Understanding the Emotional and Biological Roots of Binge Eating
Binge eating is not simply a matter of willpower or lack of self-control. It often stems from a complex interplay of emotional triggers, psychological conditions, and biological imbalances. For many individuals, the cycles of binge eating begin with emotional distress, often rooted in anxiety, depression, trauma, or chronic stress. Food, particularly highly palatable foods rich in sugar and fat, can serve as a temporary escape or comfort mechanism. This behavior becomes reinforced over time, leading to compulsive eating patterns that are hard to break without addressing the underlying issues.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
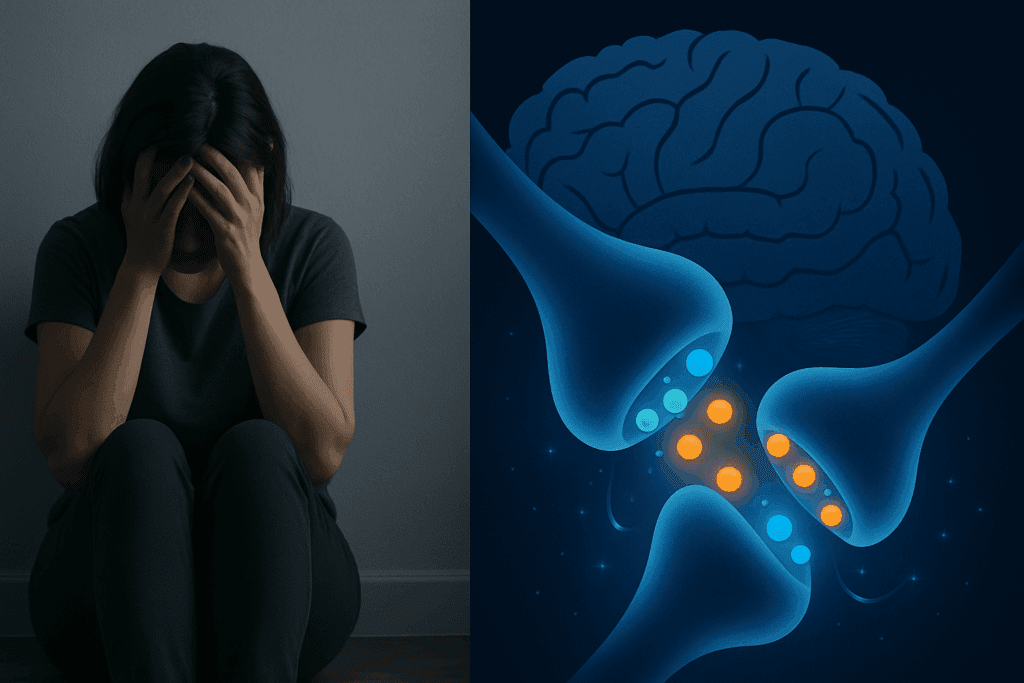
Biologically, binge eating disorder is influenced by neurochemical changes in the brain, including fluctuations in dopamine and serotonin. These neurotransmitters affect mood and reward, and imbalances can contribute to impulsive behavior and cravings. Understanding the definition for binge eating disorder involves recognizing that it is a medically recognized condition characterized by recurrent episodes of eating large quantities of food, often rapidly and to the point of discomfort, accompanied by feelings of loss of control and distress. Unlike bulimia nervosa, binge eating is not regularly followed by purging behaviors.
Additionally, environmental factors such as dieting, body dissatisfaction, and exposure to unrealistic beauty standards can exacerbate the risk. Many individuals who struggle with binge eating report a history of restrictive dieting, which sets the stage for binge-restrict cycles. These cycles of binge eating disorder are particularly harmful as they can entrench both physical and emotional patterns that reinforce the disorder. To disrupt these patterns, it is crucial to address both the emotional and physiological contributors with compassion, understanding, and evidence-based strategies.
The Role of Mindful Nutrition in Binge Eating Recovery
Mindful nutrition emphasizes awareness and presence during eating, focusing on the experience of food without judgment. This practice can help interrupt the automatic, often unconscious patterns associated with compulsive overeating. Instead of reacting to stress or emotional discomfort with food, mindful eating teaches individuals to tune into their physical hunger and fullness cues, which are often dulled by repeated binge behaviors. This reconnection to the body’s signals is essential in binge eating recovery.
