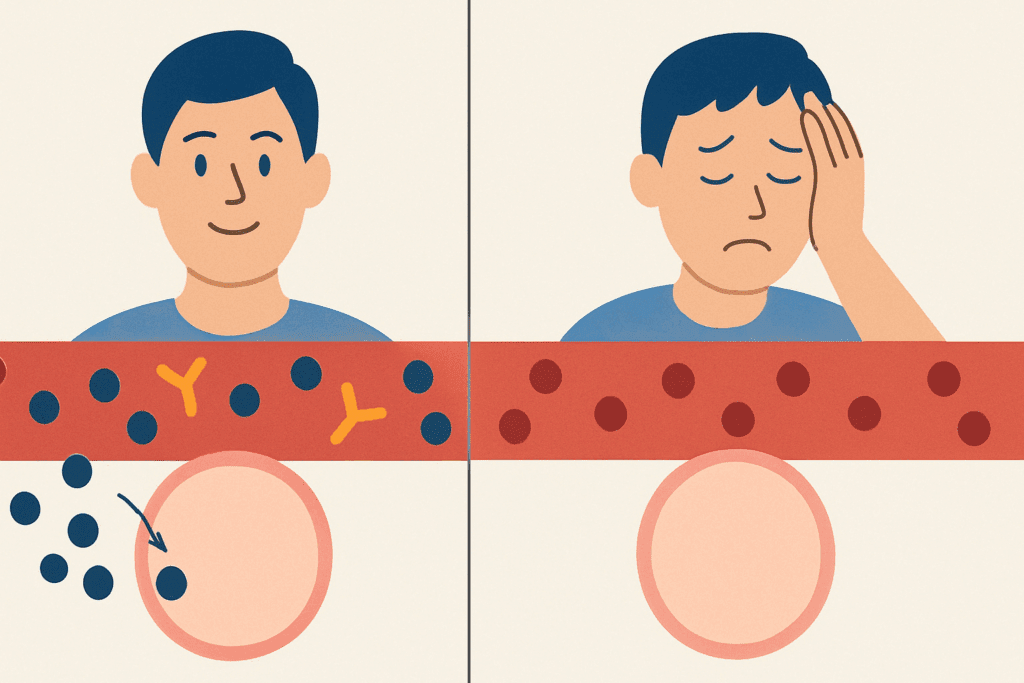
Insulin is a hormone produced by the pancreas that allows glucose to enter cells and be used for energy. In people with insulin resistance, the body’s cells become less responsive to insulin, making it harder for glucose to be absorbed. As a result, blood sugar levels may remain elevated, while cells are left starved for fuel. This paradox—the presence of excess glucose in the blood alongside energy-deprived cells—can trigger the brain to initiate hunger signals, especially for quick sources of energy like sugar.
This biological signal is part of why diabetics may crave sugar even when their blood sugar is already high. The brain perceives a lack of usable energy and demands a fast fix. That fix often comes in the form of sweet foods, which are rapidly absorbed and give the impression of energy restoration. However, consuming more sugar only exacerbates the cycle, contributing to further spikes in blood glucose, followed by crashes that once again trigger cravings. This feedback loop helps explain why diabetics crave sugar and why it can be so difficult to resist those urges.
Moreover, insulin resistance is often a silent condition that develops over years. People may notice increased cravings long before they are formally diagnosed with diabetes. In that sense, craving sugar may indeed be an early warning sign. It’s understandable, then, why someone might wonder whether craving sugar means diabetes. While not a definitive diagnostic tool, increased cravings can certainly serve as a cue to get blood glucose levels checked.
