Cardiovascular disease (CVD) continues to be the leading cause of death worldwide, cutting across gender, age, and geography. It encompasses a range of conditions, including coronary artery disease, ischemic heart disease, and those related to high calcium scores, which signal the presence of calcified plaque in the arteries. As our understanding of the relationship between nutrition and cardiovascular disease evolves, one fact remains constant: dietary choices play a pivotal role not only in preventing heart disease but also in optimizing physical endurance and performance. The intersection of cardiovascular nutrition and stamina training opens new pathways for enhancing overall well-being through evidence-based, strategic dietary approaches. For athletes, fitness enthusiasts, and individuals managing chronic cardiovascular conditions, embracing a diet tailored to heart health offers both protective and performance-enhancing benefits.
Modern dietary science has shed light on how specific foods and nutrients influence cardiovascular outcomes. Nutrients affect everything from lipid profiles and blood pressure to endothelial function and inflammatory markers. At the same time, endurance athletes and those pursuing performance enhancement require robust cardiovascular support to sustain exertion, oxygen delivery, and energy metabolism. Integrating a heart-healthy diet into an endurance-focused lifestyle is not only synergistic but essential. This article explores the science and strategy behind choosing the right foods for cardiovascular support, the nuanced differences in dietary approaches depending on specific heart-related risks such as ischemic heart disease or a high calcium score, and how these choices influence both long-term health and short-term performance outcomes.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice
Understanding Cardiovascular Nutrition in the Context of Endurance
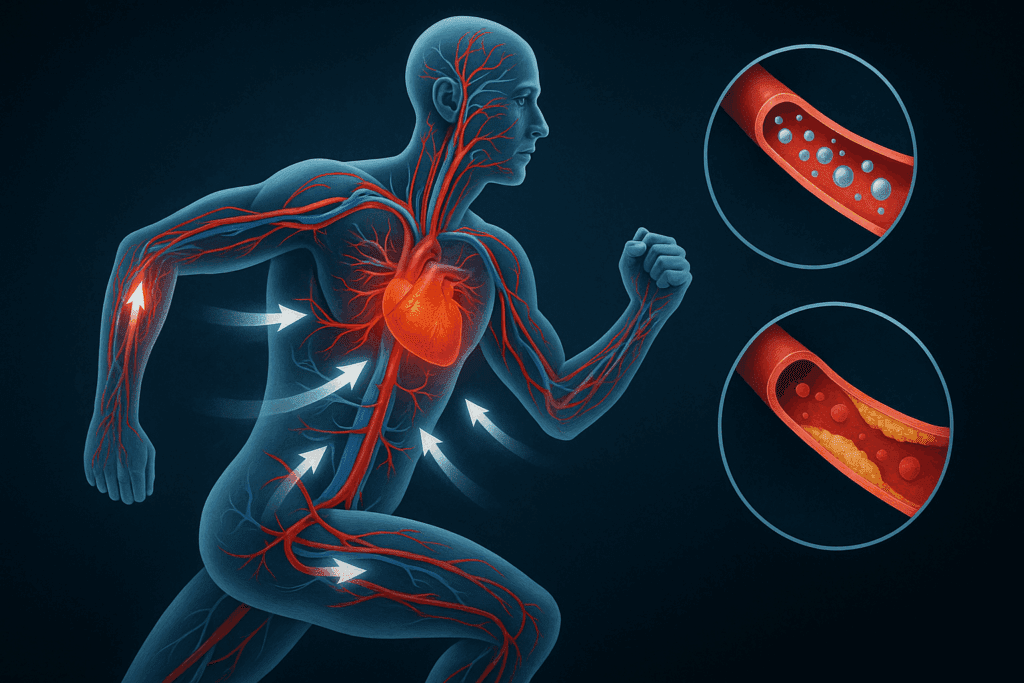
To appreciate the power of cardiovascular nutrition, it’s important to understand how the heart and vascular system support physical performance. During endurance activity, the heart pumps oxygen-rich blood to muscles, facilitating aerobic respiration. When the arteries are narrowed due to plaque buildup, as is common in individuals with a high calcium score or existing CVD, the heart must work harder, and oxygen delivery becomes compromised. This not only reduces performance but elevates the risk of cardiac events during physical exertion.
