Sleep is often viewed as a time of rest, restoration, and recovery. Yet for some individuals, the boundary between wakefulness and sleep becomes blurred in ways that impact their health, nutrition, and overall quality of life. One such phenomenon is known as a sleep eating disorder, more formally categorized under parasomnias—disruptive sleep-related behaviors. Often misunderstood or mistaken for poor dietary habits or emotional eating, this condition involves involuntary episodes of eating while in a sleep-like state. In many cases, individuals have no memory of these nocturnal episodes. This complex and often hidden disorder intertwines neurological, psychological, and nutritional dimensions, making it particularly relevant to discussions around mindful eating and healthier lifestyles.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
The term “sleep related eating disorder” (SRED disorder) may sound obscure, but it has garnered increased attention among sleep medicine professionals, mental health practitioners, and nutrition experts alike. As people increasingly seek better ways to balance wellness through diet, sleep hygiene, and stress management, awareness of disorders like sleep eating becomes more important. While the idea of sleepwalking and eating may seem curious or even humorous at first glance, its consequences can be quite serious—ranging from unintentional weight gain and poor nutritional choices to physical injury and disrupted sleep cycles. Exploring the causes, symptoms, risks, and treatment options for this condition offers not only a deeper understanding of human behavior during sleep but also practical tools for promoting long-term mental and physical health.

What Is Sleep Eating Disorder and How Does It Manifest?
A sleep eating disorder is classified as a type of parasomnia—abnormal behaviors that occur during sleep, particularly during transitions between different sleep stages. It typically arises during non-REM (rapid eye movement) sleep and is marked by partial arousal. During these episodes, individuals may find themselves preparing and consuming food with little to no conscious awareness. In some cases, these activities are complex and involve operating kitchen appliances or navigating stairs, which poses considerable risks.
Unlike typical nighttime snacking or emotional eating, sleep eating occurs without full awareness. This distinguishes it from behaviors that are driven by stress, boredom, or cravings. While individuals might recognize evidence of eating—such as food remnants or missing items—they often cannot recall the episode itself. This lack of memory is one of the defining features of a sleep related eating disorder, further complicating diagnosis and treatment.
The foods consumed during sleep eating episodes are often high in sugar, fat, or salt—suggesting a possible neurological drive toward energy-dense, easily accessible calories. This preference may stem from the brain’s attempt to satisfy unmet energy needs, a hypothesis supported by studies linking sleep deprivation with increased cravings for unhealthy foods. It is not uncommon for individuals to consume raw or frozen items, combinations that would be unappetizing when awake, or even non-food substances in extreme cases.
Understanding the Link Between Sleepwalking and Eating
The connection between sleepwalking and eating lies in shared neurological pathways. Both behaviors stem from partial arousal during deep sleep, often resulting in motor activity without full cognitive control. This state is sometimes referred to as “confusional arousal,” and it can be triggered by sleep deprivation, stress, or disruptions in the circadian rhythm. Individuals with a history of other parasomnias—such as sleepwalking, night terrors, or talking in their sleep—may be more prone to developing a sleep eating disorder.
What complicates the relationship further is the tendency for these behaviors to go undetected. Unless another person witnesses the behavior or the individual injures themselves or makes a mess, sleep eating can remain a mystery. Over time, however, patterns may emerge—such as unexplained weight gain, missing food, or signs of cooking during the night. For those who live alone, these signs can be difficult to interpret and may be dismissed as forgetfulness or stress-related lapses.
Research into sleepwalking and eating suggests that neurological, genetic, and environmental factors all play a role. Family history of parasomnias, irregular sleep patterns, and high levels of life stress can all increase susceptibility. Medications that affect the central nervous system—particularly sedative-hypnotics and certain antidepressants—have also been linked to increased episodes of sleep-related behaviors, including sleep eating.