Hypoglycemia and the Body’s Emergency Signals
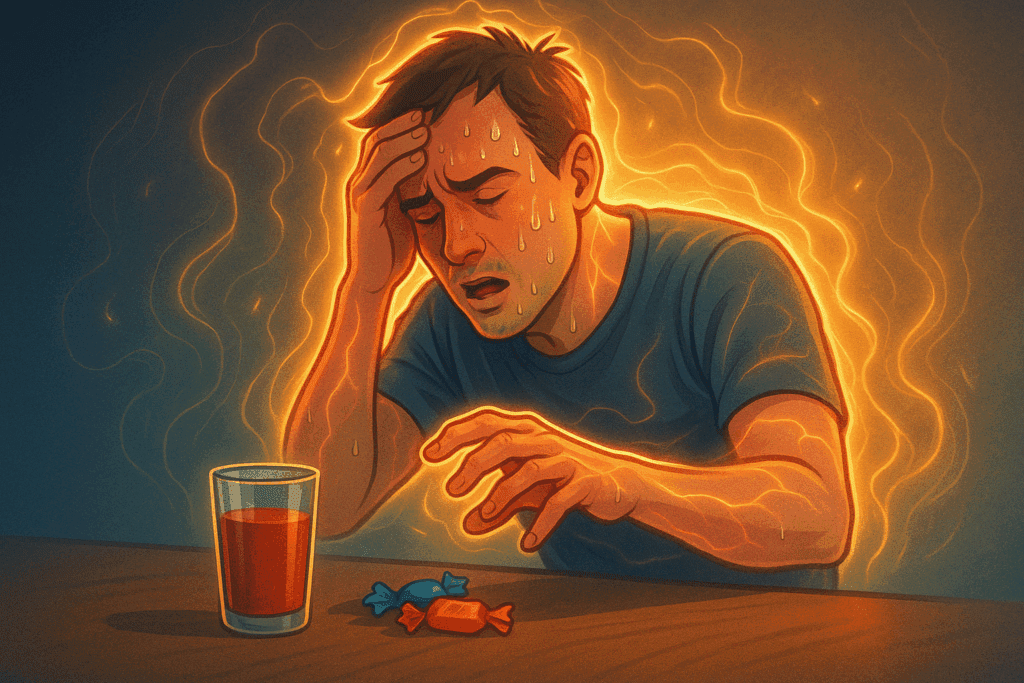
One of the most immediate causes of sugar cravings in people with diabetes is hypoglycemia—a drop in blood sugar to dangerously low levels. Hypoglycemia can occur for several reasons, including taking too much insulin, skipping meals, or overexerting oneself physically. When blood sugar drops, the body activates an emergency response system designed to correct the imbalance. This includes the release of adrenaline and cortisol, which stimulate hunger and often drive the desire for sugar.
The symptoms of hypoglycemia are both physical and psychological. People may feel shaky, dizzy, sweaty, or irritable. More importantly, they may feel an overwhelming need to consume something sweet. In this context, sugar cravings serve a physiological function: they are the body’s way of pushing us toward rapidly digestible carbohydrates that can restore normal glucose levels quickly. But for someone managing diabetes, this can be a double-edged sword. Overcompensating by consuming too much sugar can lead to another spike in blood glucose levels, perpetuating a dangerous rollercoaster.
This scenario illustrates a key reason why diabetics crave sugar—it’s not always about habit or preference. Sometimes, it’s a life-saving signal. Still, recognizing the difference between a legitimate hypoglycemic episode and a psychologically driven craving is essential for good diabetes management. For many, this distinction isn’t easy to make, and it’s what leads people to ask questions like “Does diabetes make you crave sugar?” or “Is craving sugar a symptom of diabetes?” These are not just medical questions—they’re part of the lived experience of those managing this complex condition.
The Role of Leptin, Ghrelin, and Dopamine in Sweet Cravings
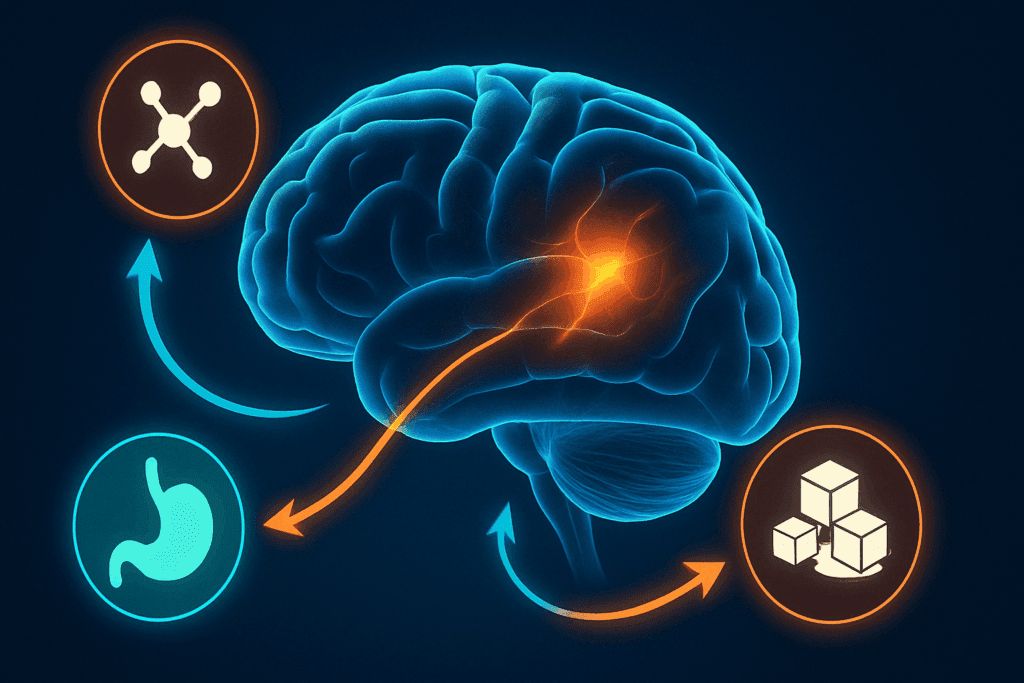
Beyond insulin, a host of other hormones also play significant roles in shaping our cravings. Leptin and ghrelin—commonly referred to as the hunger and satiety hormones—are key players. In individuals with insulin resistance or diabetes, the normal balance of these hormones can be disrupted. Ghrelin levels may remain elevated, signaling constant hunger, while leptin resistance may develop, making it harder to feel full after eating. This hormonal imbalance creates a fertile ground for cravings, especially for calorie-dense and sugar-rich foods.