Practicing mindful eating involves slowing down, chewing thoroughly, noticing the texture, taste, and aroma of food, and checking in with one’s emotional and physical state before, during, and after eating. It promotes a shift away from the guilt and shame that often accompany binge episodes and toward curiosity and self-compassion. This non-judgmental awareness allows for better recognition of triggers and patterns. For those who ask, “Why do I binge eat?” the answer often lies in unexamined emotional responses and unmet needs that surface during these mindful moments.
From a nutritional perspective, regular, balanced meals that include adequate protein, healthy fats, and fiber-rich carbohydrates can stabilize blood sugar levels and reduce the intensity of cravings. In contrast, long periods of fasting or restrictive eating can increase vulnerability to binging. Mindful nutrition strategies can therefore help to break the cycles of binge eating by preventing extreme hunger and promoting consistent energy levels. Incorporating these principles into daily life fosters a sustainable approach to eating that supports both physical and emotional wellbeing.

Recognizing the Signs of Compulsive Overeating
To effectively address compulsive eating, it is important to first recognize the behavioral, emotional, and physical signs that indicate the presence of a problem. Compulsive overeating is characterized by a persistent urge to eat large quantities of food, often when not physically hungry. It is frequently accompanied by feelings of guilt, shame, and distress. Individuals may find themselves thinking, “I can’t stop eating,” despite a desire to change.
Episodes of compulsive eating often involve secrecy, such as hiding food or eating alone to avoid judgment. These behaviors can escalate over time, resulting in health consequences such as weight gain, gastrointestinal discomfort, and an increased risk for chronic illnesses like type 2 diabetes and heart disease. More subtly, compulsive overeating can erode self-esteem and contribute to feelings of isolation and hopelessness.
Compulsive overeating is one of several compulsive eating disorders that can profoundly impact quality of life. Understanding its characteristics allows individuals and healthcare providers to intervene early and effectively. Acknowledging the issue without judgment is the first step toward healing. Asking questions like, “Do I have binge eating disorder?” or “How severe is my binge eating disorder?” can lead to professional assessments and targeted interventions.
The Psychological Triggers Behind Binging
One of the most common questions from those experiencing binge eating is, “Why do I binge?” The answer often lies in psychological triggers that create a cascade of emotional responses leading to overeating. Common triggers include stress, loneliness, boredom, anxiety, and unresolved trauma. Food becomes a coping mechanism, temporarily numbing emotional pain or providing a sense of control in an otherwise chaotic internal world.
Cognitive distortions, such as all-or-nothing thinking, can also contribute to the binge-restrict cycle. For example, a person might perceive a single indulgent food choice as a total failure, prompting a “might as well binge” mentality. This thinking reinforces the cycles of binge eating and perpetuates feelings of failure and hopelessness. Addressing these distorted beliefs is an essential component of recovery.
Therapeutic approaches such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and mindfulness-based interventions have been shown to be effective in treating binge eating disorder. These therapies help individuals identify emotional and cognitive triggers, develop healthier coping strategies, and build resilience. Through this process, people learn how to overcome binge eating by responding to emotional discomfort with self-awareness rather than food.
Exploring Medical Treatment Options
In some cases, medical intervention is necessary to support recovery. Binge eating disorder medication can play a role in regulating mood, reducing impulsivity, and diminishing cravings. Certain antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), have been prescribed to help manage the symptoms of binge eating. These medications influence brain chemistry and can offer relief for those struggling with the emotional intensity that often underlies compulsive eating.
More recently, medications such as lisdexamfetamine (Vyvanse) have received FDA approval specifically for the treatment of moderate to severe binge eating disorder. These drugs for binge eating work by altering neurotransmitter activity related to reward and impulse control. However, like all medications, they carry potential side effects and should be prescribed and monitored by a qualified healthcare provider.
Some individuals may also explore off-label options or other meds for binge eating disorder in conjunction with psychotherapy. It is essential to have a comprehensive treatment plan that includes medical, psychological, and nutritional components. Understanding how to get over binge eating may involve trying different strategies under medical supervision. Medication alone is rarely a complete solution, but it can provide the necessary support for individuals who feel overwhelmed or stuck.