Why Sleep Eating Deserves Clinical and Nutritional Attention
While sleep eating might initially appear to be a behavioral quirk, it holds significant implications for an individual’s mental and physical well-being. From a clinical perspective, a sleep eating disorder can disrupt the architecture of restorative sleep, leaving individuals fatigued, foggy, and more susceptible to mood disturbances. Nutritionally, repeated nighttime consumption of high-calorie foods can lead to weight gain, metabolic issues, and disordered eating patterns that persist during waking hours.
Because these behaviors are involuntary and typically occur without awareness, they are difficult to manage through willpower or conventional diet strategies. This makes sleep eating a unique and challenging disorder within the broader context of mindful eating. For individuals striving to build a healthier lifestyle, it’s essential to recognize that some eating patterns may not stem from poor choices but rather from sleep-related disturbances beyond their control.
Sleep eating also intersects with mental health conditions such as anxiety, depression, and obsessive-compulsive tendencies. In some cases, individuals with an existing eating disorder—such as binge eating disorder or bulimia—may also experience nocturnal eating episodes, complicating both diagnosis and treatment. The overlap between mental health, sleep disorders, and nutrition underscores the need for a comprehensive, interdisciplinary approach.
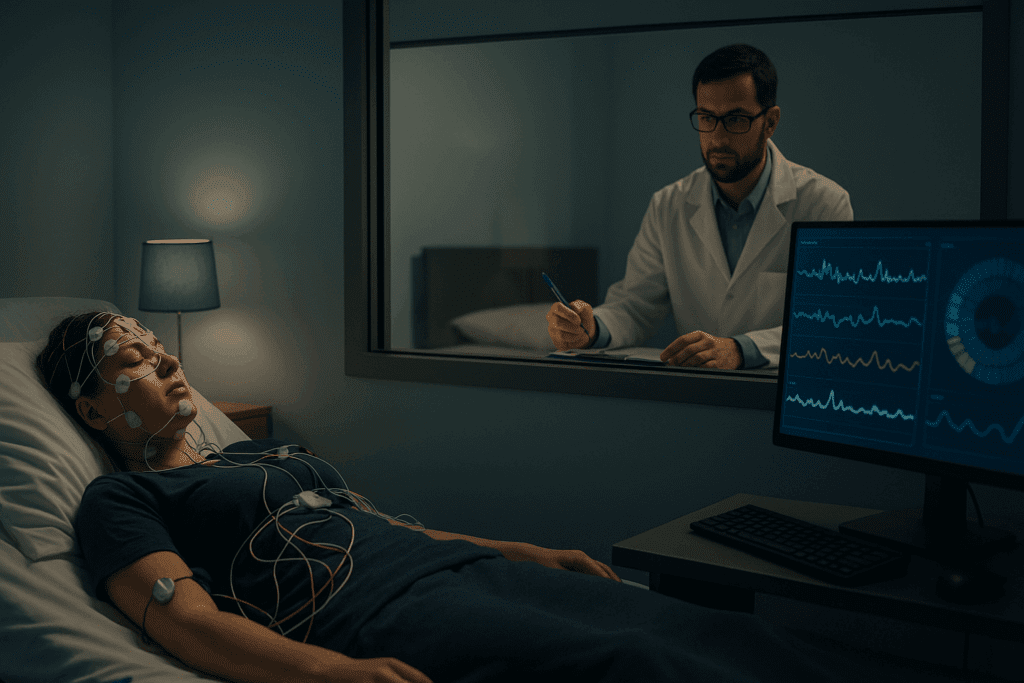
Diagnosing Sleep Related Eating Disorder: Challenges and Tools
Diagnosis of a sleep related eating disorder is often delayed due to its covert nature. Many people are unaware that their nighttime eating episodes are a medical concern, and those who suspect an issue may hesitate to seek help due to embarrassment or self-doubt. Clinicians typically begin with a thorough sleep history, including inquiries about sleep hygiene, stress levels, substance use, and family history of parasomnias.
