The liver is one of the most vital organs in the human body, playing a critical role in detoxification, metabolism, and overall health. With increasing awareness about liver-related diseases, many individuals seek liver health supplements to support optimal function. Two popular options in this category are Liver Health Formula and Liver Renew Formula. This article examines the effectiveness of these supplements, the scientific basis behind their ingredients, and their potential role in maintaining liver function.
You may also like: The Best Liver Detox Supplements: How to Choose Safe and Effective Support for Your Liver
Understanding Liver Function and the Need for Supplements
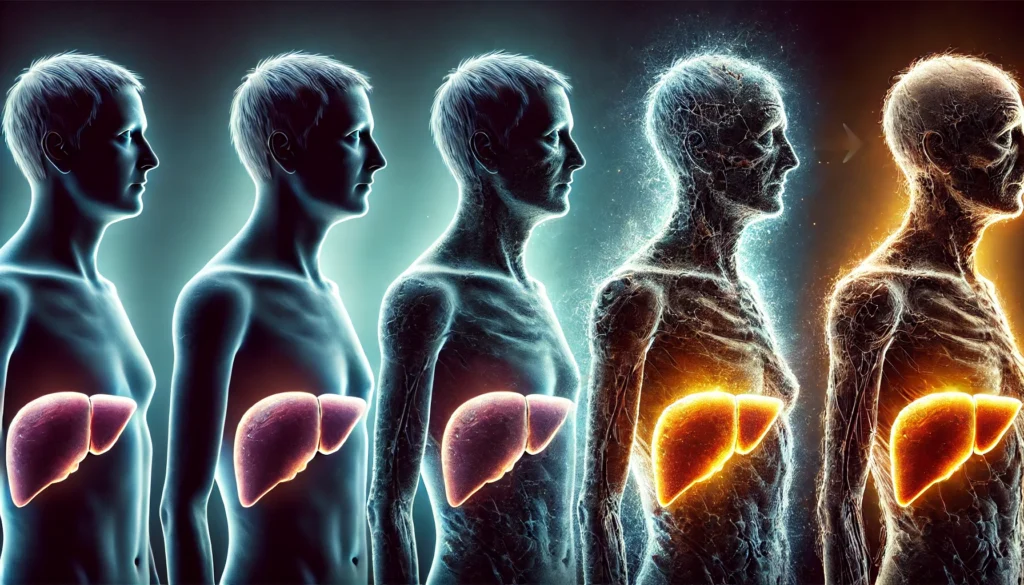
The liver is responsible for filtering toxins from the blood, producing bile for digestion, and regulating essential metabolic processes. A healthy liver supports overall well-being, but factors such as poor diet, excessive alcohol consumption, and exposure to environmental toxins can compromise its function. Over time, liver damage can lead to severe conditions, including liver cirrhosis, end-stage liver disease, and acute liver failure. Understanding the importance of liver health has led to the rise in liver supplements aimed at promoting detoxification and regeneration.
Liver health supplements often contain a blend of natural ingredients, including herbal extracts, antioxidants, and amino acids, purported to support liver function. Some ingredients, such as milk thistle, have long been used in traditional medicine for liver protection. However, the question remains: How effective are these supplements in preventing or managing liver disease?
Examining Liver Health Formula: Ingredients and Benefits
Liver Health Formula is a widely recognized liver supplement marketed as a solution for detoxification, liver repair, and improved overall health. The formula comprises a mix of herbal extracts, vitamins, and minerals believed to enhance liver function. Some of the key ingredients include milk thistle extract, dandelion root, turmeric, and N-acetyl cysteine (NAC). These components have been studied for their potential hepatoprotective properties.
Milk thistle, one of the most researched liver-protecting herbs, contains silymarin, a compound known for its antioxidant and anti-inflammatory properties. Studies suggest that silymarin can help protect liver cells from oxidative stress and promote regeneration. Similarly, turmeric contains curcumin, a powerful anti-inflammatory agent that may support liver detoxification. Dandelion root is believed to aid digestion and support bile production, which is essential for breaking down fats and eliminating toxins. NAC, a precursor to glutathione, is a crucial antioxidant that helps neutralize harmful free radicals.
While these ingredients have demonstrated potential liver benefits, it is essential to consider the dosage and formulation. Scientific evidence supports the hepatoprotective effects of milk thistle and NAC, but the effectiveness of other components varies. Additionally, individual responses to liver supplements differ, and some users may experience significant benefits while others notice minimal effects.