In this context, nutrition and heart disease are inextricably linked. A poor diet can accelerate atherosclerosis, elevate blood pressure, and disrupt lipid balance. Conversely, a strategically designed diet for ischemic heart disease or one addressing cvd nutrition more broadly can significantly reduce plaque progression, stabilize existing lesions, and improve endothelial function. Foods rich in omega-3 fatty acids, antioxidants, fiber, and anti-inflammatory compounds have demonstrated measurable improvements in cardiovascular markers. These same nutrients also support mitochondrial function and reduce oxidative stress—key determinants of stamina and recovery in physically active individuals.
Furthermore, for those seeking peak physical performance, cardiovascular health becomes the limiting factor when it is compromised. You cannot build endurance on a shaky foundation. A focus on cardiovascular nutrition bridges the gap between athletic training and medical dietary therapy, bringing together elite sports performance and chronic disease prevention. With growing interest in dual-purpose dietary strategies—those that reduce risk while optimizing energy systems—nutrition is no longer seen as ancillary but central to heart and stamina health.
The Role of Diet in Managing Ischemic Heart Disease
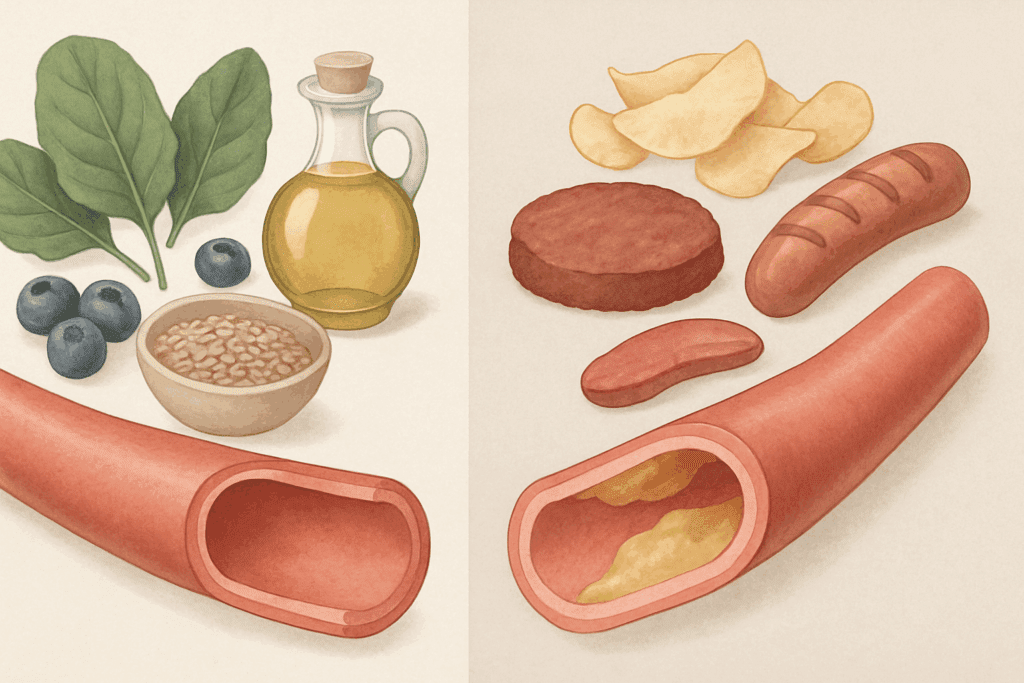
Ischemic heart disease, characterized by reduced blood flow to the heart muscle, remains one of the most pressing cardiovascular concerns today. Dietary modification is a cornerstone of therapy, particularly in reducing modifiable risk factors such as high LDL cholesterol, elevated triglycerides, hypertension, and systemic inflammation. Designing a diet for ischemic heart disease means emphasizing foods that lower lipid levels, enhance nitric oxide availability for vasodilation, and improve overall endothelial resilience.
