Understanding the Role of Inpatient Eating Disorder Clinics
In the realm of modern mental health care, inpatient eating disorder clinics provide a structured and intensive level of support for individuals battling severe eating disorders. These facilities are designed to offer round-the-clock medical, psychological, and nutritional care in a safe and controlled environment. For individuals whose conditions have escalated beyond the scope of outpatient treatment, eating disorder inpatient treatment often becomes a necessary step in the path to recovery. The controlled setting allows for close monitoring of both physical and psychological health, ensuring that patients receive timely interventions and continuous support throughout their stay.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
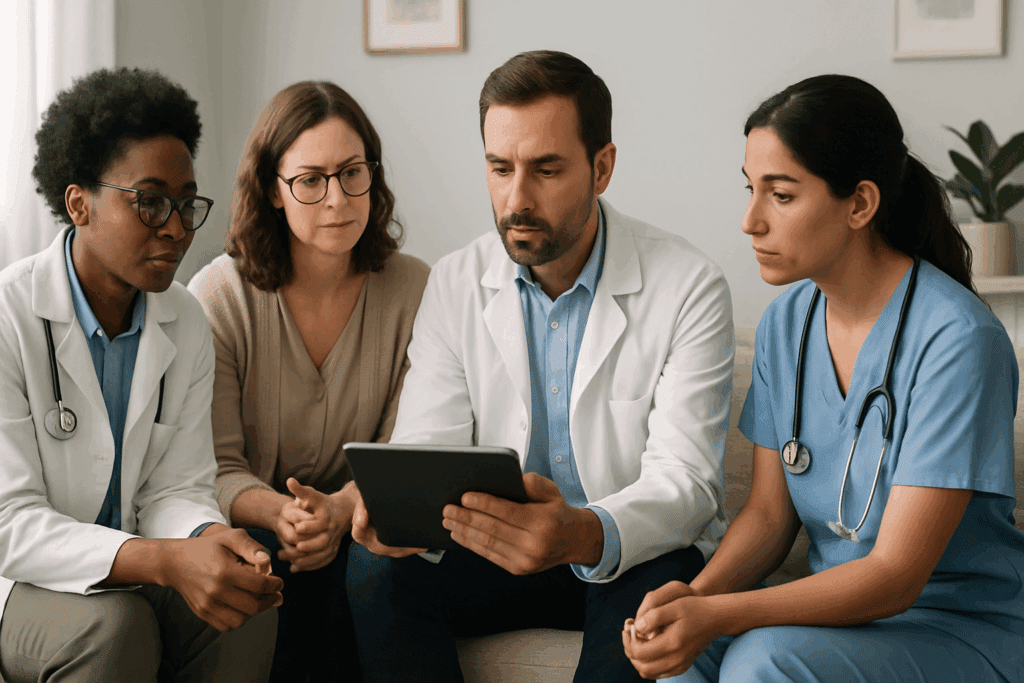
The role of an inpatient eating disorder clinic is multifaceted, involving a team of experts from different fields—psychiatrists, psychologists, dietitians, nurses, and therapists—all collaborating to address the complex nature of these disorders. This comprehensive, multidisciplinary approach helps to uncover and manage the root causes of the condition, which often extend beyond food and body image to include trauma, anxiety, and co-occurring mental health disorders. Inpatient care not only stabilizes the individual medically but also provides a foundation for long-term psychological healing and emotional regulation.
One of the primary advantages of inpatient eating disorder treatment is the removal of external triggers. Being removed from potentially harmful environments—whether they be family-related, socially influenced, or digitally perpetuated—helps patients focus entirely on their recovery. It’s a sanctuary where meals are supervised, unhealthy behaviors are monitored and addressed, and therapeutic goals can be pursued with intention and consistency. This structured environment is critical for individuals who have become trapped in dangerous patterns of restriction, purging, or binge eating that threaten both their physical health and quality of life.