Developing Sustainable Strategies to Stop Nighttime Binge Eating
Nighttime binge eating is a common manifestation of binge eating disorder and can be particularly distressing. Individuals often report feeling in control during the day, only to experience intense cravings and compulsive eating behaviors after dark. This pattern can be fueled by physical hunger due to inadequate daytime nutrition, emotional fatigue, or a desire to self-soothe before sleep.
Understanding how to stop binge eating at night requires a holistic approach. First, it is important to ensure that meals and snacks are evenly distributed throughout the day to prevent extreme hunger. Skipping meals or eating very little during the day can increase the likelihood of nighttime binging. Additionally, developing evening routines that promote relaxation and reduce stress can lessen the urge to eat as a coping mechanism.
Psychological tools such as keeping a food and emotion journal, practicing guided meditation, or engaging in light physical activity can help redirect the impulse to binge. Individuals may benefit from exploring the deeper emotional reasons behind nighttime eating, which can often reflect unresolved feelings or unmet needs. Learning how to stop nighttime binge eating is not just about managing behavior but also about nurturing emotional well-being in the hours before sleep.
Using Diagnostic Tools and Self-Assessments
If you find yourself repeatedly asking, “How can I stop binging?” or “Why can’t I stop eating?” it may be time to seek a formal diagnosis. A binge eating disorder test, administered by a licensed professional, can help assess the severity of symptoms and determine the most appropriate course of action. These evaluations typically include questions about eating patterns, emotional responses to food, and the frequency and intensity of binge episodes.
Self-assessment tools can also be helpful for those unsure whether they meet the clinical criteria. While these tools are not a substitute for professional evaluation, they can prompt important conversations and motivate individuals to seek help. Honest reflection is essential during this process. Understanding the nuances of compulsive overeating versus other types of disordered eating is critical for accurate diagnosis and effective treatment.
Healthcare providers may also use blood tests, physical examinations, and psychological screenings to evaluate the impact of binge eating on overall health. Because the cycles of binge eating can lead to metabolic disturbances, early detection and treatment can prevent long-term complications. Whether you’re considering medication for binge eating or exploring therapy options, a thorough diagnosis ensures your treatment plan is tailored to your needs.
Embracing a Holistic Approach to Recovery
Recovery from binge eating disorder requires a multifaceted approach that addresses body, mind, and spirit. While medication and therapy are important tools, lifestyle interventions such as sleep hygiene, regular physical activity, and stress management practices also play a significant role. Learning how to overcome binge behaviors means looking beyond food and identifying areas of life where self-care and balance are lacking.
Yoga, meditation, and journaling are examples of holistic practices that can help individuals connect with their emotions and reduce anxiety. These tools foster greater self-awareness, which is essential for breaking the automatic patterns associated with compulsive eating. Social support from friends, family, or peer groups also contributes to sustained recovery. Sharing your journey with others who understand can reduce shame and foster accountability.
Importantly, recovery is not a linear process. There may be setbacks along the way, and that’s okay. Each step forward, no matter how small, is progress. Learning how to control binge eating involves patience, consistency, and self-compassion. As individuals begin to reframe their relationship with food and emotions, they build a foundation for lasting change.

How to Cultivate Self-Compassion and Resilience
Self-compassion is a powerful antidote to the shame and guilt that often accompany binge eating disorder. Instead of viewing setbacks as failures, self-compassion encourages a kinder, more understanding inner dialogue. This shift in perspective can reduce the intensity of emotional triggers and provide a more stable foundation for long-term recovery.
Cultivating resilience involves developing coping strategies for stress, emotional upheaval, and life transitions. It means recognizing that everyone struggles and that imperfection is part of the human experience. Through resilience, individuals can bounce back from relapses with renewed determination rather than despair. These qualities are not innate but can be nurtured over time through intentional practice and support.
Affirmations, therapy, and mindfulness exercises can help reinforce a positive sense of self. Engaging in activities that bring joy, creativity, or connection can also replenish emotional reserves and reduce the likelihood of turning to food for comfort. As individuals build emotional strength and self-worth, they become better equipped to overcome the cycles of binge eating and maintain their recovery.