Leafy green vegetables, fatty fish like salmon and sardines, whole grains, legumes, and berries should form the core of this dietary approach. These foods provide soluble fiber, plant sterols, polyphenols, and long-chain omega-3s that improve vascular tone and reduce the oxidative damage associated with ischemic injury. In contrast, processed foods, trans fats, and excessive sodium contribute directly to vascular stiffness and plaque instability. Understanding which foods to avoid with high calcium score or signs of ischemia is as important as knowing what to consume.
Beyond general dietary recommendations, emerging evidence supports a more tailored approach. Individuals with ischemic heart disease may benefit from a Mediterranean-style or DASH-inspired plan enriched with foods that specifically modulate endothelial function and inflammatory cytokines. The addition of functional foods such as flaxseed, turmeric, and pomegranate may offer adjunctive benefits. A well-structured diet for ischemic heart disease can improve exercise tolerance, reduce anginal episodes, and lower the long-term risk of adverse cardiac events, empowering individuals to maintain an active lifestyle.
How High Calcium Scores Inform Dietary Choices
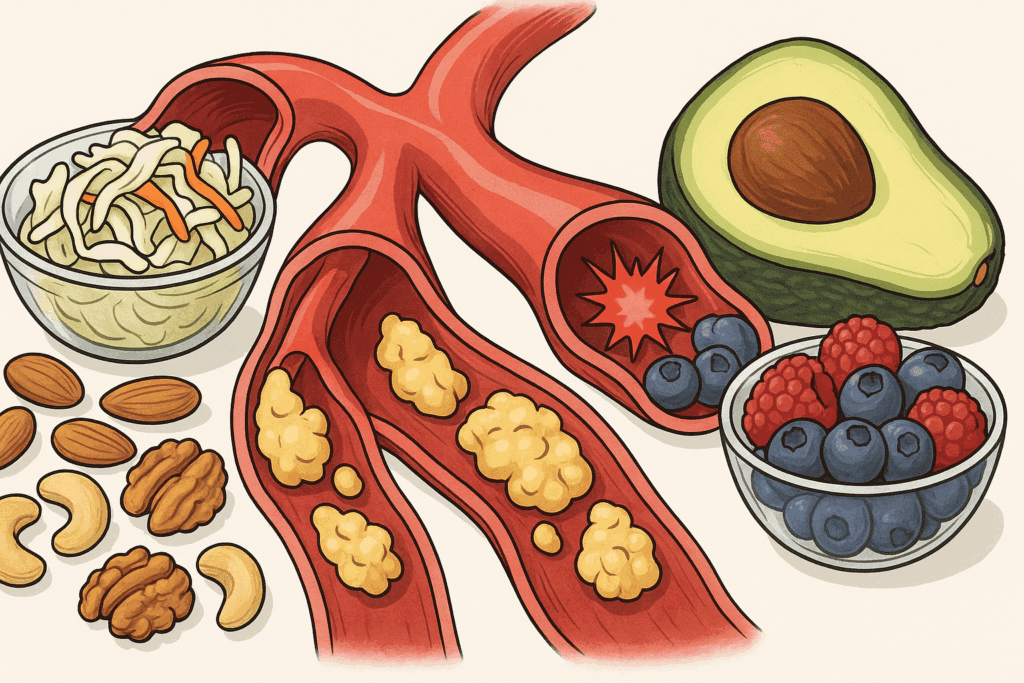
A high calcium score indicates significant plaque accumulation in coronary arteries, suggesting a high risk of future cardiovascular events. While the calcium itself is inert, its presence signals chronic inflammation and metabolic imbalance that has resulted in arterial calcification. In response, dietary intervention should prioritize anti-inflammatory foods, blood sugar regulation, and lipid control. Designing a diet for high calcium score is not about quick fixes but long-term metabolic harmony.