Moreover, inpatient settings offer a crucial sense of community. Isolation is a common theme among those suffering from eating disorders, and being surrounded by others who share similar experiences can foster empathy, understanding, and motivation. Group therapy sessions and peer interactions help patients recognize that they are not alone in their struggles, which in itself is a powerful therapeutic tool. When patients feel seen and validated, their sense of self-worth begins to rebuild, creating space for genuine healing to occur.
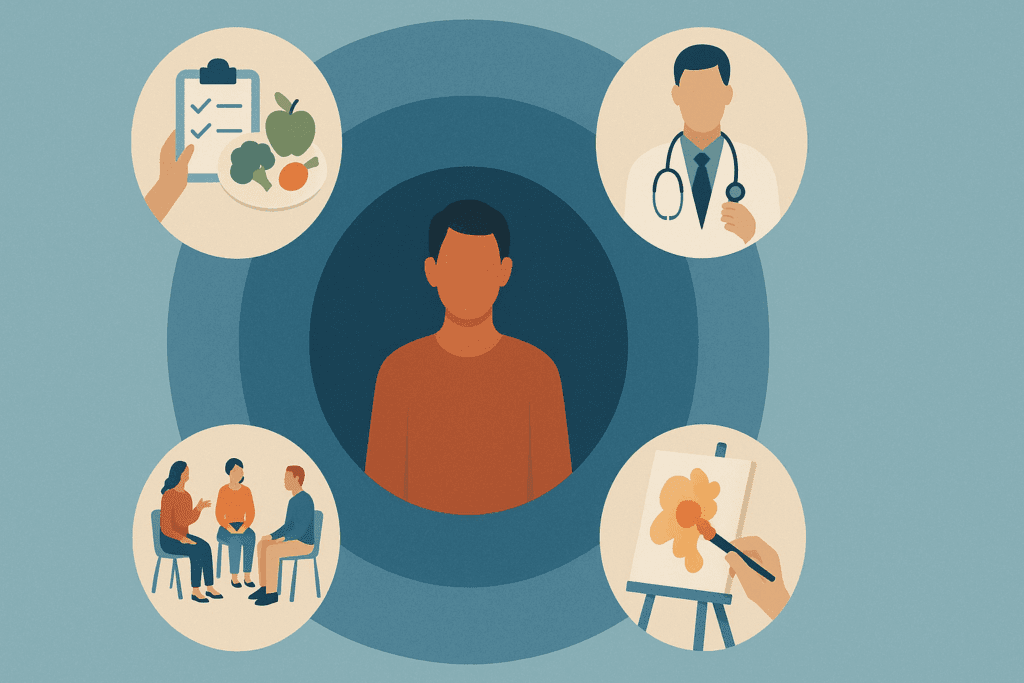
Ultimately, the goal of an inpatient eating disorder clinic is not only to treat the symptoms but to equip individuals with the skills and resilience needed to maintain recovery in the long term. From personalized meal plans and behavior modification strategies to cognitive therapy and family education, the tools provided in this environment extend far beyond discharge. Recovery is a lifelong journey, and inpatient care lays the critical groundwork needed to embark on that path with confidence.
When Is Inpatient Eating Disorder Treatment Necessary?
Determining the appropriate level of care for someone with an eating disorder involves a careful evaluation of physical, emotional, and behavioral factors. Inpatient eating disorder treatment is generally recommended when outpatient care is no longer sufficient to ensure safety or therapeutic progress. This often includes individuals with dangerously low body weight, electrolyte imbalances, cardiac complications, or other life-threatening conditions that result from prolonged disordered eating behaviors.
One of the most critical indicators for inpatient care is medical instability. For instance, when vital signs such as heart rate, blood pressure, or organ function are significantly compromised, the immediate need is to stabilize the body. Eating disorder inpatient treatment facilities are equipped to manage such acute conditions with medical oversight, while simultaneously initiating psychological support. This dual focus ensures that treatment addresses both the physical symptoms and the underlying emotional turmoil that drives the disorder.
