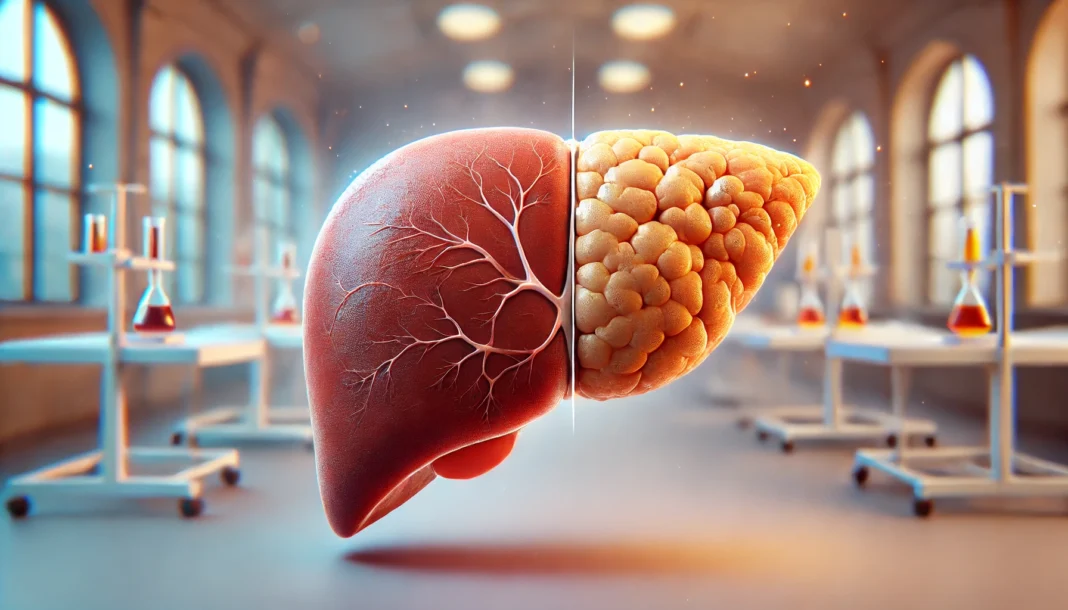
Fatty liver disease, also known as hepatic steatosis, is a condition that occurs when excessive fat accumulates in liver cells. This condition can be benign in its early stages but may progress to more severe liver diseases, such as nonalcoholic steatohepatitis (NASH), fibrosis, cirrhosis, or even liver failure. Understanding fatty liver disease lab results is crucial in diagnosing the severity of the condition, monitoring progression, and determining the best course of treatment. Blood tests play a pivotal role in assessing liver function and detecting potential damage, helping healthcare providers and patients make informed decisions about lifestyle changes and medical interventions.
You may also like: The Best Liver Detox Supplements: How to Choose Safe and Effective Support for Your Liver
The Importance of Liver Function Tests in Diagnosing Fatty Liver Disease
Liver function tests (LFTs) are a series of blood tests that evaluate the health of the liver by measuring various enzymes, proteins, and substances. These tests help determine how well the liver is performing its normal functions, including detoxification, protein production, and bile secretion. Elevated liver enzyme levels often indicate liver inflammation or damage, which may be associated with hepatic steatosis. By interpreting these test results, healthcare providers can assess the extent of liver impairment and guide patients toward appropriate lifestyle modifications or treatments.
One of the primary liver enzymes measured in LFTs is alanine aminotransferase (ALT). This enzyme is primarily found in the liver and is released into the bloodstream when liver cells are damaged. Elevated ALT levels can suggest fatty liver disease, but they are not specific to the condition, as they may also rise in cases of hepatitis, medication-induced liver injury, or other metabolic disorders. Aspartate aminotransferase (AST) is another enzyme that, when elevated, can indicate liver damage. The AST-to-ALT ratio is often used to differentiate between fatty liver disease and more severe liver conditions such as alcoholic liver disease.
In addition to ALT and AST, alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) are other enzymes commonly included in liver function tests. While these enzymes may be elevated in individuals with fatty liver disease, they are more commonly associated with bile duct obstruction or cholestasis. Understanding the significance of each enzyme level within the broader context of a patient’s symptoms and medical history is essential for accurate diagnosis and effective management of hepatic steatosis.
What Blood Test Indicates Fatty Liver?
Several blood tests can provide insight into fatty liver disease, but no single test can definitively diagnose the condition. Instead, a combination of blood markers and imaging studies is used to assess liver health. One of the most commonly used indicators of fatty liver is the presence of elevated liver enzymes, particularly ALT and AST, as discussed earlier. However, these enzymes alone do not confirm fatty liver disease, as they may also be elevated due to other liver conditions.