Whole plant-based foods, nuts, seeds, and low-glycemic fruits serve as foundational components. These foods reduce LDL oxidation and modulate insulin sensitivity—two mechanisms implicated in arterial calcification. Foods high in magnesium, potassium, and vitamin K2 are particularly valuable, as they influence calcium metabolism and vascular elasticity. On the flip side, foods to avoid with high calcium score include processed meats, refined carbohydrates, and high-sodium packaged items, all of which are linked to arterial stiffness and systemic inflammation.
Incorporating fermented foods such as kimchi, sauerkraut, and kefir can support gut microbiota diversity, which in turn regulates inflammatory responses that exacerbate plaque progression. Furthermore, intermittent fasting or time-restricted feeding has shown potential in improving cardiovascular markers among individuals with elevated calcium scores. While no diet can reverse calcification, adopting cardiovascular nutrition strategies aimed at halting progression can drastically lower the risk of heart attack and stroke and improve exercise capacity.

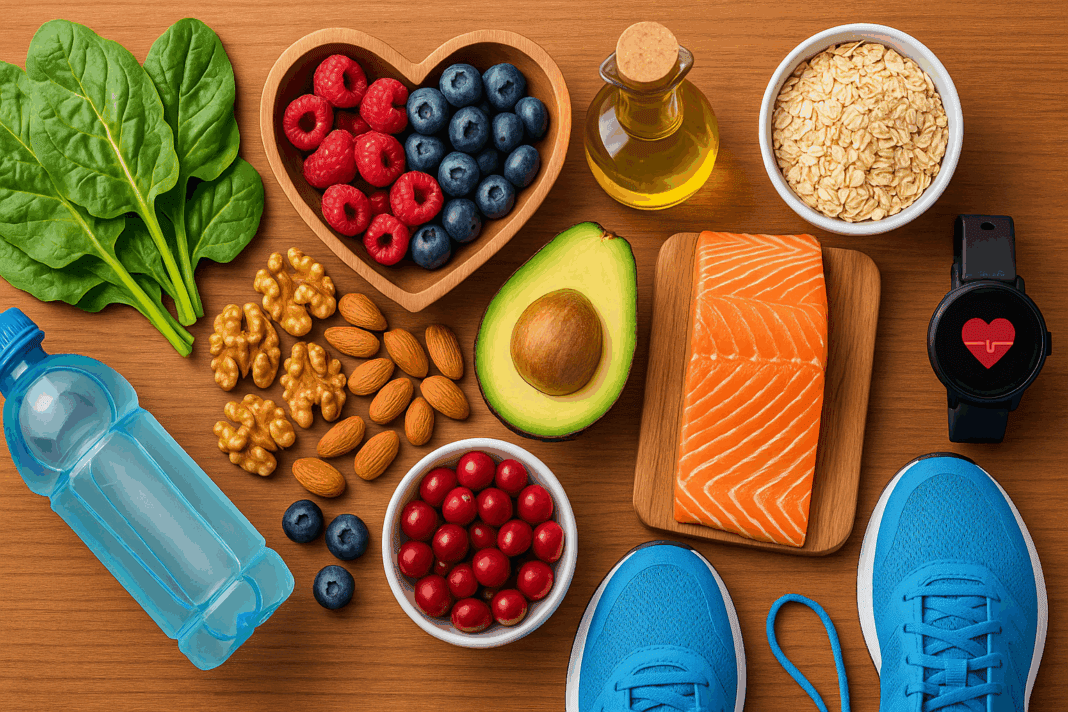
Foods That Support Cardiovascular Function and Physical Stamina
Certain foods not only protect the heart but actively support endurance and stamina. Understanding the dual-purpose nature of these foods is key to optimizing both cardiovascular health and athletic performance. Beets and beetroot juice, for example, are high in nitrates, which enhance nitric oxide production, leading to improved blood flow and lower oxygen cost during exercise. Athletes and individuals with cardiovascular concerns alike can benefit from this simple yet effective intervention.