Psychological deterioration is another strong indication for inpatient treatment. Individuals who experience overwhelming feelings of depression, suicidal ideation, or severe anxiety in connection with their eating habits may benefit from the intensive support available in an inpatient setting. These emotional disturbances often act as both causes and consequences of disordered eating, creating a vicious cycle that requires concentrated therapeutic intervention to break.
Behavioral patterns also play a role in identifying the need for inpatient care. For individuals who engage in extreme behaviors—such as frequent self-induced vomiting, laxative abuse, excessive exercise, or severe food restriction—an inpatient setting provides the necessary supervision and intervention to prevent further harm. These behaviors can escalate quickly, putting the individual at increased risk of long-term physical and psychological damage if not promptly addressed in a structured environment.
Additionally, failure to progress in less intensive treatment settings can prompt a transition to inpatient care. When individuals have participated in outpatient or intensive outpatient programs without notable improvement, or when they repeatedly relapse, it may be time to consider the more immersive support offered by an inpatient eating disorder clinic. Making this transition can mark a turning point, offering a higher level of care that may finally initiate meaningful progress.
The Multidisciplinary Approach to Treatment in Inpatient Clinics
Inpatient eating disorder clinics are grounded in a multidisciplinary model that ensures patients receive holistic, individualized care. Unlike general hospital admissions that may focus solely on medical stabilization, these specialized clinics incorporate an array of therapeutic disciplines to treat the condition from every possible angle. This integration of expertise helps to unravel the complex interplay between biological, psychological, and social factors that contribute to eating disorders.
At the heart of this approach is medical care, which involves constant monitoring by physicians and nurses trained in eating disorder management. These professionals track weight restoration, hydration, cardiovascular health, and potential refeeding syndrome—an often-overlooked complication in patients who begin nutritional rehabilitation. Medical staff also adjust medications when necessary and collaborate with psychiatrists to manage any coexisting psychiatric conditions, such as obsessive-compulsive disorder, PTSD, or mood disorders.
Nutritional rehabilitation is another cornerstone of inpatient eating disorder treatment. Registered dietitians work with patients to develop personalized meal plans that not only restore physical health but also challenge harmful beliefs about food. These plans are often flexible yet structured, providing a safe and supportive path toward normalized eating behaviors. Patients receive education on balanced nutrition, food groups, and portion sizes, helping to demystify and destigmatize the act of eating.
Psychotherapy is equally central in the treatment process. Inpatient clinics typically offer a range of therapeutic modalities, including cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), and family-based therapy. These interventions help patients identify and reframe destructive thoughts, regulate emotions, and improve communication with loved ones. Individual sessions provide a private space to delve into personal trauma and internal conflicts, while group therapy offers opportunities for social support and shared insight.
Moreover, recreational and expressive therapies—such as art therapy, yoga, and movement therapy—are often incorporated to help individuals reconnect with their bodies in a non-judgmental, affirming way. These modalities can be particularly effective in rebuilding body image, developing mindfulness, and promoting emotional expression without the use of words. The inclusion of such therapeutic options reinforces the notion that healing is not linear and must encompass the whole self.
Life Inside an Inpatient Eating Disorder Clinic
Life inside an inpatient eating disorder clinic is structured, intentional, and highly therapeutic. Days are organized around a carefully planned schedule that includes meals, therapy sessions, medical check-ins, and activities designed to support recovery. This structure helps patients establish routine and consistency, which are crucial elements in disrupting the chaotic patterns associated with disordered eating. Every part of the day is purposeful, offering multiple touchpoints for healing and personal growth.
Meal times are central to the inpatient experience, not only as a means of physical nourishment but as opportunities for therapeutic engagement. All meals and snacks are monitored by trained staff, who provide support, guidance, and intervention when anxiety or resistance arises. These supervised meals help reframe eating as a necessary and manageable part of life rather than a source of fear or control. Over time, patients begin to rebuild trust in their bodies and develop a more balanced relationship with food.