Reclaiming Your Relationship with Food and Body
At the heart of binge eating recovery lies the need to heal one’s relationship with food and the body. Years of dieting, restriction, and shame can erode trust in one’s internal cues and create a deeply adversarial connection with food. Rebuilding this trust is essential for lasting change.
This process begins with rejecting diet culture and embracing a more intuitive approach to eating. Intuitive eating encourages individuals to honor hunger and fullness, respect body signals, and find satisfaction in food without guilt. It promotes a sense of agency and reconnects people with their natural rhythms and needs. Over time, this approach can help break the cycles of binge eating and foster a more peaceful, nourishing experience with food.
Body image work is another crucial element. Accepting and appreciating the body as it is—regardless of size or shape—can reduce the emotional distress that often fuels disordered eating. This does not mean giving up on health but rather pursuing health from a place of care and respect rather than punishment. As individuals learn to relate to their bodies with compassion, the urge to engage in compulsive eating behaviors often diminishes.
Frequently Asked Questions: How to Stop Binge Eating and Break the Cycles of Compulsive Overeating
1. What are some unexpected psychological factors that contribute to the cycles of binge eating?
While emotional distress and trauma are well-known triggers, lesser-known psychological factors also influence the cycles of binge eating. These may include perfectionism, fear of failure, and chronic low self-worth, which can silently fuel the urge to overeat. People with high-achieving tendencies might binge in private as a way to rebel against their own inner pressure to appear in control. Additionally, microtraumas—such as persistent social rejection or body-shaming comments over time—can accumulate and result in compulsive eating behaviors. Addressing these subtle but significant influences is critical when exploring how to stop binge eating in a holistic and lasting way.
2. Can medication for binge eating be used long term, and are there alternatives for those who don’t respond well to them?
Binge eating disorder medication can be used long term in certain cases, but long-term use should always be monitored closely by a healthcare provider. Some individuals find success with drugs for binge eating such as lisdexamfetamine, which has shown promise in reducing frequency and severity of binges. However, not all individuals tolerate these meds for binge eating disorder well, and side effects like insomnia or irritability can arise. For those seeking non-pharmaceutical alternatives, approaches such as neurofeedback, somatic therapies, and targeted nutritional supplementation may support binge eating recovery. These methods can help retrain brain patterns and restore physiological balance without relying solely on medication.
3. Why do I binge eat even when I’m not hungry, and what can I do about it?
The question “Why do I binge eat when I’m not physically hungry?” often points to emotional or symbolic hunger. Food can become a stand-in for unmet emotional needs such as connection, validation, or security. In such cases, the solution is not only learning how to control binge eating, but also learning how to meet emotional needs directly. Techniques such as emotional mapping or working with a somatic therapist can help uncover what food represents in these moments. Understanding and meeting these deeper needs is key when learning how to overcome binge eating for good.
4. How can I stop nighttime binge eating when cravings feel strongest before bed?
Nighttime is often when emotional defenses are low, making it harder to resist urges, especially if the day was stressful or undernourished. Learning how to stop binge eating at night involves identifying the specific emotional cues and physiological patterns that spike after dark. For example, people often confuse exhaustion with hunger or use food as a reward after a long day. One effective strategy is front-loading nutrition by eating balanced, satisfying meals earlier in the day to reduce evening cravings. In addition, creating a structured bedtime routine that includes journaling, meditation, or herbal tea can reduce the emotional urgency that drives how to stop nighttime binge eating.
5. What is the difference between compulsive overeating and other compulsive eating disorders?
To describe compulsive eating disorders accurately, it’s important to understand the distinctions between them. Compulsive overeating generally involves persistent eating past the point of fullness without necessarily meeting the diagnostic criteria for binge eating disorder. In contrast, binge eating disorder includes episodes of consuming unusually large quantities of food with a sense of loss of control and significant emotional distress. Other compulsive eating disorders may involve ritualistic eating patterns, obsessive food rules, or co-occurring behaviors like purging. Understanding these nuances helps individuals assess how severe is my binge eating disorder and what tailored treatment options might work best.
