Understanding how to care for your digestive health begins with recognizing the role food plays in healing—or harming—your stomach lining. For individuals experiencing gastritis, a condition marked by inflammation of the stomach’s mucosal layer, dietary changes offer a profound path to relief. A well-structured gastritis diet helps to minimize triggers, reduce discomfort, and promote long-term healing. The connection between diet and gastritis is not merely anecdotal but grounded in clinical research showing how specific foods influence gastric acid production, inflammation, and mucosal regeneration.
The inflammation stomach diet approach is more than avoiding spicy food or acidic beverages. It encompasses a wide array of holistic practices designed to protect the gastrointestinal lining, enhance microbial diversity, and support anti-inflammatory pathways. Whether your gastritis stems from H. pylori infection, stress, NSAID use, or autoimmune processes, your diet can either perpetuate the irritation or become your most powerful ally in healing. This article explores both sides of the nutritional coin—what to eat and what to avoid—with medical accuracy, holistic insight, and practical recommendations that align with a modern, gut-conscious lifestyle.
You may also like: The Ultimate Guide to Gut Healthy Meals: Best Meals for Gut Health and Nourishing Recipes You’ll Love
How the Gastritis Diet Supports Gut Healing and Reduces Inflammation
The therapeutic power of a targeted gastritis diet lies in its capacity to shield the stomach lining from further insult while simultaneously enhancing its ability to heal. Chronic inflammation in the gastrointestinal tract can lead to complications such as ulcers, intestinal permeability, or even malabsorption of nutrients. A key goal in managing this condition is to reduce the presence of pro inflammatory foods that aggravate symptoms and delay recovery.