Liver Renew Formula: A Closer Look at Its Composition and Claims
Liver Renew Formula is another supplement marketed as a solution for enhancing liver health. This formula contains a combination of traditional herbal remedies and modern compounds, including artichoke extract, beetroot powder, alpha-lipoic acid, and zinc. Each ingredient is selected for its purported ability to support liver detoxification and cellular repair.
Artichoke extract has been traditionally used to support liver function by stimulating bile production and promoting digestion. Beetroot is a natural source of betaine, which may help reduce fatty deposits in the liver. Alpha-lipoic acid, a potent antioxidant, is known for its role in regenerating glutathione and protecting liver cells from oxidative damage. Zinc, an essential mineral, plays a role in liver enzyme function and immune system support.
Although these ingredients hold promise, their effectiveness depends on various factors, including the severity of liver damage, lifestyle choices, and individual health conditions. Clinical studies on these specific combinations are limited, and while the individual ingredients have shown positive effects, more research is needed to establish their efficacy in supplement form.
Do Liver Health Supplements Prevent Liver Disease?
One of the primary reasons individuals turn to liver supplements is the hope of preventing liver disease. Conditions such as non-alcoholic fatty liver disease (NAFLD), liver fibrosis, and cirrhosis are often linked to poor dietary habits, sedentary lifestyles, and excessive alcohol consumption. While liver health supplements may provide supportive benefits, they should not be considered a replacement for a healthy lifestyle.
The effectiveness of liver supplements in preventing liver disease largely depends on their ability to reduce inflammation, combat oxidative stress, and support detoxification pathways. Ingredients such as milk thistle, turmeric, and alpha-lipoic acid have demonstrated potential benefits in reducing liver inflammation and promoting cell repair. However, these supplements should be used in conjunction with a balanced diet, regular exercise, and reduced alcohol intake for optimal liver health.
Are Liver Health Supplements Safe for Everyone?
Safety is a crucial consideration when evaluating liver health supplements. While many ingredients in these formulas are derived from natural sources, they can still interact with medications or cause adverse effects in certain individuals. For example, milk thistle may interact with medications that affect the liver’s enzyme system, potentially altering drug metabolism. Turmeric, when consumed in high doses, can cause gastrointestinal discomfort or interfere with blood-thinning medications.
Additionally, individuals with pre-existing liver conditions should consult a healthcare professional before using liver supplements. While some compounds may support liver function, others could exacerbate existing conditions. It is also important to note that dietary supplements are not regulated as strictly as pharmaceutical drugs, meaning product quality and ingredient concentrations can vary between brands.
Frequently Asked Questions (FAQ) on End-Stage Liver Disease and Liver Failure
1. What are the key symptoms in the final stages of liver failure? The liver disease final stages symptoms can vary but generally include severe jaundice, confusion due to toxin buildup (hepatic encephalopathy), ascites (fluid buildup in the abdomen), extreme fatigue, and significant weight loss. Patients often experience gastrointestinal bleeding as liver function deteriorates. The immune system becomes severely compromised, making infections more frequent. Eventually, organ failure leads to a coma-like state before death. Recognizing these symptoms early may allow for palliative care interventions to improve comfort.
2. How long does the liver failure death timeline typically last? The liver failure death timeline depends on several factors, including the underlying cause, overall health, and medical intervention. Acute liver failure death timeline cases can progress within days to weeks, whereas chronic liver disease may take months or even years to reach the terminal phase. End-stage liver failure timeline cases often follow a predictable decline, with worsening complications leading to multi-organ failure. A liver cirrhosis death timeline can range from weeks to months, depending on the severity and management of complications. Early detection and medical support can sometimes slow progression, but in advanced cases, timeframes are often unpredictable.
3. What are the last stages of liver failure before death? In the last stages of liver failure before death, patients typically experience profound mental confusion, extreme weakness, and an inability to eat or drink. The liver can no longer detoxify the blood, leading to severe metabolic imbalances. Multiple organ failure often follows, with kidney dysfunction (hepatorenal syndrome) and respiratory failure being common. Ascites and internal bleeding may worsen, necessitating hospitalization for symptom management. Hospice or palliative care becomes critical in ensuring comfort as the body shuts down.