Therapy is woven throughout the day, often taking place in both individual and group settings. Patients explore topics such as body image, self-worth, coping strategies, and interpersonal relationships in a space designed to foster safety and openness. These sessions are not only about understanding the disorder but also about constructing a new identity separate from it. Through storytelling, role play, and skill-building exercises, patients start to reclaim autonomy and self-acceptance.
Medical care is ongoing and seamlessly integrated into the daily routine. Vital signs are regularly monitored, medications are administered as needed, and health education is provided to help patients understand the physical impacts of their eating behaviors. This medical oversight reassures both patients and their families that recovery is progressing safely and that any complications will be addressed promptly.
Daily life also includes moments of rest, reflection, and recreation. These aspects of care are vital for developing a sustainable lifestyle post-discharge. Activities like journaling, nature walks, or creative arts offer therapeutic value while reinforcing the idea that joy, pleasure, and relaxation are essential to well-being. The clinic environment thus becomes a microcosm for real life, allowing patients to practice recovery in a setting that mirrors the complexities and rewards of the outside world.
Transitioning from Inpatient Care to Independent Living
One of the most critical phases of recovery occurs not during inpatient care but immediately after discharge. Transitioning from the highly supportive environment of an inpatient eating disorder clinic to the relative independence of everyday life can be both empowering and daunting. The goal of discharge planning is to ensure that patients leave with a roadmap, a support system, and the coping tools necessary to maintain the gains achieved during treatment.
The discharge process typically begins well before the end of the inpatient stay. Clinical teams collaborate with patients to develop a comprehensive aftercare plan tailored to their individual needs. This may include referrals to outpatient therapists, dietitians, support groups, or partial hospitalization programs (PHP). By connecting patients with ongoing care, the transition becomes less abrupt and more manageable, reducing the likelihood of relapse.
Education plays a key role in post-inpatient success. Patients are equipped with knowledge about their condition, relapse warning signs, and self-care practices that support ongoing recovery. They learn how to navigate social situations involving food, manage stress, and advocate for their needs in personal and professional environments. These practical skills help bridge the gap between treatment and real life, empowering individuals to reclaim their autonomy without sacrificing their well-being.
Family and community involvement are also crucial. Many inpatient programs offer family therapy and education sessions to help loved ones understand the recovery process and learn how to provide appropriate support. When families are informed and involved, they become allies in the recovery journey, offering encouragement and accountability during vulnerable moments.
Moreover, many clinics offer alumni programs or follow-up check-ins to help former patients stay connected. These resources provide a safety net, reminding individuals that support remains available even after they leave the facility. The transition to independence is not the end of the journey but a continuation of it—an opportunity to apply what was learned in treatment to the unpredictable but ultimately rewarding landscape of everyday life.
Sustaining Long-Term Recovery Beyond Inpatient Treatment
While inpatient eating disorder treatment serves as a pivotal turning point, sustained recovery requires continued effort, support, and self-awareness. Long-term recovery involves more than just the absence of disordered behaviors; it signifies the development of a fulfilling life that is not dominated by thoughts of food, weight, or appearance. It requires cultivating resilience, embracing imperfection, and actively engaging in practices that nurture physical and emotional health.
One of the most effective ways to support long-term recovery is through consistent outpatient care. Regular therapy sessions, nutritional counseling, and medical check-ins help individuals stay grounded and accountable. These services reinforce the progress made in an inpatient setting and provide a safe space to process challenges as they arise. It’s not uncommon for individuals to continue outpatient treatment for months or even years following discharge, particularly during high-stress periods or life transitions.
Developing a support network is equally essential. Friends, family, peer groups, and mentors who understand the complexities of eating disorders can offer encouragement and guidance. Whether through formal support groups or informal relationships, staying connected with others reduces feelings of isolation and helps individuals stay focused on recovery goals. The presence of supportive, understanding people can make a significant difference during difficult moments.
