Introduction: The Liver’s Role in Detoxification and the Impact of Cirrhosis
The liver is one of the most vital organs responsible for maintaining homeostasis in the body. Its primary role in detoxification ensures that harmful substances, metabolic byproducts, and external toxins are neutralized and eliminated. However, when the liver undergoes pathological changes, such as those seen in cirrhosis, its ability to perform detoxification is significantly impaired. Understanding the pathophysiology of liver cirrhosis and how cirrhotic liver morphology influences detoxification is crucial in the prevention, management, and treatment of liver diseases. By exploring the complex mechanisms of liver damage, fibrosis, and functional decline, we can better comprehend the systemic consequences that result from hepatic dysfunction.
You may also like: The Best Liver Detox Supplements: How to Choose Safe and Effective Support for Your Liver
Liver cirrhosis is a progressive, chronic condition characterized by the replacement of healthy liver tissue with scar tissue, leading to a distortion of hepatic architecture. This fibrosis disrupts the normal structure and function of the liver, reducing its ability to filter toxins from the blood. The resulting accumulation of harmful substances, such as ammonia and bilirubin, leads to complications like hepatic encephalopathy, jaundice, and increased susceptibility to infections. As the disease advances, the cirrhotic liver loses its ability to regenerate and adapt, ultimately causing multi-organ failure in severe cases. Understanding the connection between cirrhotic liver morphology and detoxification impairment provides valuable insights into disease management and potential therapeutic interventions.
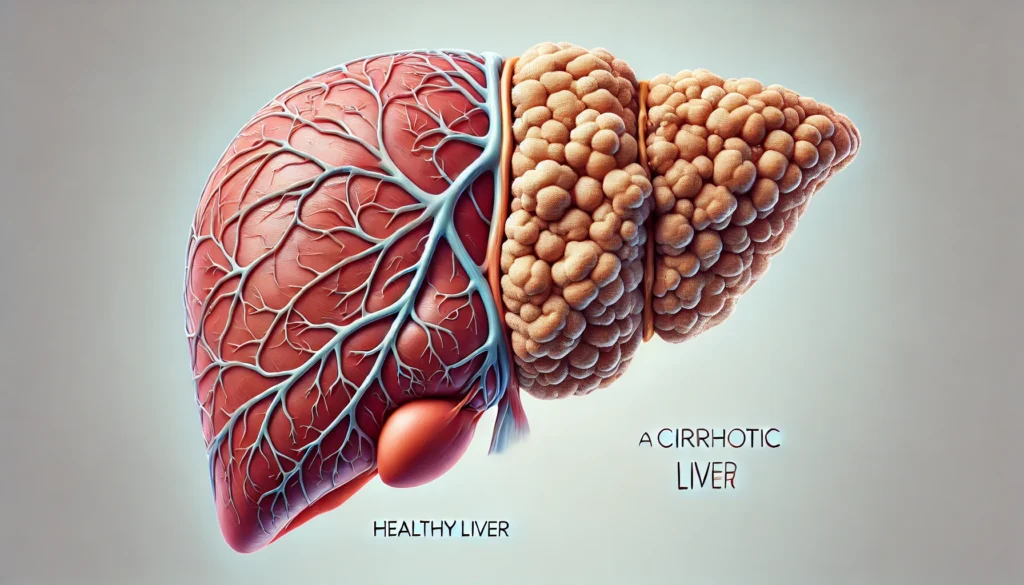
Structural Changes in Cirrhotic Liver Morphology
The healthy liver possesses a unique architectural framework that supports its diverse physiological functions. Hepatic lobules, the fundamental units of the liver, are composed of hepatocytes arranged in plates that radiate around a central vein. This structure allows for efficient blood flow through the hepatic sinusoids, enabling direct interaction between hepatocytes and the circulating blood. However, when cirrhosis develops, this orderly arrangement is disrupted due to excessive deposition of fibrous tissue, leading to the formation of regenerative nodules. These morphological changes have a profound impact on the liver’s ability to detoxify harmful substances.