Similarly, fatty fish provides EPA and DHA, omega-3 fatty acids that reduce inflammation, stabilize cardiac rhythms, and enhance mitochondrial efficiency. For those managing diet and CVD risk simultaneously, incorporating fish two to three times per week supports both recovery and plaque stabilization. Legumes such as lentils and chickpeas offer plant-based protein, fiber, and polyphenols that improve glycemic control and support steady energy release—crucial for long bouts of exercise and overall cardiovascular health.
Dark leafy greens like spinach and kale provide folate, magnesium, and antioxidants that counteract oxidative stress and assist in homocysteine metabolism—a marker associated with heart disease when elevated. Finally, dark-colored fruits like blueberries and blackberries supply anthocyanins, which improve vascular reactivity and reduce exercise-induced muscle damage. Collectively, these foods illustrate the core principles of cvd nutrition: choose foods that heal, energize, and sustain.
Strategic Nutritional Patterns for Cardiovascular Health and Endurance
Dietary patterns matter as much as individual food choices. A well-balanced dietary framework ensures consistency and synergy across nutrients. The Mediterranean diet, which emphasizes whole grains, healthy fats, fresh produce, and moderate fish and poultry intake, remains one of the most researched and recommended patterns for cardiovascular health. Its anti-inflammatory and antioxidant-rich profile supports both the prevention of heart disease and the metabolic demands of endurance training.
The DASH diet (Dietary Approaches to Stop Hypertension) has also proven effective in managing blood pressure and improving arterial health. For athletes or active individuals with high blood pressure or a family history of heart disease, incorporating DASH principles can offer protection while supporting training goals. Another emerging approach is plant-forward eating, which does not eliminate animal products entirely but prioritizes plants as the primary source of nutrition, aligning well with both sustainability and cardiovascular objectives.
For those needing a diet for ischemic heart disease or managing a diet for high calcium score, blending Mediterranean and DASH elements can be a highly effective strategy. Structured meal timing, mindful eating, and attention to glycemic load further optimize metabolic responses during and after exercise. Importantly, these patterns also contribute to weight management, which is a modifiable risk factor for CVD and a determinant of athletic performance.
The Interplay Between Macronutrients and Cardiovascular Performance
Macronutrients—carbohydrates, fats, and proteins—play distinct roles in cardiovascular health and physical stamina. Carbohydrates serve as the primary energy source during moderate to high-intensity exercise. However, quality matters. Refined carbohydrates spike insulin and promote fat storage, while complex carbs such as quinoa, oats, and sweet potatoes provide steady energy and support vascular function. Within the context of cvd nutrition, the emphasis is on glycemic control, fiber intake, and whole grain consumption.
Fats are equally crucial. Monounsaturated and polyunsaturated fats, found in olive oil, avocados, nuts, and seeds, reduce LDL cholesterol and improve HDL levels, thereby enhancing lipid profiles. Saturated fats, when consumed in excess, promote atherogenesis and should be limited, especially in a diet for ischemic heart disease. However, not all saturated fats are harmful—those from whole foods like coconut or pasture-raised meats may be tolerated in moderation, depending on individual lipid responses.
Protein intake supports muscle repair and vascular integrity, particularly in individuals engaged in resistance or endurance training. Plant-based proteins such as tofu, tempeh, and legumes offer cardiovascular benefits, while lean animal proteins like turkey and fish provide high bioavailability of essential amino acids. Strategic distribution of protein across meals ensures sustained repair and reduced muscle catabolism. Balancing macronutrients according to physical demands and cardiovascular goals creates a dietary synergy that supports long-term performance and heart health.