Foods that contribute to inflammation include refined sugars, processed meats, and hydrogenated oils. But beyond avoiding these known offenders, the diet should proactively include soothing, nutrient-rich alternatives. For instance, fermented foods such as kefir or yogurt can supply the gut with beneficial bacteria that enhance mucosal defense. Meanwhile, anti-inflammatory herbs like ginger and turmeric have been shown in various studies to help reduce gastric irritation and support mucosal healing.
Importantly, the gastritis diet is not one-size-fits-all. While some individuals thrive on soft, low-fiber foods during flare-ups, others may tolerate a broader range of cooked vegetables or whole grains. However, certain universal truths remain: reducing acidity, avoiding alcohol, and eating smaller, more frequent meals can drastically improve digestive outcomes. Transitioning to this diet requires mindfulness, but the rewards—reduced pain, normalized digestion, and improved nutrient absorption—are well worth the effort.
Best Foods for Gastritis: What to Eat for Soothing Relief
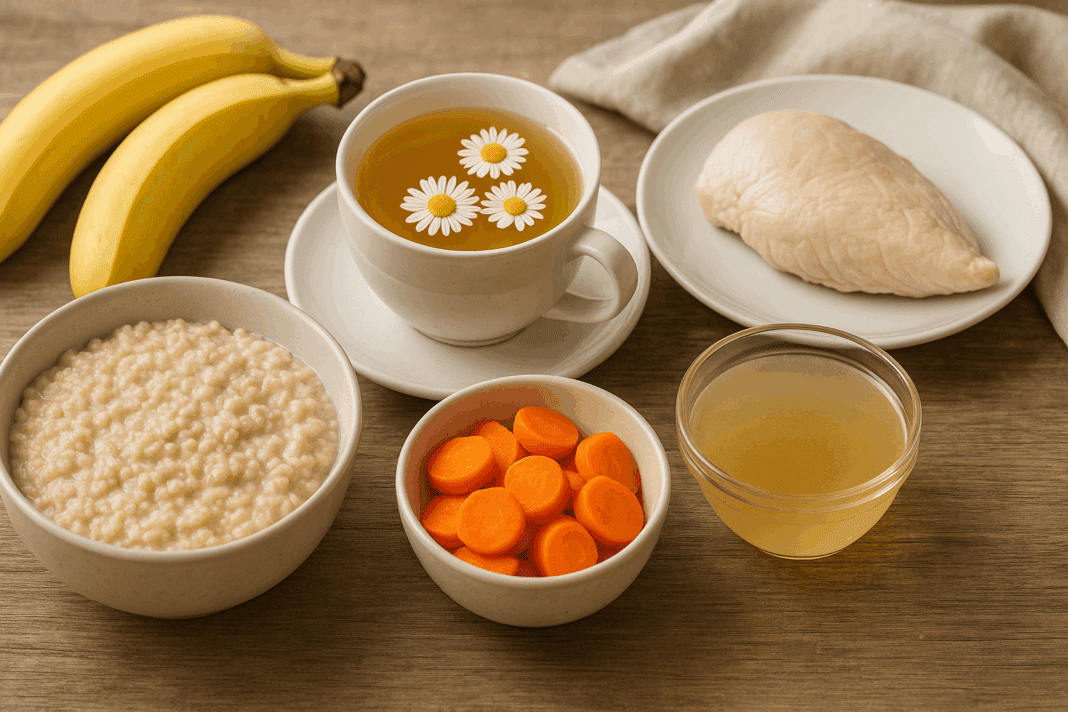
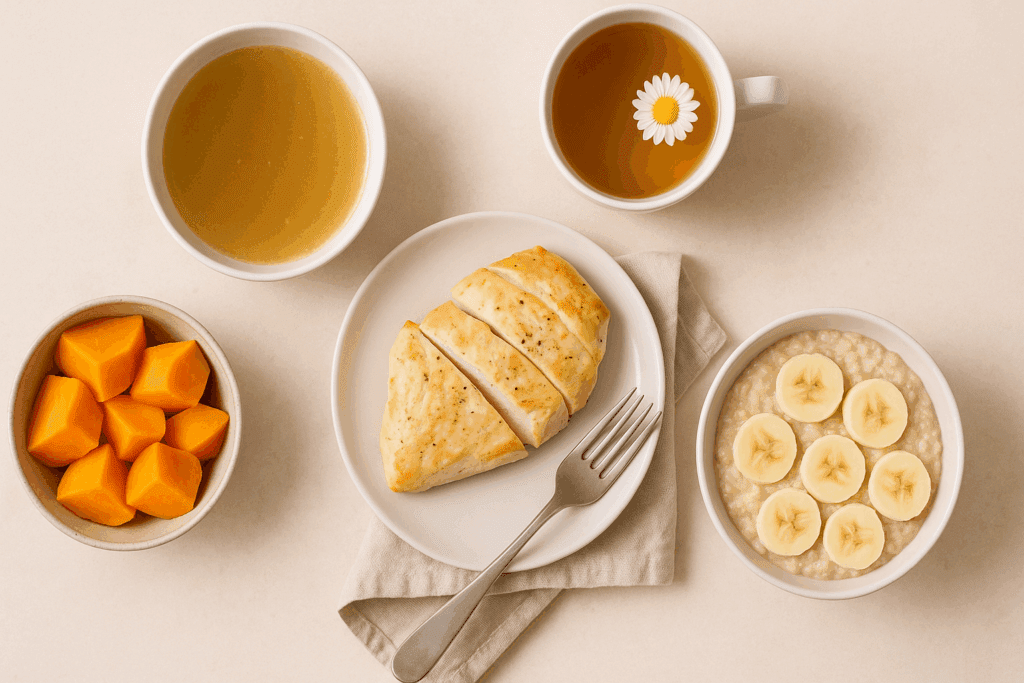
Knowing what to eat with gastritis can transform your experience from chronic discomfort to daily relief. Some of the best foods for gastritis include easy-to-digest grains, steamed or boiled vegetables, lean proteins, and gut-healing broths. Oatmeal, for example, is rich in soluble fiber and creates a protective coating along the stomach lining, making it an ideal breakfast option. It also supports an inflammation stomach diet when paired with anti-inflammatory fruits like bananas or blueberries.