Fibrosis results from chronic inflammation triggered by persistent liver injury, commonly caused by conditions such as viral hepatitis, chronic alcohol consumption, non-alcoholic fatty liver disease (NAFLD), and autoimmune disorders. In response to sustained hepatic injury, hepatic stellate cells become activated and produce excessive collagen and extracellular matrix proteins. Over time, these fibrotic changes lead to the narrowing of sinusoids, increased vascular resistance, and impaired hepatocyte function. The progressive accumulation of scar tissue further compromises blood flow, preventing the liver from effectively processing and eliminating toxins.
Another critical feature of cirrhotic liver morphology is the disruption of bile canaliculi and hepatic ducts. The impaired bile flow leads to cholestasis, a condition characterized by the buildup of bile acids and bilirubin in the liver. This dysfunction exacerbates the retention of toxic metabolites, contributing to complications such as jaundice, pruritus, and malabsorption of fat-soluble vitamins. The overall structural deterioration of the cirrhotic liver significantly impacts its detoxification capacity, leading to systemic toxicity and metabolic disturbances.
Impaired Detoxification Pathways in Cirrhosis
The liver utilizes three primary detoxification pathways: phase I, phase II, and phase III biotransformation. In a healthy liver, these pathways work in concert to neutralize toxins and facilitate their elimination. However, in the presence of cirrhotic liver morphology, these pathways become severely impaired, leading to toxin accumulation and increased susceptibility to systemic toxicity.
Phase I detoxification, primarily mediated by cytochrome P450 enzymes, involves the oxidation, reduction, and hydrolysis of lipophilic toxins to make them more water-soluble. However, in cirrhosis, the expression and activity of cytochrome P450 enzymes are significantly reduced, leading to decreased metabolism of drugs, environmental toxins, and endogenous waste products. This reduction in enzymatic activity contributes to prolonged drug half-lives, increased drug toxicity, and heightened sensitivity to medications.
Phase II detoxification involves conjugation reactions, where the liver attaches molecules such as glucuronic acid, sulfate, and glutathione to toxins, rendering them more hydrophilic for excretion. In cirrhotic livers, the impairment of conjugation pathways leads to ineffective clearance of bilirubin, resulting in jaundice. Additionally, glutathione depletion exacerbates oxidative stress, further accelerating liver damage and dysfunction.
Phase III detoxification refers to the active transport of conjugated toxins out of hepatocytes into bile or urine. This process relies on ATP-binding cassette (ABC) transporters, which are frequently downregulated in cirrhosis. The resulting decrease in biliary excretion contributes to the accumulation of toxins within the liver, leading to increased systemic toxicity. Collectively, these impairments in detoxification pathways underscore the profound impact of cirrhotic liver morphology on hepatic function and overall health.
Consequences of Detoxification Impairment in Cirrhosis
The inability of the cirrhotic liver to effectively detoxify substances leads to multiple systemic complications, the most significant being hepatic encephalopathy, jaundice, and drug toxicity. Hepatic encephalopathy arises from the accumulation of neurotoxic substances, particularly ammonia, in the bloodstream. In a healthy liver, ammonia is converted to urea via the urea cycle and excreted through the kidneys. However, in cirrhosis, impaired urea cycle function leads to hyperammonemia, which crosses the blood-brain barrier and disrupts neurotransmission, causing cognitive dysfunction, confusion, and, in severe cases, coma.
Jaundice, another hallmark of liver dysfunction, results from the liver’s inability to conjugate and excrete bilirubin. As unconjugated bilirubin accumulates in the bloodstream, it deposits in tissues, leading to the characteristic yellowing of the skin and sclera. This condition not only affects appearance but also indicates a significant decline in liver function.
Patients with cirrhosis also experience heightened drug sensitivity due to impaired metabolism and clearance. Medications that require hepatic metabolism, such as benzodiazepines, opioids, and nonsteroidal anti-inflammatory drugs (NSAIDs), can accumulate to toxic levels, increasing the risk of adverse effects. Physicians must carefully adjust drug dosages and monitor for signs of toxicity in individuals with cirrhosis.