Another hormonal factor is dopamine, a neurotransmitter that governs the brain’s reward system. When we eat sugar, dopamine is released, producing feelings of pleasure and satisfaction. Over time, this reward mechanism can become hyperactive, especially in the presence of repeated sugar consumption. This can condition the brain to associate sugar with emotional comfort, stress relief, or even a sense of safety. Thus, for people with diabetes who already have dysregulated glucose and insulin levels, the brain’s reward system may further reinforce cravings, making them more intense and harder to resist.
This biochemical interplay can help explain why diabetics crave sweets in a way that feels more urgent or habitual than in those without blood sugar issues. It also highlights that craving sugar diabetes is not just about willpower or dietary choices. It’s about managing a complex web of hormonal signals that influence behavior, appetite, and emotional well-being. Understanding these mechanisms can empower individuals to take a more compassionate and informed approach to their cravings.

Emotional Triggers and Psychological Conditioning
While biology plays a foundational role, emotional and psychological factors cannot be overlooked. For many people with diabetes, food—especially sugary food—serves as a coping mechanism. Whether it’s dealing with the stress of disease management, emotional burnout, or simply the psychological fatigue that comes with chronic illness, sweets often become a form of self-soothing.
This behavior is rooted in both cultural conditioning and neurobiology. From a young age, many of us are taught to associate sweets with rewards, comfort, and celebration. For people dealing with diabetes, the deprivation of certain foods can paradoxically heighten the desire for them. The forbidden nature of sugar can make it all the more tempting, particularly during periods of emotional distress. Over time, this can create a feedback loop in which cravings are not just physiological responses, but also learned behaviors.
The question “does diabetes make you crave sweets?” can’t be fully answered without acknowledging this psychological layer. Cravings are not always rational—they are often emotional and tied to past experiences or current mental states. Strategies that only address the physical aspect of diabetes without accounting for emotional health are often incomplete. This is why comprehensive diabetes care must include psychological support, stress management techniques, and mindful eating practices.
Craving Sugar Before Diagnosis: A Potential Red Flag
One of the more subtle aspects of sugar cravings is that they often begin before a formal diagnosis of diabetes. This is particularly true in cases of prediabetes or undiagnosed Type 2 diabetes, where blood sugar regulation is already impaired but has not yet reached clinical thresholds. In these cases, individuals may begin to notice an unusual frequency or intensity of sugar cravings without understanding why.
This is where the question “is craving sweets a sign of diabetes?” becomes particularly relevant. While sugar cravings alone are not enough to diagnose diabetes, they can serve as an important clue when considered alongside other symptoms such as fatigue, increased thirst, frequent urination, or blurred vision. If multiple signs are present, it is worth exploring whether craving sugar means diabetes is developing.
Medical professionals increasingly recognize the importance of early detection in preventing or delaying the onset of full-blown diabetes. Recognizing craving sugar diabetes as a potential early indicator, especially when coupled with family history or lifestyle factors, can prompt earlier testing and intervention. This proactive approach not only supports physical health but also empowers individuals to make informed dietary and lifestyle choices before the condition progresses.

Managing Cravings with Mindful Nutrition
So what can be done when these cravings strike? Fortunately, there are evidence-based strategies that can help manage sugar cravings in people with diabetes without resorting to deprivation or restriction. One of the most powerful approaches is mindful eating—a practice that involves slowing down, savoring food, and becoming more attuned to the body’s hunger and satiety cues.
Mindful eating encourages individuals to observe their cravings without judgment and to investigate their origins. Are they stemming from genuine hunger, emotional distress, or blood sugar fluctuations? By asking these questions in real-time, people can make more intentional food choices that align with their health goals. Over time, this practice can help break the automatic habit loop that often underlies sugar cravings.
Additionally, focusing on balanced meals that include high-quality protein, healthy fats, and fiber can help stabilize blood sugar levels and reduce the likelihood of energy crashes that trigger sweet cravings. These nutrients slow the absorption of glucose, providing sustained energy and preventing the spikes and crashes that exacerbate cravings. In this way, addressing the question “why do diabetics crave sugar?” becomes an invitation to explore nutritional strategies that support stability and satisfaction.