When considering proteins, lean poultry such as skinless chicken or turkey is preferable, provided it is baked or steamed without irritants like pepper or vinegar. For vegetarians, well-cooked legumes like lentils can be tolerated when introduced slowly. Bone broth is another excellent choice due to its high collagen content, which supports the repair of gastrointestinal tissues. Incorporating small amounts of healthy fats from sources like avocados or flaxseed oil can aid nutrient absorption without overwhelming the stomach.
In addition to whole foods, certain beverages also play a role in symptom management. The best morning drink for gastritis might be warm chamomile tea, which has mild antispasmodic effects and can soothe the gut when consumed on an empty stomach. Aloe vera juice, in its purified form, may also be effective in coating the lining and reducing acidity. Ultimately, your food for gastritis should reflect a balance between nourishment, digestibility, and therapeutic potential.
The Role of Gastritis-Friendly Vegetables in Mucosal Healing
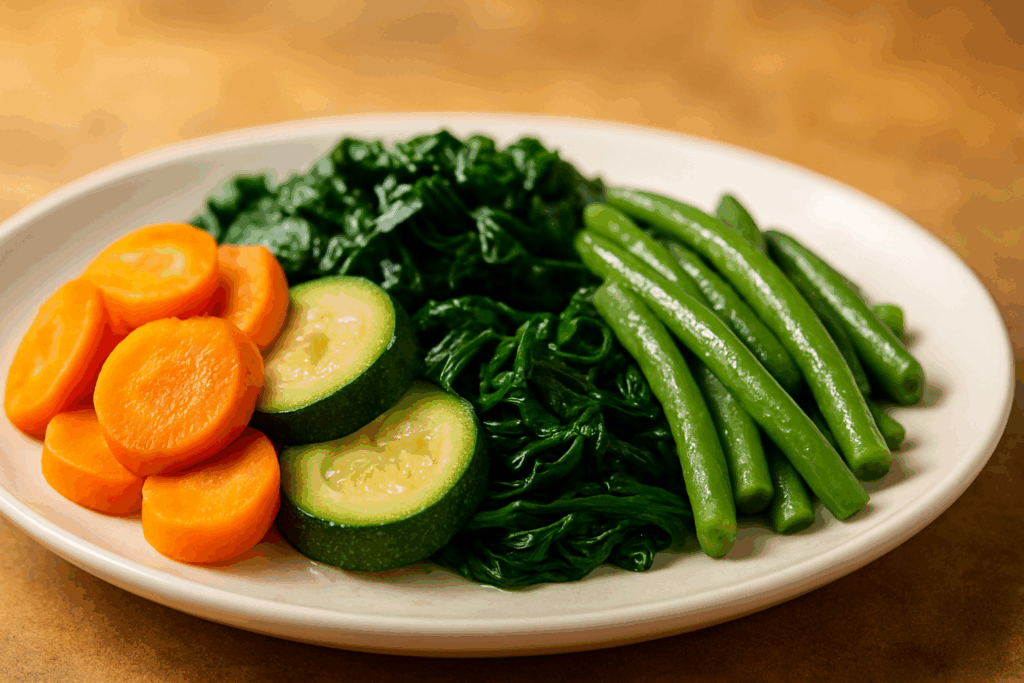
Vegetables are a critical component of a gastritis diet, provided that selections are made with care. Gastritis friendly vegetables are those that are low in acid, easily digestible, and unlikely to ferment excessively in the stomach. Cooked carrots, zucchini, spinach, sweet potatoes, and green beans are excellent choices because they provide antioxidants, vitamins, and fiber without irritating the stomach lining. These vegetables can be steamed, boiled, or pureed to enhance digestibility and maximize nutrient availability.
However, not all vegetables are equal when it comes to inflammation. Veggies that cause inflammation often include those in the cruciferous family, such as broccoli, cauliflower, and cabbage, which produce gas and can aggravate bloating and pain during a gastritis flare-up. Nightshades like tomatoes and peppers, though nutritious, are acidic and may increase gastric irritation in sensitive individuals. It’s crucial to understand your body’s tolerance and introduce vegetables gradually while monitoring symptoms.
