Understanding Fatty Liver Disease and Its Progression
Fatty liver disease, also known as hepatic steatosis, occurs when excessive fat accumulates in the liver. This condition is often linked to obesity, insulin resistance, metabolic syndrome, and excessive alcohol consumption. There are two primary types of fatty liver disease: alcoholic fatty liver disease (AFLD) and non-alcoholic fatty liver disease (NAFLD). The latter has become a growing concern worldwide due to the rising prevalence of obesity and sedentary lifestyles. NAFLD encompasses a spectrum of liver conditions, ranging from simple fatty liver (steatosis) to non-alcoholic steatohepatitis (NASH), fibrosis, cirrhosis, and eventually liver failure. Understanding the stages of fatty liver disease is crucial for early intervention, effective management, and prevention of severe liver damage.
You may also like: The Best Liver Detox Supplements: How to Choose Safe and Effective Support for Your Liver
The Initial Stage: Simple Hepatic Steatosis
The earliest phase of fatty liver disease is known as simple hepatic steatosis, where fat accumulates in the liver without causing significant inflammation or damage. Many individuals with this condition remain asymptomatic and may only discover it during routine health screenings. While hepatic steatosis is generally considered benign at this stage, it can progress to more severe liver conditions if lifestyle modifications are not made. Factors such as poor dietary habits, lack of physical activity, and genetic predisposition contribute to the development and persistence of hepatic steatosis.
Grade I Fatty Liver: The Beginning of Fat Accumulation
Grade I fatty liver is the mildest form of fatty liver disease, characterized by the presence of small fat deposits within liver cells. At this stage, liver function remains relatively normal, and no significant inflammation is observed. However, if left unaddressed, these fat deposits can increase, potentially triggering inflammatory responses that lead to more advanced stages of liver disease. The key to managing grade I fatty liver lies in dietary adjustments, increased physical activity, and weight management. Simple interventions, such as reducing sugar intake, avoiding processed foods, and incorporating regular exercise, can help reverse fatty liver and prevent progression.
Grade II Fatty Liver: Increasing Fat Deposition and Potential Risks
As fatty liver disease advances to grade II, fat accumulation within liver cells becomes more extensive. Unlike grade I fatty liver, where minimal inflammation is present, grade II fatty liver may show early signs of liver cell injury and inflammation. Although liver function may still be preserved, prolonged exposure to fat deposits can impair the liver’s ability to detoxify the blood, regulate metabolism, and process nutrients efficiently. Individuals at this stage may begin to experience mild symptoms such as fatigue, mild discomfort in the upper right abdomen, and unexplained weight gain. Medical professionals often recommend a more aggressive approach to lifestyle changes, including the adoption of a Mediterranean-style diet, regular cardiovascular and strength-training exercises, and close monitoring of blood sugar and cholesterol levels.
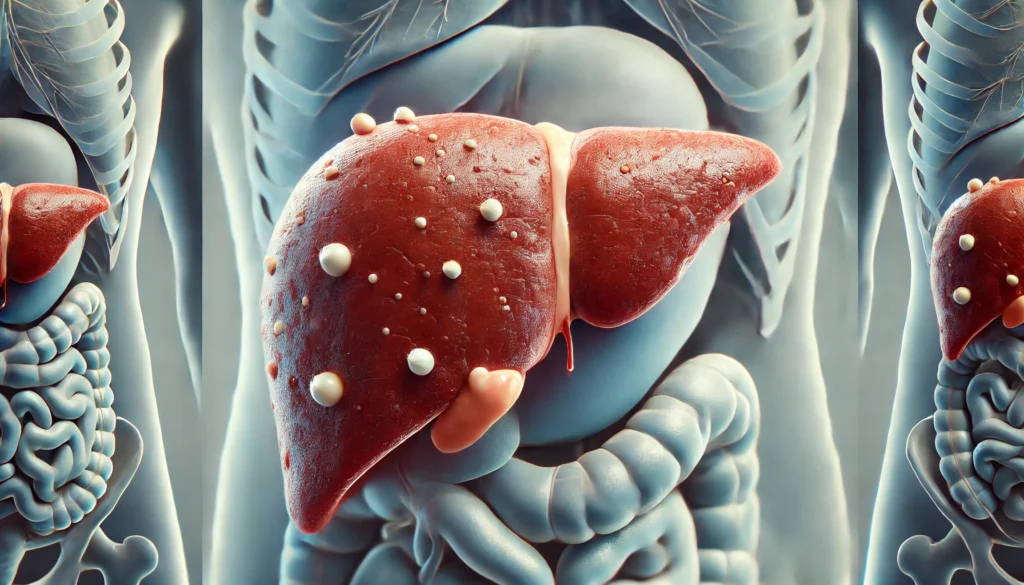
Fatty Liver Stage 3: The Onset of Fibrosis and Structural Damage
Fatty liver stage 3 marks a significant turning point in the progression of liver disease. At this stage, chronic inflammation leads to fibrosis, a condition characterized by the formation of scar tissue within the liver. Unlike simple hepatic steatosis, fibrosis indicates that liver cells have sustained considerable damage, and the body’s healing response is generating fibrotic tissue to replace normal liver cells. Although fibrosis does not yet signify irreversible liver failure, it significantly increases the risk of progression to cirrhosis. Symptoms such as persistent fatigue, jaundice, and fluid retention in the abdomen (ascites) may begin to manifest. Early diagnosis and intervention are critical at this stage to prevent further liver deterioration.