Polysomnography, also known as a sleep study, may be recommended to observe nighttime behavior and brain activity. In some cases, a video recording is used to capture the individual’s actions during sleep. These tools help differentiate between sleep eating disorder and other conditions such as nocturnal eating syndrome (NES), which involves conscious eating during nighttime awakenings rather than unconscious episodes.
Another diagnostic challenge lies in distinguishing between sleep eating and medication-induced behaviors. Certain medications—particularly those that affect GABA receptors or suppress REM sleep—can increase the likelihood of parasomnias. A careful review of medications, including over-the-counter sleep aids, is critical in identifying potential contributing factors. In some cases, modifying or discontinuing these medications can significantly reduce or eliminate episodes.
Treatment Approaches for Managing Sleep Eating Disorder
Because sleep eating disorder is multifaceted, treatment often involves a combination of strategies tailored to the individual’s needs. Behavioral interventions are often the first step, particularly those aimed at improving sleep hygiene. Maintaining a consistent sleep schedule, avoiding stimulants in the evening, and creating a calming pre-sleep routine can all reduce the likelihood of partial arousal episodes.
Cognitive-behavioral therapy (CBT) may also be beneficial, especially when sleep eating is associated with anxiety or stress. CBT techniques help individuals manage underlying psychological triggers and improve their relationship with food. When nutritional deficiencies or poor daytime eating habits are identified, a consultation with a registered dietitian may help address imbalances that could contribute to nighttime cravings.
In more severe or persistent cases, medication may be considered. Options such as selective serotonin reuptake inhibitors (SSRIs), topiramate, or clonazepam have shown some effectiveness in reducing sleep-related behaviors. However, medication is generally used with caution due to potential side effects and the risk of dependency. Treatment plans should always be developed collaboratively, with regular monitoring and adjustments based on progress and side effects.
Environmental modifications can also support safety and prevention. Locking up high-risk items, using kitchen alarms, or installing motion-sensor lights may deter dangerous behaviors during sleep episodes. Loved ones and roommates can play a supportive role by helping to monitor nighttime activity and encouraging individuals to seek professional guidance.

The Role of Nutrition and Sleep Hygiene in Recovery
Addressing a sleep eating disorder through nutrition and lifestyle changes is a vital part of long-term management. Ensuring that daytime meals are balanced, satisfying, and rich in complex carbohydrates and proteins can reduce the likelihood of the body seeking energy during the night. Nutrient deficiencies, particularly in magnesium, vitamin D, or B-complex vitamins, may also play a role in sleep disturbances and should be addressed through dietary assessments or supplementation when needed.
Sleep hygiene practices are equally important in reducing sleep disruptions that can trigger confusional arousals. Strategies such as maintaining a regular bedtime, minimizing screen exposure before bed, and creating a dark, quiet, and cool sleep environment can significantly improve sleep quality. Reducing alcohol and caffeine intake, particularly in the late afternoon and evening, can further stabilize sleep cycles and decrease the frequency of parasomnias.
Mindfulness techniques, including meditation, breathing exercises, and body scanning, can help individuals cultivate greater awareness of their body’s needs and responses. When practiced regularly, these techniques may enhance relaxation, reduce stress, and support healthier sleep patterns—all of which contribute to reducing sleep eating episodes. Integrating mindfulness into one’s approach to nutrition and self-care creates a powerful foundation for long-term change.

Real-Life Impact and Personal Stories
For those who experience a sleep eating disorder, the condition can have profound personal and social consequences. Feelings of confusion, shame, and frustration are common, particularly when loved ones misunderstand the behavior as a lack of discipline or self-control. Individuals may go to great lengths to conceal evidence of their episodes, further contributing to isolation and emotional distress.
Real-life accounts often highlight the unpredictability and hidden toll of sleep eating. One person might wake up to find chocolate smears on their sheets and no memory of how it happened. Another may discover a trail of crumbs leading to the kitchen, or worse, a stove left on or broken glass scattered across the floor. These moments can be jarring, raising valid concerns about personal safety and emotional well-being.