Why is pasta with spinach good for acute gastroenteritis? One reason is that spinach, when cooked, becomes soft and alkaline-forming, while plain pasta provides a bland carbohydrate source that is gentle on the gut. Together, they form a mild, nourishing meal that can be particularly useful during periods of acute inflammation or recovery from gastrointestinal distress. Knowing how to combine ingredients is just as important as choosing the right ones, and this understanding elevates your diet from basic sustenance to a therapeutic protocol.

Frequently Asked Questions About the Gastritis Diet and Inflammation Relief
What are some overlooked triggers in a gastritis diet that people commonly miss?
While most individuals are aware of the usual irritants such as spicy foods or coffee, many fail to consider the impact of temperature extremes in beverages and meals. Extremely hot or cold items can provoke the gastric lining and exacerbate discomfort. Additionally, artificial sweeteners, especially those found in sugar-free gums and diet sodas, may disrupt the gut microbiota and stimulate acid production. Another overlooked category is dried fruits, which, due to their concentrated sugar and acidity, can silently contribute to gastric irritation. A well-managed gastritis diet should not only focus on food types but also food preparation and consumption habits.
How does chronic stress affect the efficacy of an inflammation stomach diet?
Chronic stress plays a profound role in reducing the effectiveness of even the best-formulated inflammation stomach diet. Cortisol, the body’s primary stress hormone, can increase gastric acid secretion and suppress mucosal blood flow, impairing the stomach’s natural defenses. Stress also alters gut motility and increases intestinal permeability, potentially undoing the benefits of a carefully curated gastritis meal plan. Techniques such as mindful eating, meditation, and cognitive behavioral therapy can be critical adjuncts to diet. Integrating stress management with dietary changes offers a more holistic and sustainable approach to gastritis relief.
Can chicken cause inflammation in individuals following a gastritis diet?
While lean chicken is often considered a safe protein in a gastritis diet, the method of preparation significantly affects its impact on the stomach. Grilled or baked chicken seasoned simply with herbs is generally well tolerated, but fried or heavily spiced chicken may become problematic. Furthermore, certain individuals might react to preservatives or additives commonly found in processed poultry products. For those with sensitivities, even seemingly benign meats can become culprits in triggering inflammation. Carefully sourcing organic, minimally processed chicken and observing your body’s response remains essential.
Why is rice considered one of the best foods for gastritis recovery?
Rice is particularly gentle on the digestive system, making it a staple in nearly every diet for gastric problem management. It is low in fat, naturally gluten-free, and easy to digest, making it ideal for those with inflamed stomachs. Brown rice adds an additional layer of benefit by providing fiber that helps regulate digestion, though it should be introduced cautiously during acute flare-ups. For many, the answer to “is rice good for inflamed stomach” is a resounding yes, especially when paired with steamed vegetables or broth. This simple food often provides a soothing base during the healing process.
Could sausage cause inflammation even if consumed occasionally?
Yes, even occasional consumption of sausage could cause inflammation, particularly in individuals with sensitive stomachs or a history of gastritis. Sausages are typically high in saturated fats, sodium, and nitrates—ingredients known to trigger inflammation in the gut and joints. While some varieties may appear healthier, such as those labeled “organic” or “grass-fed,” they often still contain problematic spices and preservatives. Moreover, processed meats rank high among the foods that contribute to inflammation and are best limited or avoided entirely in an effective gastritis diet plan. If you’re seeking alternatives, consider lean fish or steamed lentils as more stomach-friendly protein sources.
What role do gastritis friendly vegetables play in preventing relapses?
Gastritis friendly vegetables like zucchini, spinach, and carrots offer vital nutrients while minimizing mechanical or chemical irritation to the stomach. These vegetables are rich in anti-inflammatory compounds, fiber, and antioxidants that support tissue repair and immune function. They also help maintain microbial diversity in the gut, a crucial factor in preventing gastritis recurrence. Unlike raw or cruciferous vegetables, which may act as veggies that cause inflammation for some, these options are typically well tolerated when cooked thoroughly. Including a rotation of these vegetables in your gastritis meal plan promotes dietary variety without risking digestive upset.