Strategies for Managing Detoxification Impairment in Cirrhosis
While cirrhosis is irreversible, several strategies can help mitigate the impact of impaired detoxification. Lifestyle modifications, including alcohol cessation, a balanced diet rich in antioxidants, and weight management, play a crucial role in preserving liver function. Pharmacological interventions, such as lactulose and rifaximin, can reduce ammonia levels and prevent hepatic encephalopathy. Additionally, emerging therapies, including antifibrotic agents and regenerative medicine approaches, offer potential hope for slowing disease progression.
Liver transplantation remains the definitive treatment for end-stage cirrhosis, restoring normal hepatic architecture and detoxification capacity. Advances in transplantation techniques and immunosuppressive therapy have significantly improved outcomes for patients undergoing liver transplantation.

Frequently Asked Questions (FAQ) on Cirrhotic Liver Morphology and the Pathophysiology of Liver Cirrhosis
1. How does cirrhotic liver morphology impact overall liver function? Cirrhotic liver morphology significantly alters the liver’s architecture, leading to compromised blood flow and impaired function. As the liver develops fibrosis, normal hepatocytes are replaced with scar tissue, obstructing essential processes such as detoxification, metabolism, and protein synthesis. These structural changes also contribute to portal hypertension, which can cause complications like varices and ascites. Over time, reduced liver function impacts nutrient absorption, immune response, and toxin clearance. Understanding the pathophysiology of liver cirrhosis is crucial for managing and mitigating these long-term effects.
2. What are the early signs that the liver is undergoing cirrhotic changes? The early signs of cirrhotic liver morphology often go unnoticed because the liver compensates well until significant damage occurs. However, symptoms such as persistent fatigue, unexplained weight loss, and mild jaundice can be early indicators. Patients may also experience easy bruising due to impaired clotting factor production and swelling in the lower extremities from fluid retention. Laboratory findings often show elevated liver enzymes before symptoms become apparent. Early detection through regular health screenings can help slow the progression by addressing underlying causes and implementing lifestyle changes.
3. How does the pathophysiology of liver cirrhosis lead to complications like hepatic encephalopathy? The pathophysiology of liver cirrhosis disrupts ammonia metabolism, leading to hepatic encephalopathy, a condition characterized by cognitive impairment. When the liver fails to detoxify ammonia and other neurotoxic substances, they accumulate in the bloodstream and affect brain function. Symptoms range from mild confusion and forgetfulness to severe disorientation and coma in advanced cases. Managing dietary protein intake and using medications such as lactulose can help reduce ammonia levels. Regular monitoring of cirrhotic liver morphology through imaging and blood tests is essential to prevent severe complications.
4. Can cirrhosis-related liver damage be reversed? While cirrhosis itself is generally irreversible, early intervention can halt or slow its progression. Lifestyle modifications, such as eliminating alcohol, maintaining a balanced diet, and managing underlying conditions like hepatitis B or C, can prevent further damage. Some medications and regenerative therapies are being researched for their potential to promote liver cell regeneration. In cases where cirrhotic liver morphology has led to significant scarring, a liver transplant may be the only option. Understanding the pathophysiology of liver cirrhosis can help patients and healthcare providers make informed treatment decisions.
5. What role does nutrition play in managing cirrhosis? Proper nutrition is crucial in managing the effects of cirrhotic liver morphology. A diet rich in lean protein, whole grains, and antioxidants supports liver function and prevents muscle wasting. Sodium intake should be restricted to minimize fluid retention and the risk of ascites. Patients with cirrhosis often require vitamin and mineral supplementation due to malabsorption issues. Avoiding alcohol and processed foods helps reduce additional liver stress. Understanding the nutritional needs of a cirrhotic liver can significantly improve quality of life and long-term health outcomes.
