High cholesterol and fatty liver disease are two increasingly common health concerns that affect millions of people worldwide. While they may appear to be separate conditions, scientific research suggests a strong connection between them. Understanding this link can help individuals take proactive steps toward better health, reducing their risk of complications such as cardiovascular disease and liver damage. This article explores the relationship between high cholesterol and fatty liver, the underlying causes, and effective strategies for prevention and treatment.
You may also like: The Best Liver Detox Supplements: How to Choose Safe and Effective Support for Your Liver
Understanding High Cholesterol and Fatty Liver Disease
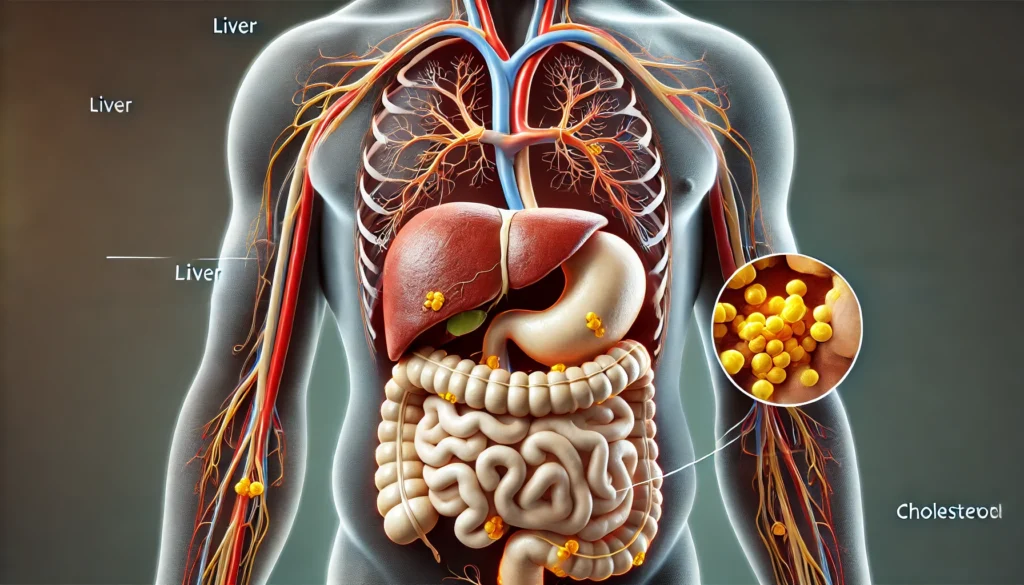
Cholesterol is a fatty substance essential for many bodily functions, including hormone production, cell membrane integrity, and bile acid formation. However, when cholesterol levels become too high, particularly low-density lipoprotein (LDL) cholesterol, it can lead to plaque buildup in the arteries, increasing the risk of heart disease. On the other hand, fatty liver disease occurs when excess fat accumulates in liver cells, impairing liver function and potentially leading to inflammation, fibrosis, or even cirrhosis.