What to eat when you have gastritis but also suffer from joint inflammation?
When managing both gastritis and joint inflammation, one must be particularly vigilant about avoiding foods that cause inflammation in joints and the gastrointestinal lining. Incorporating omega-3 rich foods like chia seeds or flax oil can help address both concerns simultaneously. Soft-cooked greens, skinless poultry, and low-acid fruits like melons and pears serve as excellent examples of food for gastritis and joint health. It’s equally important to limit pro inflammatory foods like refined carbohydrates and processed meats, which exacerbate both conditions. A targeted gastritis diet plan that supports systemic anti-inflammation can yield holistic improvements.
What is the long-term benefit of following a strict gastritis diet plan?
Sticking to a gastritis diet plan over time offers profound benefits that go beyond immediate symptom control. Long-term adherence helps rebuild the gastric mucosa, reduce dependency on medications like PPIs, and support a more resilient gut microbiome. It may also protect against secondary conditions such as ulcers or esophageal inflammation. A consistent anti-inflammatory regimen based on foods good for gastritis reduces the likelihood of flare-ups and enhances overall digestive efficiency. The key lies in consistency, dietary diversity, and mindful eating habits that adapt as your digestive health evolves.
Are there vegetables that cause inflammation even when cooked?
Yes, while cooking typically reduces the inflammatory potential of many vegetables, some still act as vegetables that cause inflammation due to individual sensitivity or underlying conditions. Eggplant, tomatoes, and peppers are part of the nightshade family and are known to trigger inflammation in some people, especially those with autoimmune conditions. Even when cooked, these can still pose risks if you’re particularly susceptible to food-based triggers. Including only well-tested, gastritis friendly vegetables in your diet while carefully tracking symptoms can help isolate the culprits. Personalized observation remains one of the most effective tools in tailoring a diet for gastric problem relief.
How do I build a sustainable lifestyle around the gastritis diet?
Building a lifestyle around the gastritis diet requires strategic planning, flexibility, and a willingness to reevaluate habits over time. Begin with structured meal planning and batch cooking using foods to eat to avoid gastritis symptoms. Cultivate mindful eating routines such as chewing thoroughly, eating slowly, and stopping before full satiety to prevent gastric overload. Incorporate stress-relief practices like yoga or journaling to reduce the physiological triggers of stomach irritation. Over time, these strategies coalesce into a sustainable way of life that reduces dependency on medication and fosters a deeper connection with your body’s needs.

Avoiding Inflammatory Triggers: What to Avoid for Gastritis Relief
Equally important as knowing what to eat is understanding what to avoid for gastritis management. The list of foods to avoid with gastritis is long and varied, but certain themes stand out: acidity, spice, fat, and processing. Highly acidic foods such as citrus fruits, tomatoes, and vinegar-based condiments can exacerbate inflammation by stimulating excessive gastric acid production. Likewise, spicy ingredients including chili powder, black pepper, and hot sauces are known to trigger symptoms in many gastritis sufferers.
Processed meats are another major offender. Not only do they often contain nitrates and preservatives, but many are also high in saturated fats and sodium, which can damage the gastric mucosa. A common question is: could sausage cause inflammation? The answer is yes—especially when it is fatty, seasoned, and chemically preserved. Sausage and similar deli products should be minimized or eliminated entirely from a gastritis-conscious diet.
Alcohol, caffeine, and carbonated beverages also rank high on the list of things to avoid. These drinks can strip the stomach of its protective mucus and lead to increased acid exposure. Even seemingly benign items like chocolate or peppermint can cause problems due to their effect on the lower esophageal sphincter, which may worsen reflux in those with concurrent GERD. Understanding which foods cause inflammation in joints and gut tissues is central to developing an effective gastritis meal plan that is both preventative and restorative.
Further Reading:
What to Eat and What to Avoid If You Have Gastritis