Sharing these experiences through support groups, therapy, or online communities can offer validation and connection. It also helps to shift the narrative from self-blame to curiosity and compassion. Understanding that sleepwalking and eating are involuntary behaviors rooted in complex neurobiology empowers individuals to seek effective help and take proactive steps toward healing.
Frequently Asked Questions: Sleep Eating Disorder and Sleepwalking with Food Consumption
1. Can sleep eating disorder be triggered by changes in diet or nutrition? Yes, nutritional deficiencies can play a surprising role in the onset or worsening of a sleep related eating disorder. Individuals with insufficient intake of magnesium, B-complex vitamins, or tryptophan may experience more disrupted sleep, which can increase vulnerability to parasomnias like sleep eating. A poorly balanced diet—especially one lacking in complex carbohydrates and protein—can leave the body craving energy during the night, potentially setting off involuntary eating episodes. This does not mean that diet alone causes sleep eating disorder, but nutrition is an important piece of the puzzle. Holistic treatment approaches that include dietary optimization may help stabilize energy levels and reduce the likelihood of sleepwalking and eating episodes.
2. How is sleep eating disorder different from night eating syndrome (NES)? While both conditions involve nighttime eating, they are distinct in key ways. A sleep eating disorder involves unconscious behavior, often during partial arousals from deep sleep, and the person typically has little or no memory of the episode. In contrast, night eating syndrome involves conscious awareness and is often driven by stress, anxiety, or disrupted circadian rhythms. NES sufferers might wake up deliberately to eat, while individuals with a sleep eating disorder are unaware and often confused upon discovering evidence of eating. These distinctions are crucial for accurate diagnosis and selecting the appropriate treatment strategy for each condition.
3. Is sleepwalking and eating more common in people with other sleep disorders? Yes, sleep eating often co-occurs with other sleep disorders, particularly those involving arousals from deep sleep. People with obstructive sleep apnea, restless legs syndrome, or chronic insomnia may be at higher risk of developing sleep eating behaviors. These conditions fragment the sleep cycle and increase the chances of partial awakenings, which can trigger parasomnias. It’s not uncommon for individuals who already experience sleepwalking to develop a sleep eating disorder later, as the behaviors share neurological origins. Early detection and management of coexisting sleep issues may prevent the progression to more complex disorders like SRED.
4. Can stress or trauma contribute to the development of a sleep eating disorder? Absolutely. Psychological stress and trauma are significant contributors to the development and exacerbation of a sleep related eating disorder. Stress activates the hypothalamic-pituitary-adrenal (HPA) axis, which can interfere with sleep quality and promote nighttime arousals. Traumatic experiences—especially those involving disordered eating or food insecurity—can resurface during sleep, manifesting as sleepwalking and eating. In clinical settings, individuals with post-traumatic stress disorder (PTSD) have been found to exhibit higher rates of sleep eating, suggesting a possible subconscious connection between unprocessed trauma and nighttime behavior. Addressing emotional trauma in therapy can be a transformative step toward healing SRED.
5. Are there any wearable devices or technologies that help detect sleep eating episodes? Yes, emerging technologies are making it easier to detect and monitor symptoms of sleep eating disorder at home. Wearable sleep trackers with motion sensors can capture unusual nighttime activity, especially when paired with smart home devices like kitchen cameras or fridge door sensors. Some advanced wearables even track sleep stages and can highlight patterns of frequent arousals that align with parasomnia behaviors. While these tools don’t replace professional diagnosis, they can provide valuable data for healthcare providers. Over time, tech-based monitoring may become a routine part of managing sleepwalking and eating disorders, especially for individuals living alone.
6. Can people with a sleep eating disorder engage in dangerous behaviors without knowing it? Yes, one of the most concerning aspects of a sleep eating disorder is the potential for harm during episodes. Because individuals are not fully conscious, they may use knives, ovens, or hot surfaces in ways that put them at significant risk. There are also documented cases of people consuming non-food items, expired products, or allergens without awareness, which can lead to poisoning or severe allergic reactions. The danger lies not only in the act of sleep eating itself but in the loss of judgment and motor coordination that accompanies partial wakefulness. This highlights the importance of safeguarding the environment for those diagnosed with SRED.