Daily routines and self-care habits also contribute to sustained wellness. Establishing consistent eating patterns, engaging in joyful movement, getting adequate sleep, and setting healthy boundaries are all practices that reinforce stability. Many individuals find mindfulness and meditation helpful for managing anxiety and reconnecting with their bodies in a compassionate way. These habits act as protective factors, shielding against the internal and external stressors that can trigger relapse.
Finally, a mindset of growth and self-compassion is vital. Recovery is not linear, and setbacks do not equate to failure. Individuals who approach their journey with curiosity, flexibility, and kindness toward themselves are more likely to maintain long-term success. Inpatient eating disorder clinics lay the groundwork, but it is the ongoing commitment to healing—and the belief that a better life is possible—that sustains recovery over time.
Frequently Asked Questions (FAQ) About Inpatient Eating Disorder Clinics and Long-Term Recovery
What makes inpatient eating disorder treatment different from outpatient care?
The primary difference lies in the level of intensity and structure. Inpatient eating disorder treatment provides 24/7 care in a medically supervised environment, which is critical for individuals who are medically unstable or facing acute psychological distress. Unlike outpatient programs that allow patients to return home daily, inpatient care immerses individuals in a therapeutic setting where disordered behaviors can be closely monitored and interrupted. The structure of daily meals, constant emotional support, and access to multiple therapeutic modalities allows for a deeper, more focused recovery process. This high-touch model often yields faster stabilization and lays the groundwork for long-term change.
How long do patients typically stay in an inpatient eating disorder clinic?
The length of stay varies depending on the severity of the disorder and the patient’s response to treatment. Most inpatient eating disorder clinics recommend a stay of several weeks to a few months to ensure both medical stabilization and meaningful psychological progress. While short-term programs can initiate recovery, many patients benefit from longer stays to develop coping skills, process trauma, and build new thought patterns. Some clinics offer step-down programs to ease the transition into lower levels of care, which can help prevent relapse. Ultimately, duration is tailored to the individual’s unique medical and emotional needs.
Can patients continue their education or work responsibilities during treatment?
Most inpatient eating disorder clinics prioritize health and recovery above all else, so traditional work and academic responsibilities are often paused. However, some advanced programs do provide structured academic or vocational support, particularly for adolescents and young adults. Educational liaisons may help patients stay on track with schoolwork, while job coaching or remote access might be allowed in later stages of treatment for those further along in recovery. Still, participation is carefully managed to avoid stressors that could interfere with progress. The emphasis remains on full emotional and physical restoration before reintegrating complex responsibilities.
What kind of therapies are used beyond traditional talk therapy?
Inpatient eating disorder treatment goes far beyond standard talk therapy. Clinics often employ expressive therapies such as art, music, and movement therapy to help patients reconnect with their emotions and bodies in nonverbal ways. Somatic experiencing and trauma-informed yoga are increasingly used to address physiological responses tied to past trauma. Culinary therapy, where patients learn to prepare and interact with food in a controlled setting, also helps reshape dysfunctional eating patterns. These integrative approaches enrich recovery by addressing multiple dimensions of healing—physical, emotional, and spiritual.
Do inpatient eating disorder clinics accommodate diverse identities and needs?
Leading inpatient eating disorder clinics are increasingly striving to provide inclusive care that respects gender identity, cultural background, neurodiversity, and body diversity. Clinics now offer gender-affirming policies, bilingual staff, and culturally competent programming to better support a broader range of patients. Some facilities also specialize in treating marginalized communities who often face barriers to traditional treatment. This shift acknowledges that one-size-fits-all care is ineffective and that recovery must be tailored to reflect the patient’s lived experience. Representation and inclusion are now seen as essential aspects of ethical and effective treatment.
How are families involved during inpatient eating disorder treatment?