4. What percentage of liver damage is dangerous? Liver function is remarkably resilient, but damage exceeding 75-80% is typically life-threatening. What percentage of liver damage is dangerous depends on whether the liver can still regenerate and function despite injury. Chronic conditions like cirrhosis impair the liver’s ability to repair itself, increasing the risk of liver failure. In cases of acute liver failure, rapid destruction of 50% or more of the liver can lead to immediate organ shutdown. Advanced fibrosis and cirrhosis significantly increase mortality risk, particularly when complications arise.
5. How many stages of cirrhosis are there, and what do they mean? When asking how many stages of cirrhosis are there, most medical professionals classify cirrhosis into four stages. Stage 1 involves mild fibrosis with no significant symptoms. Stage 2 sees increasing scarring but still manageable function. Stage 3 represents advanced fibrosis with portal hypertension and noticeable complications. Finally, stage 4 is decompensated cirrhosis, characterized by liver failure, severe complications, and a high risk of death. Understanding these stages helps determine the best treatment approach.
6. What are the final symptoms of end-stage liver disease? The final symptoms of end-stage liver disease include profound weakness, confusion, unresponsiveness, and severe fluid retention. Jaundice becomes extreme, and many patients develop significant itching due to bile salt buildup. Bleeding complications, including gastrointestinal hemorrhage, are common. Hepatic encephalopathy may progress to coma. Death often follows multi-organ failure, requiring close medical management to ensure comfort.
7. How does the end-stage liver disease death process typically unfold? The end-stage liver disease death process varies by individual but generally involves progressive decline. The body struggles to remove toxins, causing confusion and coma. Fluid overload leads to difficulty breathing and infection risks. Organ function deteriorates until the heart and lungs cease to function. Pain and discomfort can be managed through palliative care, helping families navigate this difficult period.
8. How can caregivers support someone in the final stages of liver failure? Caregivers play a crucial role in ensuring comfort and dignity in the end stages of liver failure. Providing emotional support, assisting with symptom management, and coordinating with healthcare providers are essential. Ensuring hydration, preventing bedsores, and managing medications can improve quality of life. Hospice care can provide specialized support tailored to end-stage needs. Open discussions about care preferences can help families prepare for the inevitable.
9. Can anything be done to slow down the end-stage liver failure timeline? While end-stage liver failure timeline progression is inevitable, some interventions can slow its course. Optimizing nutrition, avoiding alcohol, and managing complications like infections or bleeding can extend survival. Medications to reduce fluid buildup and ammonia levels can improve symptoms. Some patients may qualify for liver transplantation, offering a potential cure. However, once the liver reaches complete failure, treatment focuses on comfort rather than prolonging life.
10. What are the options for end-of-life care in advanced liver failure? For those in the final stages of liver failure before death, palliative and hospice care are critical options. Palliative care manages pain, nausea, and discomfort while addressing emotional and psychological needs. Hospice care provides comprehensive support for both patients and families, emphasizing dignity and quality of life. Discussions about advance directives, do-not-resuscitate (DNR) orders, and symptom relief strategies help ensure a peaceful passing. Early conversations about end-of-life wishes can reduce stress and ensure a compassionate approach to care.

Conclusion: Are Liver Health Supplements Worth It?
Liver health supplements, including Liver Health Formula and Liver Renew Formula, contain ingredients that have shown promise in supporting liver function. Compounds such as milk thistle, NAC, and turmeric have demonstrated hepatoprotective properties in scientific studies. However, the overall effectiveness of these supplements depends on multiple factors, including individual health status, diet, and lifestyle choices.
While these supplements may provide additional support for liver health, they should not replace medical treatment or healthy habits. Individuals experiencing symptoms of liver dysfunction, such as fatigue, jaundice, or abdominal pain, should seek medical advice rather than relying solely on supplements. Ultimately, the best approach to liver health involves a combination of a nutritious diet, physical activity, and moderation in alcohol consumption.
liver detox supplements, best liver support supplements, milk thistle liver benefits, natural liver detox remedies, liver health tips, liver support vitamins, turmeric for liver health, fatty liver treatment options, liver disease prevention, signs of liver damage, benefits of dandelion root, antioxidants for liver health, NAC for liver detox, herbal liver remedies, artichoke liver benefits, best foods for liver health, non-alcoholic fatty liver disease, glutathione for liver detox, liver cleansing diet, how to improve liver function naturally
Further Reading:
The Inside-Out of End-Stage Liver Disease: Hepatocytes are the Keystone
Palliative Care and End Stage Liver Disease
Liver Disease and Palliative Care
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.