NASH Stage 3: The Progression Toward Cirrhosis
Non-alcoholic steatohepatitis (NASH) represents an advanced form of NAFLD where fatty deposits, inflammation, and fibrosis coexist. NASH stage 3 indicates significant liver fibrosis, approaching cirrhosis but still possessing some capacity for recovery if immediate lifestyle changes and medical interventions are implemented. Individuals with stage 3 NASH liver disease often face a heightened risk of liver-related complications, including hepatic encephalopathy, portal hypertension, and increased susceptibility to liver cancer. Addressing NASH at this stage requires a multifaceted approach, including medical therapies, controlled dietary interventions, and regular liver function monitoring. Advanced imaging techniques and biopsy evaluations help assess the extent of fibrosis and guide treatment strategies.
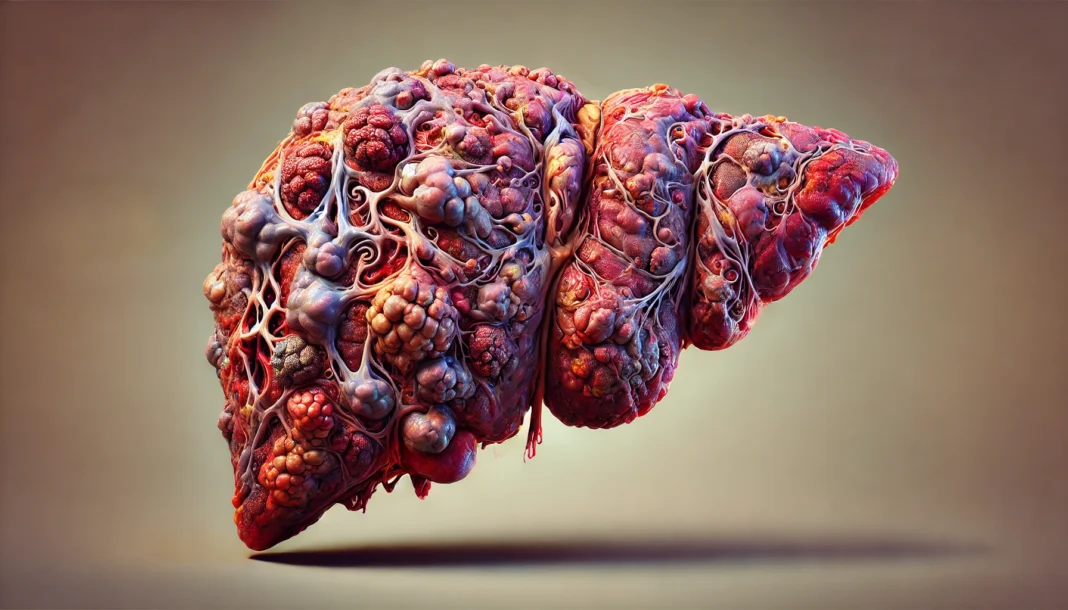
The Final Stage: Cirrhosis and End-Stage Liver Disease
Cirrhosis represents the most severe stage of fatty liver disease, where extensive fibrosis has permanently compromised liver function. At this point, normal liver tissue is largely replaced by scar tissue, leading to liver dysfunction and, in some cases, liver failure. Common complications associated with cirrhosis include severe jaundice, increased susceptibility to infections, variceal bleeding, and hepatic encephalopathy. Once cirrhosis develops, treatment options become limited, with liver transplantation often being the only viable long-term solution. Preventing progression to cirrhosis through early intervention in the earlier stages of fatty liver disease remains the most effective strategy.
The Difference Between Fatty Liver and Fibrosis
A common question that arises in discussions about fatty liver disease is: what is the difference between fatty liver and fibrosis? While fatty liver primarily refers to excessive fat accumulation within liver cells, fibrosis represents a structural alteration in liver tissue due to chronic inflammation and scarring. Fatty liver is generally reversible with lifestyle changes, whereas fibrosis signifies a more advanced stage where liver healing mechanisms have been compromised. Understanding this distinction is essential for recognizing the importance of early intervention and targeted treatment approaches.