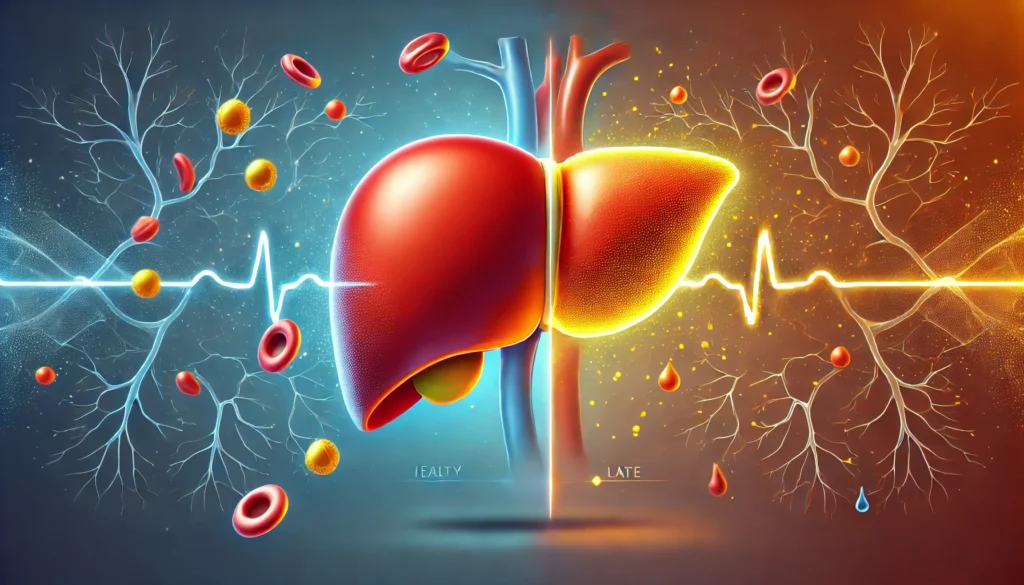
Fatty liver disease can be categorized into two primary types: non-alcoholic fatty liver disease (NAFLD) and alcoholic fatty liver disease (AFLD). NAFLD is closely linked to metabolic syndrome, obesity, type 2 diabetes, and high cholesterol levels. AFLD results from excessive alcohol consumption, which disrupts fat metabolism in the liver. While both forms can progress to severe liver damage, NAFLD has emerged as the most prevalent liver disorder in developed countries, often occurring alongside high cholesterol and other metabolic abnormalities.
Can Fatty Liver Cause High Cholesterol?
One of the most critical questions regarding the connection between fatty liver and cholesterol is whether fatty liver disease can directly contribute to high cholesterol levels. Research suggests that the liver plays a central role in cholesterol metabolism. When the liver accumulates excessive fat, its ability to regulate cholesterol production and clearance becomes impaired. As a result, individuals with fatty liver disease often experience elevated cholesterol and triglyceride levels, further exacerbating their risk of cardiovascular disease.
Additionally, fatty liver disease can alter the composition of lipoproteins in the blood, increasing the prevalence of small, dense LDL particles, which are more likely to contribute to arterial plaque formation. This shift in lipid profile makes it even more critical for individuals with fatty liver disease to manage their cholesterol levels effectively.
The Metabolic Connection Between High Cholesterol and Fatty Liver Disease
Metabolic dysfunction is a significant factor linking high cholesterol and fatty liver disease. Insulin resistance, a hallmark of metabolic syndrome, plays a key role in both conditions. When cells become resistant to insulin, the pancreas compensates by producing more insulin, leading to higher circulating levels of this hormone. Elevated insulin promotes fat storage in the liver, contributing to fatty liver disease, while also increasing LDL cholesterol and triglyceride production.
Moreover, chronic inflammation, often associated with obesity and metabolic syndrome, exacerbates both high cholesterol and fatty liver disease. Inflammatory markers such as C-reactive protein (CRP) and cytokines disrupt normal lipid metabolism and impair the liver’s ability to process fats efficiently. This inflammatory response can further accelerate the progression of fatty liver disease and increase the likelihood of developing cardiovascular complications.
How Diet Impacts High Cholesterol and Fatty Liver Disease
Diet plays a pivotal role in the development and management of both high cholesterol and fatty liver disease. Consuming a diet high in refined carbohydrates, saturated fats, and trans fats contributes to liver fat accumulation and dyslipidemia. Processed foods, sugary beverages, and excessive alcohol intake further strain liver function and promote lipid imbalances.
Conversely, adopting a nutrient-dense diet rich in whole foods can significantly improve liver health and cholesterol levels. The Mediterranean diet, for example, emphasizes healthy fats such as olive oil, nuts, and fatty fish, which support lipid metabolism and reduce inflammation. Fiber-rich foods like vegetables, legumes, and whole grains help regulate cholesterol absorption in the intestines, lowering LDL cholesterol and promoting overall metabolic health.
Lifestyle Modifications to Improve Liver Health and Cholesterol Levels
In addition to dietary changes, adopting a physically active lifestyle can have profound benefits for individuals struggling with high cholesterol and fatty liver disease. Regular exercise enhances insulin sensitivity, reduces liver fat, and promotes the breakdown of harmful lipids in the bloodstream. Both aerobic activities, such as brisk walking and cycling, and resistance training contribute to improved metabolic health.