Family involvement is a crucial component of successful recovery, particularly for adolescents and young adults. In many inpatient eating disorder clinics, family-based therapy is offered to rebuild communication, address conflict, and teach supportive skills. Educational workshops help families understand the complexity of eating disorders and prepare them for post-discharge challenges. Even in adult programs, family or partner sessions may be incorporated to foster healthy relationship dynamics. When families are equipped with knowledge and compassion, they can become vital allies in relapse prevention and long-term healing.
Is it possible to relapse after inpatient eating disorder treatment, and what can reduce that risk?
Relapse is a recognized part of many recovery journeys, but it doesn’t indicate failure. The risk of relapse can be significantly reduced through structured aftercare plans, ongoing therapy, support groups, and consistent self-monitoring. Inpatient eating disorder clinics often prepare patients for discharge with detailed strategies that include relapse prevention skills, emotional regulation tools, and crisis planning. Continued connection to outpatient services and a strong support network also reinforce recovery efforts. Success hinges on viewing recovery as a lifelong process, not a fixed destination.
How do inpatient programs address co-occurring mental health issues?
Most eating disorder inpatient treatment programs are equipped to treat co-occurring conditions such as depression, anxiety disorders, PTSD, and substance abuse. These issues are not viewed as secondary but rather as interwoven threads in the fabric of the eating disorder itself. Psychiatrists and psychologists work in tandem to assess and treat these overlapping diagnoses through integrated care plans. Medications may be introduced or adjusted, and specialized therapies like trauma-focused CBT or EMDR are sometimes used. The goal is to heal the whole person—not just the symptoms related to food and body image.
What role does nutrition education play in inpatient eating disorder clinics?
Nutrition education is a cornerstone of inpatient eating disorder treatment, helping patients rebuild not just physical strength but also confidence in their relationship with food. Registered dietitians guide patients through meal planning, nutritional science, and food myth-busting sessions that demystify common fears. Education is delivered in a compassionate, non-judgmental way that encourages curiosity over shame. By understanding how nutrients affect energy, cognition, and mood, patients begin to make informed food choices grounded in self-care rather than fear. This empowers them to carry forward balanced eating patterns after discharge.
Are there innovations or future trends emerging in eating disorder inpatient treatment?
Yes, the field of inpatient eating disorder treatment is evolving with promising innovations. Virtual reality exposure therapy, for example, is being explored as a way to desensitize patients to anxiety-provoking situations like dining out. Genetic and neurobiological research is uncovering biomarkers that may eventually help personalize treatment approaches. More clinics are also incorporating mindfulness-based interventions and trauma-informed care models to improve outcomes. The future points toward increasingly individualized, tech-supported, and integrative care that adapts to each patient’s needs. As science and empathy continue to converge, inpatient eating disorder clinics are better equipped than ever to support long-term recovery.

Conclusion: How Inpatient Eating Disorder Clinics Build the Foundation for Lifelong Healing
Inpatient eating disorder clinics play a vital role in initiating recovery and preparing individuals for the complexities of life beyond treatment. These clinics offer a sanctuary where healing begins—not just of the body, but of the mind and spirit. By combining medical oversight with psychological support, nutritional rehabilitation, and therapeutic structure, inpatient eating disorder treatment provides a comprehensive foundation that addresses every facet of the disorder. It is an immersive, transformative experience that equips individuals with the tools, insights, and confidence needed to reclaim their lives.
Long after discharge, the impact of an inpatient eating disorder clinic continues to resonate. The skills learned, the connections formed, and the self-discoveries made during treatment all contribute to a more grounded, resilient recovery journey. When individuals leave these facilities, they do so with a deeper understanding of themselves and a renewed sense of hope. They are not cured in the traditional sense, but they are changed—stronger, more self-aware, and better prepared to live fully and freely.
For anyone considering eating disorder inpatient treatment, the path may seem daunting at first. But the potential for healing, growth, and transformation is real. With the right support, recovery is not just possible—it’s achievable, sustainable, and life-affirming. Whether you are seeking help for yourself or a loved one, know that inpatient care is a powerful step toward long-term recovery and a healthier, more fulfilling future.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.