Preventing and Managing Fatty Liver Disease
Prevention strategies for fatty liver disease revolve around lifestyle modifications that promote metabolic health. Maintaining a healthy weight, engaging in regular physical activity, and consuming a balanced diet rich in whole foods, lean proteins, and healthy fats can significantly reduce the risk of hepatic steatosis. Additionally, limiting alcohol intake, managing blood sugar levels, and monitoring cholesterol levels play crucial roles in preventing liver disease progression. In cases where fatty liver has already developed, medical professionals may recommend dietary interventions such as a low-glycemic diet, intermittent fasting, or supplementation with liver-supportive nutrients like omega-3 fatty acids, vitamin E, and antioxidants.
The Role of Medical Treatments and Emerging Therapies
While lifestyle changes form the cornerstone of fatty liver disease management, medical treatments and emerging therapies are being explored to halt or reverse liver damage. Pharmacological interventions, such as insulin-sensitizing agents, anti-inflammatory medications, and anti-fibrotic drugs, are under investigation for their potential to mitigate liver damage. Additionally, ongoing research in regenerative medicine and liver transplantation holds promise for individuals with advanced liver disease. Combining medical interventions with sustainable lifestyle changes enhances the likelihood of successful long-term outcomes.
Frequently Asked Questions (FAQ) About Fatty Liver and NASH
1. What are the key differences between fatty liver and fibrosis?
Fatty liver disease, also known as hepatic steatosis, is characterized by excessive fat accumulation in the liver cells, while fibrosis refers to scarring caused by prolonged liver damage. Fatty liver is generally reversible with lifestyle changes, whereas fibrosis indicates a more advanced stage of liver disease. In early hepatic steatosis stages, fat buildup occurs without significant scarring, but over time, persistent inflammation can lead to fibrosis. Understanding what is the difference between fatty liver and fibrosis helps in recognizing the severity of liver conditions and taking proactive measures to prevent progression. Fibrosis is more concerning as it indicates that the liver is sustaining permanent damage, potentially leading to cirrhosis if left untreated.
2. How serious is fatty liver stage 3?
Fatty liver stage 3 is a critical phase of non-alcoholic steatohepatitis (NASH), marked by extensive liver inflammation and fibrosis. At this stage, liver function is significantly compromised, and the risk of cirrhosis increases. Unlike grade I fatty liver or fatty liver stage 2, stage 3 represents advanced scarring, making lifestyle and medical intervention essential. Patients with stage 3 NASH liver disease often experience symptoms like fatigue, abdominal discomfort, and metabolic complications. Without timely intervention, fatty liver stage 3 can lead to irreversible cirrhosis, necessitating long-term monitoring and treatment.
3. Can grade 2 fatty liver be reversed?
Yes, grade 2 fatty liver can often be reversed with appropriate lifestyle modifications such as a healthy diet, regular exercise, and weight management. Unlike stage 3 NASH liver disease, which involves significant fibrosis, grade 2 fatty liver is still considered an intermediate stage where damage can be mitigated. Reducing sugar and processed food intake, increasing fiber consumption, and engaging in physical activity can help restore liver health. Early detection is crucial in reversing grade 2 fatty liver, as prolonged neglect can lead to progression into more severe hepatic steatosis stages. Medical guidance can help tailor interventions to individual needs for effective liver recovery.
4. What are the common risk factors for developing NASH stage 3?
NASH stage 3 is associated with metabolic syndrome, obesity, insulin resistance, and high cholesterol levels. Individuals with type 2 diabetes are at a higher risk due to chronic inflammation and insulin resistance contributing to liver damage. Unlike grade I fatty liver, where fat accumulation is mild, NASH stage 3 is marked by widespread fibrosis, increasing the risk of liver failure. Genetic predisposition and lifestyle factors, such as excessive alcohol consumption or poor dietary habits, also play a role in disease progression. Early lifestyle changes can help prevent progression from fatty liver stage 2 to advanced stages like stage 3 NASH liver disease.
5. What dietary changes help manage hepatic steatosis stages?
Managing hepatic steatosis stages involves adopting a balanced diet rich in lean proteins, whole grains, and healthy fats while minimizing processed sugars and trans fats. Unlike fatty liver stage 3, where medical intervention is often necessary, early stages can benefit significantly from dietary improvements. Foods high in antioxidants, such as berries, green tea, and leafy greens, can help reduce oxidative stress in the liver. Omega-3 fatty acids, found in fish and nuts, can also aid in reducing liver fat accumulation. Staying hydrated and avoiding excessive alcohol consumption are additional key strategies in supporting liver health.