Weight management is another crucial aspect of addressing these conditions. Losing even a small percentage of body weight—typically around 5-10%—can lead to significant reductions in liver fat content and improvements in cholesterol levels. Combining calorie control with nutrient-dense meals and physical activity creates a sustainable approach to long-term health improvement.
Medical Interventions for Managing High Cholesterol and Fatty Liver Disease
For individuals with severe cases of high cholesterol and fatty liver disease, medical interventions may be necessary. Statins, commonly prescribed to lower LDL cholesterol, have also shown potential benefits for individuals with NAFLD by reducing liver inflammation and preventing disease progression. However, not all patients with fatty liver disease can tolerate statins, necessitating alternative lipid-lowering therapies such as fibrates, niacin, and omega-3 fatty acids.
In cases where fatty liver disease has progressed to non-alcoholic steatohepatitis (NASH) or cirrhosis, additional medical treatments may be required. Emerging therapies, including medications targeting liver fat metabolism and inflammation, offer hope for individuals with advanced liver disease. However, early intervention through lifestyle modifications remains the most effective strategy for preventing disease progression.
The Importance of Regular Health Screenings
Routine health screenings are essential for detecting high cholesterol and fatty liver disease in their early stages. Blood tests measuring lipid levels, liver enzymes, and markers of inflammation provide valuable insights into an individual’s metabolic health. Imaging techniques such as ultrasound, elastography, and MRI can assess liver fat accumulation and fibrosis, guiding treatment decisions.
Individuals with risk factors such as obesity, diabetes, or a family history of cardiovascular disease should prioritize regular check-ups with their healthcare providers. Early detection allows for timely interventions, reducing the risk of complications and improving long-term health outcomes.
Frequently Asked Questions (FAQ) on High Cholesterol and Fatty Liver Disease
1. How are high cholesterol and fatty liver disease connected?
High cholesterol and fatty liver disease are closely linked because both conditions are influenced by poor metabolic health. When the liver becomes fatty, it struggles to process lipids efficiently, often leading to an increase in LDL cholesterol and triglycerides in the bloodstream. This can contribute to plaque buildup in arteries, raising the risk of cardiovascular diseases. Additionally, insulin resistance—a common factor in metabolic syndrome—can worsen both high cholesterol and fatty liver disease. Addressing these conditions through diet, lifestyle changes, and medical interventions is key to improving overall health.
2. Can fatty liver cause high cholesterol, or is it the other way around?
Fatty liver can cause high cholesterol by impairing the liver’s ability to regulate lipid metabolism. When excess fat accumulates in liver cells, it disrupts the normal breakdown and distribution of cholesterol, leading to elevated blood levels of LDL (bad cholesterol) and triglycerides. Conversely, high cholesterol—especially when driven by poor diet and lifestyle choices—can contribute to the development of fatty liver disease. The relationship is bidirectional, meaning that managing one condition often helps improve the other.
3. What dietary changes help manage high cholesterol and fatty liver disease?
A diet rich in fiber, healthy fats, and lean proteins can significantly improve high cholesterol and fatty liver disease. Incorporating foods like leafy greens, avocados, nuts, and fatty fish can help reduce LDL cholesterol and support liver function. Processed foods, refined carbohydrates, and trans fats should be minimized, as they contribute to inflammation and fat accumulation in the liver. Additionally, increasing water intake and consuming antioxidant-rich foods, such as berries and green tea, can further aid in liver detoxification and cholesterol balance.
4. How does exercise impact high cholesterol and fatty liver disease?
Regular physical activity plays a crucial role in managing both high cholesterol and fatty liver disease. Exercise helps improve insulin sensitivity, which in turn reduces fat accumulation in the liver and promotes better cholesterol metabolism. Aerobic exercises like walking, cycling, and swimming, combined with resistance training, can increase HDL (good cholesterol) and lower triglycerides. Engaging in at least 150 minutes of moderate-intensity exercise per week can yield noticeable improvements in metabolic health.