Substituting Sweets Without Sacrificing Satisfaction
Completely eliminating sweet foods is neither realistic nor necessary for most people with diabetes. Instead, the goal should be to substitute high-glycemic sweets with more nutrient-dense alternatives. Naturally sweet foods like berries, apples, and citrus fruits can provide the pleasure of sweetness while delivering fiber, vitamins, and antioxidants. Pairing these fruits with a small amount of protein or fat—such as almond butter or yogurt—can further stabilize blood sugar.
There are also numerous recipes and products designed specifically for people with diabetes that satisfy the desire for something sweet without causing large glucose spikes. These include treats made with stevia, monk fruit, or erythritol, which offer sweetness without the blood sugar impact of traditional sugar. Understanding these options can empower individuals to satisfy cravings in a way that aligns with their health needs.
The persistent question—“is craving sugar a sign of diabetes?”—becomes less alarming when individuals are equipped with tools and strategies to manage those cravings effectively. Education, rather than restriction, is the key to creating a sustainable and empowered relationship with food. Recognizing that these cravings are biologically and psychologically complex helps eliminate guilt and promote healthier long-term habits.
Lifestyle Factors That Influence Cravings
Beyond diet, a variety of lifestyle factors can impact how often and how intensely someone craves sugar. Lack of sleep, for example, has been shown to impair glucose metabolism and increase levels of ghrelin, the hunger hormone. Chronic sleep deprivation can therefore lead to increased cravings—not just for any food, but specifically for high-carbohydrate, high-sugar options. Similarly, physical inactivity contributes to insulin resistance, compounding the problem of unstable blood sugar and subsequent cravings.
Stress is another major player. When we are stressed, cortisol levels rise, which can increase appetite and drive a preference for sweet and fatty foods. For someone managing diabetes, this creates yet another feedback loop: stress worsens blood sugar control, which in turn increases cravings, which may then lead to poor food choices, perpetuating both physiological and emotional stress.
Understanding these broader lifestyle factors allows individuals to see the full picture. It’s not just about asking “does diabetes make you crave sugar?”—it’s also about recognizing the external and internal conditions that may be amplifying those cravings. Sleep hygiene, regular physical activity, and stress reduction techniques such as meditation, yoga, or therapy can all play vital roles in supporting more stable glucose levels and reducing the frequency and intensity of sugar cravings.
The Importance of Compassionate Diabetes Care
Ultimately, one of the most effective ways to manage cravings is through compassionate and comprehensive care. When people feel judged or shamed for their food choices, it becomes harder to make positive changes. Instead of labeling cravings as bad or viewing them as signs of failure, it’s more productive to approach them with curiosity and self-compassion.
This mindset shift can significantly improve the way individuals manage their diabetes. Rather than asking “is craving sugar a symptom of diabetes?” as if it were a flaw or a weakness, people can begin to understand that cravings are a form of communication from the body. When understood correctly, they offer valuable information about blood sugar balance, emotional state, and nutritional needs.
Healthcare providers can support this process by validating the complexity of cravings and offering practical, individualized strategies. Registered dietitians, diabetes educators, and mental health professionals can work together to provide integrated support that addresses not just the physical aspects of diabetes, but also the emotional and psychological ones. This holistic approach ensures that cravings are not seen as the enemy, but as an opportunity for deeper understanding and more effective management.
Conclusion: Rethinking Sugar Cravings in Diabetes With Insight and Strategy
Understanding why diabetics crave sugar is not about pointing fingers or reinforcing myths. It’s about recognizing the intricate biological, psychological, and lifestyle-driven mechanisms that drive these cravings—and responding with knowledge, compassion, and strategy. Whether sugar cravings arise from insulin resistance, hormonal imbalances, emotional distress, or hypoglycemic episodes, they are a real and valid part of the diabetes experience.
Rather than viewing these cravings as a failure of willpower, we can reframe them as a call for balance—an opportunity to fine-tune blood sugar regulation, enhance nutritional practices, and improve emotional resilience. For those who wonder whether craving sugar means diabetes or ask, “Is craving sweets a sign of diabetes?” the answer is nuanced. Cravings can indeed be a signal that something in the body’s regulatory system is out of balance, and they warrant both attention and care.
By integrating mindful eating, targeted nutrition, lifestyle adjustments, and psychological support, people with diabetes can reduce the frequency and intensity of sugar cravings without feeling deprived or overwhelmed. In doing so, they take meaningful steps toward a healthier, more empowered life—one where sweetness can be enjoyed in moderation and with intention, rather than feared or forbidden.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Understanding the science behind sugar and cravings
Why Do Diabetics Crave Sweets?
20 Reasons for Blood Sugar Swings
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.