6. How do I build long-term habits that help me get over binge eating for good?
Learning how to get over binge eating isn’t just about avoiding trigger foods—it requires restructuring how you relate to stress, emotion, and nourishment. Habit stacking, where you link a new recovery-oriented behavior with an existing one (like doing a breathing exercise before meals), can make new routines more sustainable. Identifying personal cues that signal the start of the cycles of binge eating allows you to proactively intervene before a binge escalates. Working with a nutritionist can also help ensure that meals support stable blood sugar, which reduces physiological triggers. Most importantly, focusing on long-term consistency over short-term perfection is key in binge eating disorder recovery.
7. What should I do if I keep thinking, “I can’t stop eating” even when I’m full?
When the thought “I can’t stop eating” arises repeatedly, it’s a signal that internal coping mechanisms may be overwhelmed. This may relate to the brain’s reward system being dysregulated, especially in those who have experienced trauma or chronic stress. Practices like polyvagal exercises, which calm the nervous system, can help reduce the urgency that drives compulsive eating. Addressing this thought pattern with curiosity, rather than judgment, opens the door to deeper healing and more compassionate self-dialogue. Consulting a therapist can also provide clarity on how to overcome binge tendencies by examining the psychological roots behind persistent overeating.
8. Are there new or emerging therapies that help stop binging more effectively?
Recent developments in mental health care offer new pathways for those wondering how to stop binging. Acceptance and Commitment Therapy (ACT), which helps individuals commit to values-based living despite difficult emotions, shows promise in helping people step away from compulsive patterns. EMDR (Eye Movement Desensitization and Reprocessing) is being used with success for individuals whose cycles of binge eating are tied to trauma. There’s also growing interest in psychedelics-assisted therapy (in clinical settings) to help reset ingrained patterns and improve emotional flexibility. While not yet mainstream, these approaches may revolutionize how to stop compulsive eating and support holistic recovery.
9. How can I assess whether I need professional help for binge eating disorder?
Asking “Do I have binge eating disorder?” is an important step, and a binge eating disorder test can provide helpful clarity. These assessments often examine emotional distress, frequency of binge episodes, and physical symptoms like rapid weight fluctuations. If you find that the cycles of binge eating disorder are interfering with your quality of life, relationships, or physical health, professional help is strongly recommended. Clinical psychologists, dietitians, and psychiatrists trained in eating disorders can guide you through diagnosis and treatment. Taking this step can be a turning point in how to overcome binge eating and develop a personalized recovery plan.
10. What role does body image play in binge eating, and how can I improve it?
Poor body image often serves as both a trigger and a consequence of binge eating behaviors. When individuals internalize negative beliefs about their appearance, it can lead to restrictive dieting and emotional shame, which are precursors to the urge to binge. Reframing body image through practices like body neutrality, self-compassion meditation, or mirror work can interrupt the compulsive eating cycle. This shift helps reduce the emotional burden that perpetuates the thought, “How can I stop binging if I hate my body?” Learning to view the body as a vehicle for life rather than a project to fix can dramatically improve self-worth and support binge eating disorder recovery.
Conclusion: Moving Forward with Awareness and Hope
Breaking free from binge eating and compulsive overeating is a courageous and deeply personal journey. It involves unraveling long-held beliefs, confronting emotional pain, and cultivating new habits that support healing and self-respect. For those who wonder, “How can I stop binging?” or struggle with feelings of, “I can’t stop eating,” know that recovery is possible with the right support and strategies.
By addressing both the psychological and physiological roots of binge eating disorder, embracing mindful nutrition, and exploring tools such as therapy and medication for binge eating, individuals can begin to shift their relationship with food and themselves. Whether through medical support like binge eating disorder medication, lifestyle adjustments, or therapeutic practices, there are many pathways to recovery.
Understanding how to stop compulsive eating requires commitment, but it also opens the door to deeper self-understanding and resilience. With patience and compassion, it’s possible to end the cycles of binge eating and reclaim a sense of peace and empowerment. As this journey unfolds, the emphasis should always remain on nourishment, self-care, and a return to wholeness—one mindful step at a time.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.