7. Does sleep eating disorder affect certain age groups more than others? Sleep eating can occur across all age groups, but it is most commonly observed in young to middle-aged adults. Adolescents experiencing hormonal changes or increased stress may also be vulnerable, particularly if there is a history of sleepwalking or anxiety. In older adults, sleep eating is less prevalent but may emerge due to neurodegenerative conditions, medication side effects, or chronic sleep disruptions. The age-related risk factors for sleep eating disorder also intersect with broader lifestyle changes—such as irregular work schedules, parenting stress, or retirement transitions. Tailoring treatment approaches based on age and life stage can improve outcomes significantly.
8. Are there any medications that unintentionally cause or worsen sleep eating behavior? Yes, several classes of medications have been linked to the onset or intensification of sleep eating episodes. Sedative-hypnotics like zolpidem, benzodiazepines, and certain antidepressants can alter brain chemistry in ways that increase the likelihood of parasomnias. These drugs affect neurotransmitters responsible for sleep regulation and inhibition control, sometimes lowering the threshold for sleepwalking and eating to occur. Additionally, over-the-counter sleep aids and even antihistamines may have similar effects in sensitive individuals. Anyone suspecting that their sleep eating disorder is medication-related should consult with their prescribing provider before making changes.
9. How can families support someone with a sleep related eating disorder? Family support plays a crucial role in the management of a sleep eating disorder. Loved ones can help by observing and documenting episodes, removing access to high-risk foods or sharp kitchen tools at night, and participating in behavioral interventions. Rather than framing the behavior as a choice or flaw, understanding that sleepwalking and eating are involuntary can foster empathy and reduce shame. Encouraging the individual to seek professional help and accompany them to appointments can also ease the treatment journey. By creating a supportive, nonjudgmental environment, families can help reduce stress and promote recovery.
10. What future advancements in sleep medicine might improve treatment for SRED? Advancements in neuroimaging, artificial intelligence, and wearable diagnostics are poised to revolutionize the understanding and treatment of SRED. Functional MRI studies are already uncovering how specific brain regions behave during parasomnia episodes, shedding light on the neural circuits involved in sleep eating disorder. AI-powered sleep analysis platforms may soon offer real-time insights and predictive alerts for parasomnia events, allowing individuals to intervene before a full episode unfolds. Personalized medicine—tailoring treatment based on genetic and neurobiological markers—could also pave the way for more effective and targeted therapies. As research evolves, the future holds promising tools to better manage and possibly prevent sleepwalking and eating behaviors.
Conclusion: Supporting Long-Term Wellness in the Face of Sleep Eating Disorder
Understanding a sleep eating disorder requires acknowledging its layered complexity, encompassing elements of neurology, psychology, nutrition, and lifestyle. While the experience of sleepwalking and eating may feel bewildering or distressing, it is a medically recognized condition that deserves attention and care. Raising awareness about this disorder helps remove stigma and promotes a more compassionate, evidence-based approach to treatment.
Addressing the root causes of a sleep related eating disorder involves more than managing symptoms—it calls for a holistic strategy that prioritizes sleep hygiene, mental health, mindful nutrition, and emotional well-being. Whether someone is navigating mild, occasional episodes or living with more chronic and disruptive patterns, a multidisciplinary treatment plan tailored to individual needs can make a meaningful difference.
As the conversation around sleep and health continues to evolve, recognizing the role of parasomnias like sleep eating becomes increasingly important. Not only does it bridge the gap between mind and body, but it also offers a roadmap for deeper self-understanding and healing. By approaching this disorder with curiosity, clinical insight, and practical support, individuals can reclaim their nights and move toward a more balanced, nourishing lifestyle.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Sleep-Related Eating Disorders