Supplements and Functional Foods for Cardiovascular Support
While whole foods should form the foundation of any nutritional approach, targeted supplementation can play a supportive role, particularly when nutrient gaps are present. Omega-3 fatty acids from fish oil or algae-based supplements are commonly recommended for individuals seeking cardiovascular support. They are especially useful when dietary intake is insufficient or when managing elevated triglycerides or systemic inflammation.
Coenzyme Q10 (CoQ10), a mitochondrial cofactor, has been shown to improve endothelial function, reduce blood pressure, and support energy production. It is particularly relevant in cases of statin-induced myopathy or chronic fatigue in heart patients. Magnesium, which supports vascular tone and muscle function, is often deficient in modern diets and can enhance both blood pressure regulation and recovery from training. For those with a high calcium score, vitamin K2 supplementation has gained attention for its potential role in directing calcium away from arteries and toward bone tissue.
Functional foods, including green tea, cacao, garlic, and turmeric, offer bioactive compounds that modulate inflammation, lipid metabolism, and oxidative stress. These foods can be incorporated daily to enhance both performance and cardiovascular protection. Still, supplements should be used judiciously and under medical supervision, particularly when managing nutrition and heart disease in clinical settings.
Long-Term Lifestyle Integration for Sustainable Cardiovascular Health
Sustaining dietary change requires more than knowledge—it demands behavioral strategies, support systems, and adaptability. Meal prepping, mindful grocery shopping, and learning to cook simple, flavorful meals can help reinforce cardiovascular nutrition habits. For athletes and active individuals, coordinating nutrition with training cycles enhances both compliance and outcomes. Tracking biomarkers such as cholesterol, triglycerides, blood glucose, and blood pressure can provide tangible feedback and motivate ongoing effort.
It’s also essential to adapt nutrition strategies during different life stages. Older adults may require higher protein intake to preserve lean mass, while younger athletes might focus on fueling growth and recovery. Women, particularly post-menopausal, face unique cardiovascular risks and may benefit from phytoestrogen-rich foods like flaxseed and soy. Cultural preferences, budget considerations, and personal taste must also be accounted for to create an individualized, sustainable eating plan.
Ultimately, the goal is not short-term compliance but long-term integration. A performance-focused diet that simultaneously reduces cardiovascular risk offers the best of both worlds. As awareness grows around the importance of dietary choices, empowering individuals with practical, science-backed strategies becomes the cornerstone of modern preventive and performance medicine.
The Future of Diet and CVD Prevention: Embracing Innovation and Personalization
As nutrition science advances, the future of cardiovascular dietary strategy will likely involve greater personalization. Genetic testing, microbiome analysis, and continuous glucose monitoring are opening new frontiers in tailoring diet plans to individual risk profiles and metabolic patterns. For example, some individuals may have genetic variants that affect lipid metabolism or inflammatory responses, making them more responsive to certain fats or antioxidants.
The integration of artificial intelligence into nutrition tracking, combined with wearable technology, allows real-time adjustment of dietary choices to match cardiovascular demands during training and recovery. These innovations hold promise for those managing diet for ischemic heart disease or looking to optimize performance without sacrificing heart health. Personalized supplementation protocols and AI-generated meal plans may soon replace one-size-fits-all recommendations, ensuring greater efficacy and adherence.
Nevertheless, foundational principles remain unchanged. Whole, unprocessed foods, consistent meal patterns, and the avoidance of inflammatory, highly processed options continue to be the backbone of cardiovascular nutrition. As we continue to uncover the intricate links between diet and CVD, the focus shifts toward empowering individuals with the tools and knowledge to make informed, health-enhancing decisions.