6. How does exercise impact fatty liver progression?
Regular physical activity plays a vital role in preventing and managing fatty liver disease. Exercise helps reduce fat accumulation in the liver, improves insulin sensitivity, and decreases inflammation, which is critical in slowing the progression from fatty liver stage 2 to more advanced stages. Aerobic exercises like brisk walking, cycling, and swimming have been shown to improve hepatic steatosis stages by promoting fat metabolism. Strength training also contributes by enhancing muscle mass and boosting metabolic rate. A combination of both resistance and cardiovascular exercise can be highly effective in reversing early-stage fatty liver conditions.
7. What is the role of medication in treating stage 3 NASH liver disease?
While lifestyle modifications are the first line of defense, medications may be prescribed for individuals with stage 3 NASH liver disease. Certain drugs targeting insulin resistance, such as pioglitazone, have shown promise in reducing liver inflammation. Additionally, vitamin E supplementation is sometimes recommended for patients without diabetes to help reduce oxidative stress. Unlike grade I fatty liver, where dietary changes alone may suffice, advanced cases require medical intervention to slow fibrosis progression. Ongoing clinical trials are exploring potential pharmaceutical treatments to address the underlying causes of NASH and improve liver function.
8. How can I monitor my liver health if I have grade 2 fatty liver?
Routine liver function tests, imaging studies such as ultrasound or MRI, and monitoring metabolic markers like blood sugar and cholesterol are essential in tracking grade 2 fatty liver progression. Unlike stage 3 NASH liver disease, where significant fibrosis is present, grade 2 fatty liver remains in a modifiable state, making regular monitoring crucial. FibroScan is another non-invasive tool that assesses liver stiffness, helping to determine the extent of fibrosis. Physicians may also recommend periodic liver enzyme tests to evaluate any changes in inflammation or fat accumulation. Keeping track of body weight and waist circumference can also serve as indirect indicators of liver health.
9. What complications arise if fatty liver stage 3 progresses to cirrhosis?
If fatty liver stage 3 progresses unchecked, it can lead to cirrhosis, a condition where liver function becomes severely impaired due to extensive scarring. Cirrhosis can result in complications such as portal hypertension, liver failure, and an increased risk of liver cancer. Unlike earlier hepatic steatosis stages, where fat accumulation can still be managed, cirrhosis is largely irreversible. Symptoms like jaundice, fluid retention, and mental confusion may develop in advanced cases. Early intervention and regular medical follow-ups are key to preventing further progression and managing potential complications effectively.
10. Are there any emerging treatments for advanced NASH and fatty liver conditions?
Recent research into NASH and fatty liver treatments has focused on developing drugs targeting liver inflammation and fibrosis. Some promising therapies include FXR agonists, GLP-1 receptor agonists, and SGLT2 inhibitors, which aim to reduce fat accumulation and improve metabolic function. Unlike traditional treatments focused on lifestyle changes, these emerging therapies provide new options for those with advanced NASH stage 3 and stage 3 NASH liver disease. Clinical trials are also investigating the role of gut microbiota in liver health, exploring probiotics and prebiotics as potential interventions. While no FDA-approved medication specifically for NASH exists yet, ongoing advancements provide hope for more effective treatment options in the near future.

Conclusion: The Importance of Early Detection and Proactive Management
The stages of fatty liver disease underscore the critical importance of early detection, proactive management, and lifestyle modifications in preventing severe liver complications. By recognizing the warning signs and understanding the progression of hepatic steatosis stages, individuals can take informed steps to improve their liver health. Whether dealing with grade I fatty liver, fatty liver stage 3, or NASH stage 3 liver disease, early intervention remains the key to reversing or slowing disease progression. Through a combination of dietary modifications, regular exercise, and emerging medical treatments, individuals can protect their liver and overall well-being for years to come.
fatty liver symptoms, liver health and diet, hepatic steatosis treatment, liver fibrosis vs fatty liver, NASH liver disease management, best diet for fatty liver, non-alcoholic fatty liver disease prevention, fatty liver and metabolic syndrome, liver detoxification strategies, reducing liver inflammation naturally, early signs of liver disease, managing insulin resistance and liver health, obesity and fatty liver disease, liver cirrhosis prevention, liver-supporting nutrients, lifestyle changes for liver health, alcohol and liver damage, liver disease screening, chronic liver disease management, metabolic health and liver function
Further Reading:
Nonalcoholic Steatohepatitis (NASH)
Mechanisms and disease consequences of nonalcoholic fatty liver disease
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.