6. How is cirrh medical terminology relevant for understanding liver cirrhosis? Cirr medical terminology provides essential insights into the diagnosis, staging, and management of cirrhosis. Terms such as “fibrosis,” “portal hypertension,” and “hepatic decompensation” describe key aspects of disease progression. Understanding these terms helps patients communicate effectively with healthcare providers and grasp the implications of their condition. Medical imaging reports often describe cirrhotic liver morphology in detail, making familiarity with relevant terminology beneficial. Patients who understand cirr medical terminology are better equipped to participate in their treatment plans and advocate for their health.
7. What are the best diagnostic tools for assessing cirrhotic liver morphology? A combination of imaging techniques and blood tests is used to assess cirrhotic liver morphology. Ultrasound elastography measures liver stiffness, helping to determine the extent of fibrosis. MRI and CT scans provide detailed views of liver structure and blood flow. Liver biopsy remains the gold standard for confirming cirrhosis and grading fibrosis severity. Additionally, blood tests measuring liver enzymes, bilirubin, and albumin levels provide biochemical indicators of liver function. Early and accurate diagnosis is essential for managing the pathophysiology of liver cirrhosis effectively.
8. Why does cirrhosis increase the risk of liver cancer? Cirrhotic liver morphology creates an environment conducive to the development of hepatocellular carcinoma (HCC), the most common type of liver cancer. Chronic inflammation and fibrosis promote genetic mutations in liver cells, increasing the likelihood of malignant transformation. The pathophysiology of liver cirrhosis involves altered blood flow, which can limit the liver’s ability to filter harmful substances, further contributing to cancer risk. Regular screening with imaging and alpha-fetoprotein (AFP) tests helps detect liver cancer at an early, treatable stage. Patients with cirrhosis should undergo periodic evaluations to mitigate this risk.
9. How does cirrh medical terminology help differentiate between compensated and decompensated cirrhosis? Cirr medical terminology is essential in distinguishing between compensated and decompensated cirrhosis. Compensated cirrhosis means the liver is still functioning well despite fibrosis, and patients may have minimal or no symptoms. Decompensated cirrhosis is marked by complications such as ascites, variceal bleeding, and hepatic encephalopathy. Understanding these terms is crucial for determining prognosis and treatment options. Patients diagnosed with decompensated cirrhosis often require more intensive medical management and closer monitoring.
10. What are future treatment prospects for cirrhosis? Research into liver regeneration and antifibrotic therapies offers hope for patients with cirrhotic liver morphology. Scientists are exploring stem cell therapies and gene-editing techniques to promote liver repair. New medications targeting fibrosis pathways aim to halt or even reverse some aspects of the pathophysiology of liver cirrhosis. Advances in artificial liver support systems may provide temporary relief for patients awaiting transplantation. As medical technology evolves, the potential for improved outcomes in cirrhosis treatment continues to expand.

Conclusion: The Critical Link Between Cirrhotic Morphology and Detoxification
The pathophysiology of liver cirrhosis underscores the intricate relationship between hepatic morphology and detoxification. Structural changes in cirrhotic liver morphology profoundly impair the liver’s ability to metabolize and eliminate toxins, leading to severe systemic consequences. Understanding these pathophysiological mechanisms is essential for developing effective treatment strategies and improving patient outcomes. As research continues to explore novel therapies, the goal remains to preserve liver function, prevent complications, and ultimately enhance the quality of life for individuals affected by cirrhosis.
chronic liver disease, hepatic fibrosis, liver detoxification process, bile acid metabolism, hepatic encephalopathy management, non-alcoholic fatty liver disease progression, oxidative stress in cirrhosis, ammonia metabolism dysfunction, drug metabolism in liver disease, jaundice and bilirubin processing, hepatocyte function decline, cytochrome P450 enzyme impairment, cirrhosis and systemic toxicity, regenerative medicine for liver disease, liver transplantation outcomes, fibrosis and hepatic sinusoids, portal hypertension complications, stellate cell activation in fibrosis, phase I and II liver detoxification, urea cycle dysfunction in cirrhosis
Further Reading:
Influence of biliary cirrhosis on the detoxification and elimination of a food derived carcinogen
Silymarin for Treating Toxic Liver Disease: International Consensus Recommendations
The exposome and liver disease – how environmental factors affect liver health
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.