Frequently Asked Questions: Nutrition and Cardiovascular Disease
1. How does psychological stress interact with cardiovascular nutrition to influence heart health?
Psychological stress has a profound impact on cardiovascular health, and its relationship with nutrition is often underappreciated. Chronic stress can disrupt hormonal balance, elevate cortisol, and increase blood pressure, all of which compound the risks associated with poor dietary patterns. When combined with a suboptimal diet and CVD risk factors, stress may accelerate endothelial damage and plaque formation. Research now explores how anti-inflammatory foods in a cardiovascular nutrition plan may buffer stress-related damage, particularly when combined with stress-reducing practices like mindfulness. This is especially relevant in constructing a diet for ischemic heart disease, as psychological resilience may enhance the effectiveness of dietary strategies designed to reduce arterial inflammation.
2. Are there social or cultural considerations when designing a diet for high calcium score?
Yes, cultural dietary patterns must be taken into account when building a sustainable diet for high calcium score. For instance, traditional Mediterranean diets, which naturally include high levels of cardiovascular-friendly fats and antioxidants, differ significantly from East Asian diets that emphasize fermented vegetables and fish. Tailoring cardiovascular nutrition to cultural preferences improves adherence and ensures nutritional adequacy without sacrificing flavor. Understanding local food sources also allows for more creative substitutions when avoiding foods that exacerbate calcification, such as processed meats or sodium-rich condiments. Culturally inclusive approaches to nutrition and heart disease ensure that dietary recommendations are not only effective but also practical and respectful of individual heritage.
3. Can athletes safely follow a diet and CVD prevention plan without compromising performance?
Athletes can absolutely benefit from a diet and CVD prevention strategy when it is properly structured. A common misconception is that heart-healthy diets are too low in energy or fats to sustain endurance. In reality, a diet for ischemic heart disease or for general cardiovascular support can be high in nutrient-dense calories from sources like avocados, nuts, whole grains, and fatty fish. These foods support mitochondrial function and oxygen utilization, which are crucial for endurance. With smart planning and emphasis on timing and macronutrient distribution, athletic performance can improve alongside cardiovascular resilience.
4. What are some emerging research trends in nutrition and cardiovascular disease?
One exciting area of emerging research is the role of the gut microbiome in shaping cardiovascular outcomes. Scientists are exploring how specific bacteria, influenced by dietary fiber and polyphenols, produce metabolites that either protect or harm cardiovascular health. This adds a new layer to cvd nutrition, as fiber-rich diets may reduce inflammation and arterial stiffness by supporting beneficial microbial populations. Personalized nutrition based on microbiome profiles is likely to become a significant part of future cardiovascular care. These findings encourage more precise tailoring of diet for high calcium score and ischemic conditions to promote optimal gut-heart interactions.
5. Why is it important to monitor hidden sources of sodium in cardiovascular nutrition?
Many people trying to follow a heart-healthy eating plan are unaware of how much sodium is hidden in everyday foods. Packaged items like breads, salad dressings, and even breakfast cereals can significantly increase sodium intake, contributing to high blood pressure and worsening CVD outcomes. For those managing nutrition and heart disease, carefully reading labels and preparing more meals at home allows for greater control over sodium content. A diet for high calcium score particularly benefits from this strategy, as excessive sodium intake has been linked to arterial calcification and stiffening. Eliminating or reducing hidden sodium supports better blood pressure control and vascular integrity.
6. How do sleep habits influence the effectiveness of a diet for ischemic heart disease?
Sleep plays a crucial role in modulating inflammation, hormonal regulation, and metabolic control, all of which impact the success of a diet for ischemic heart disease. Poor sleep can lead to increased cravings for high-fat and high-sugar foods, undermining cardiovascular nutrition goals. Additionally, insufficient sleep raises cortisol levels, which can promote arterial plaque instability. Integrating consistent, high-quality sleep into a CVD-focused lifestyle plan helps reinforce the benefits of diet and endurance training. Healthcare providers increasingly recommend that sleep hygiene be discussed alongside diet and CVD risk management.