5. Are there specific supplements that can support liver health and cholesterol levels?
Certain supplements may help manage high cholesterol and fatty liver disease. Omega-3 fatty acids, found in fish oil, can lower triglycerides and reduce liver fat. Milk thistle has been studied for its potential to protect liver cells and improve detoxification. Niacin (vitamin B3) can raise HDL cholesterol and reduce LDL levels. However, it’s important to consult with a healthcare professional before starting any supplement regimen, as individual responses and potential interactions with medications should be considered.
6. Can weight loss alone reverse fatty liver and improve cholesterol levels?
Yes, weight loss is one of the most effective ways to improve both fatty liver disease and high cholesterol. Losing just 5-10% of body weight can lead to significant reductions in liver fat, improved cholesterol levels, and enhanced insulin sensitivity. Sustainable weight loss strategies, such as adopting a Mediterranean or plant-based diet and incorporating regular physical activity, are recommended over crash diets, which can strain the liver.
7. How does alcohol consumption affect high cholesterol and fatty liver disease?
Excessive alcohol intake can worsen both high cholesterol and fatty liver disease by increasing fat accumulation in liver cells and disrupting lipid metabolism. Alcohol-related liver disease can develop alongside non-alcoholic fatty liver disease (NAFLD), further exacerbating liver damage. Moderate alcohol consumption—such as one drink per day for women and two for men—may be permissible for some individuals, but those with advanced fatty liver disease should consider abstaining entirely.
8. What are the long-term risks of untreated high cholesterol and fatty liver disease?
If left unmanaged, high cholesterol and fatty liver disease can lead to severe health complications. Fatty liver disease may progress to non-alcoholic steatohepatitis (NASH), cirrhosis, or liver cancer. High cholesterol increases the risk of heart disease, stroke, and atherosclerosis. Because these conditions are often silent in the early stages, regular medical check-ups and proactive lifestyle changes are essential for preventing long-term damage.
9. Are there genetic factors that influence the risk of high cholesterol and fatty liver disease?
Genetics can play a significant role in both high cholesterol and fatty liver disease. Some individuals have a genetic predisposition to higher LDL cholesterol levels or metabolic disorders that increase the likelihood of liver fat accumulation. Familial hypercholesterolemia is an inherited condition that leads to dangerously high cholesterol levels at an early age. While genetics cannot be changed, lifestyle interventions can significantly mitigate their impact.
10. Can medications help treat high cholesterol and fatty liver disease?
Yes, medications are sometimes necessary to manage high cholesterol and fatty liver disease, especially if lifestyle changes alone are insufficient. Statins are commonly prescribed to lower cholesterol levels and may also have protective effects on the liver. Other medications, such as fibrates and PCSK9 inhibitors, can help regulate lipid levels. Emerging treatments for fatty liver disease, including GLP-1 receptor agonists, are being explored for their potential to reduce liver fat. Always consult a healthcare provider before starting any medication regimen to determine the best course of action for your specific condition.
Conclusion: Taking a Proactive Approach to Health
Understanding the intricate connection between high cholesterol and fatty liver disease empowers individuals to take control of their health. By adopting a balanced diet, engaging in regular physical activity, and undergoing routine health screenings, individuals can mitigate their risk of developing severe metabolic complications. Proactive lifestyle changes, combined with medical interventions when necessary, offer a pathway to improved liver function, optimal cholesterol levels, and overall well-being.
healthy liver function, cholesterol management, metabolic health, NAFLD prevention, diet for liver health, lowering LDL cholesterol, insulin resistance and fatty liver, heart disease risk factors, non-alcoholic fatty liver disease treatment, exercise for metabolic syndrome, triglycerides and liver health, weight loss and liver fat reduction, inflammation and cholesterol levels, best foods for liver detox, liver enzyme improvement, cardiovascular disease prevention, fiber and cholesterol reduction, medical treatments for fatty liver, importance of omega-3 for heart and liver, lifestyle changes for cholesterol and liver health
Further Reading:
Recent insights on the role of cholesterol in non-alcoholic fatty liver disease
How are liver function and cholesterol production linked?
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.