7. What are some unexpected foods to avoid with high calcium score?
Beyond obvious culprits like processed meats and sugary snacks, some health-labeled foods can be problematic for those with high calcium scores. Granola bars, for instance, often contain trans fats and added sugars despite their healthy image. Energy drinks, even those labeled as natural, can contribute to endothelial dysfunction due to high caffeine and sodium content. Over-reliance on calcium-fortified juices or supplements without adequate vitamin K2 may also contribute to arterial calcification. These lesser-known examples underscore the importance of scrutinizing labels when managing foods to avoid with high calcium score in a comprehensive cardiovascular nutrition plan.
8. How can plant-based diets be adapted for those managing diet and heart disease together?
Plant-based diets can be highly effective when managing diet and heart disease, but they must be strategically structured. Simply avoiding animal products does not automatically ensure cardiovascular benefits; refined grains and processed vegan products can still elevate CVD risk. Whole food-based plant diets that emphasize legumes, whole grains, nuts, seeds, and a variety of vegetables offer the best outcomes. Attention must also be paid to nutrients like B12, iron, and omega-3s, which can be less abundant in plant-based plans. When carefully composed, these diets can align perfectly with a diet for ischemic heart disease and deliver powerful anti-inflammatory effects.
9. Can cardiovascular nutrition improve mental clarity and cognitive function?
Yes, cardiovascular nutrition may significantly influence brain health due to the shared vascular pathways between heart and cognitive function. A diet that supports endothelial health improves cerebral blood flow, which is essential for memory, focus, and mood stability. Nutrients like omega-3 fatty acids, flavonoids, and magnesium—which are commonly included in a diet and CVD prevention plan—have also been shown to reduce cognitive decline. Chronic inflammation and insulin resistance are risk factors for both heart disease and dementia, highlighting the overlapping nature of these conditions. This makes nutrition and cardiovascular disease management a key strategy in promoting long-term mental performance.
10. What lifestyle tools can help reinforce consistency with cvd nutrition habits?
Behavioral tools such as habit tracking, meal journaling, and mobile nutrition apps can greatly enhance consistency when following a cvd nutrition plan. These tools provide immediate feedback, helping individuals make real-time adjustments and stay aligned with their dietary goals. Joining peer support groups or working with a registered dietitian can also improve accountability and motivation. For those managing both nutrition and heart disease, even simple rituals like a weekly meal prep session or a regular morning smoothie routine can build long-term success. Embedding nutrition habits into a broader lifestyle framework ensures that dietary changes are sustainable, enjoyable, and impactful.
Conclusion: Smart Dietary Strategies for Heart Health and Endurance Longevity
In an era where both cardiovascular disease and performance optimization are top priorities, the role of strategic nutrition has never been more critical. From tailoring a diet for ischemic heart disease to selecting foods that align with a high calcium score, the path to cardiovascular resilience is paved with informed dietary decisions. Nutrition and cardiovascular disease are no longer separate conversations—they are deeply interconnected dialogues with wide-reaching implications for healthspan and physical capacity.
Embracing a framework of cardiovascular nutrition empowers individuals to not only reduce their risk of adverse cardiac events but also to enhance their endurance, recovery, and day-to-day energy. Whether the goal is managing diet and CVD risk, supporting athletic training, or simply living with vitality, the power of food should not be underestimated. Every bite carries the potential to either nourish or diminish heart health. By focusing on nutrient-dense, anti-inflammatory, and performance-supporting foods, individuals can take control of their health with precision and purpose.
Ultimately, the journey toward heart health and endurance longevity begins with a single meal—but it doesn’t end there. It evolves through daily choices, sustained habits, and a commitment to lifelong well-being. With the right knowledge and support, anyone can master the art of using nutrition to fortify the heart and fuel a thriving, active life.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.