The presence of insulin resistance is another significant factor in fatty liver disease. Since hepatic steatosis is closely linked to metabolic syndrome, measuring fasting blood glucose and hemoglobin A1c levels can provide insight into a patient’s risk of developing type 2 diabetes, which often coexists with fatty liver disease. Elevated triglycerides and low-density lipoprotein (LDL) cholesterol levels also serve as markers of metabolic dysfunction, reinforcing the need for a comprehensive lipid panel when evaluating fatty liver risk.
Furthermore, blood tests measuring inflammatory markers such as C-reactive protein (CRP) and ferritin levels can help assess the presence of inflammation and oxidative stress in the liver. Elevated ferritin levels may suggest liver inflammation and can sometimes indicate the progression of fatty liver disease to nonalcoholic steatohepatitis (NASH), a more severe form of hepatic steatosis characterized by liver inflammation and fibrosis. Understanding these lab markers allows healthcare professionals to determine the likelihood of disease progression and recommend targeted interventions.
The Role of Fibrosis Markers in Assessing Liver Damage
As fatty liver disease progresses, liver fibrosis—the formation of scar tissue—can develop, leading to a decline in liver function. Blood tests that evaluate fibrosis markers help determine the severity of liver scarring and assess the risk of complications such as cirrhosis. One commonly used fibrosis marker is the Fibrosis-4 (FIB-4) index, which calculates the degree of liver fibrosis based on age, platelet count, AST, and ALT levels. A higher FIB-4 score suggests more advanced liver fibrosis and may warrant further imaging or liver biopsy.
Another important marker is the Enhanced Liver Fibrosis (ELF) test, which measures specific proteins associated with liver fibrosis. This test provides a noninvasive means of assessing the likelihood of significant liver scarring, allowing for earlier intervention. The AST-to-platelet ratio index (APRI) is another commonly used formula that estimates liver fibrosis based on AST levels and platelet count. Low platelet levels are often associated with advanced fibrosis, making APRI a valuable tool in monitoring disease progression.
Patients with fatty liver disease should also be tested for serum albumin and prothrombin time, which help assess the liver’s ability to produce essential proteins and clotting factors. A decline in albumin levels or prolonged prothrombin time may indicate significant liver dysfunction, necessitating closer medical supervision. By combining these fibrosis markers with other liver function tests, healthcare providers can gain a comprehensive understanding of a patient’s liver health and determine appropriate treatment strategies.

Frequently Asked Questions (FAQ) About Fatty Liver Disease Lab Results
1. What are the most common lab tests used to diagnose fatty liver disease?
Several blood tests can help detect fatty liver disease, but no single test provides a definitive diagnosis. Physicians often look at a combination of fatty liver disease labs, including liver enzyme tests like ALT (alanine aminotransferase) and AST (aspartate aminotransferase), which may be elevated in liver conditions. Additionally, tests for alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) help assess liver function. A lipid panel can indicate abnormal cholesterol levels often associated with hepatic steatosis. Further specialized tests, such as the FibroTest or imaging like FibroScan, may be recommended to evaluate liver fibrosis or advanced liver disease.
2. What blood test indicates fatty liver disease most reliably?
While no single blood test can diagnose fatty liver disease on its own, ALT and AST levels are often the first indicators of liver dysfunction. Elevated ALT is particularly significant because it is more specific to liver-related damage than AST, which can also rise due to muscle conditions. However, some individuals with fatty liver disease may have normal ALT and AST levels, making additional tests necessary. Physicians also check for metabolic markers such as fasting glucose and insulin resistance, which can contribute to liver fat accumulation. To confirm the diagnosis, hepatic steatosis labs may include imaging tests like an ultrasound or MRI to visually assess fat deposits in the liver.
3. Can normal fatty liver disease lab results still indicate an issue?
Yes, it is possible to have normal fatty liver disease lab results while still having fat accumulation in the liver. Some individuals with hepatic steatosis do not experience significant liver enzyme elevations, especially in early stages. This is why additional testing, including imaging studies such as an abdominal ultrasound or MRI, is often recommended for those at risk. Other markers like elevated triglycerides, insulin resistance, or inflammation-related indicators such as C-reactive protein (CRP) can still suggest metabolic dysfunction affecting the liver. Regular follow-ups and lifestyle modifications are essential, even in the absence of abnormal blood test results.
4. What is the significance of ALT and AST ratios in fatty liver disease?
The ratio of ALT to AST can provide clues about the underlying cause of liver enzyme elevations. In non-alcoholic fatty liver disease (NAFLD), ALT is typically higher than AST, while in alcoholic liver disease, the opposite is often true. A high AST-to-ALT ratio (greater than 2:1) may suggest alcohol-related damage or advanced fibrosis. However, fatty liver disease labs should be interpreted in conjunction with other clinical findings, such as imaging results and metabolic risk factors. If AST levels are significantly higher than ALT, further investigation for liver fibrosis or cirrhosis may be warranted.
5. What role do triglycerides and cholesterol play in hepatic steatosis labs?
High triglycerides and abnormal cholesterol levels are closely linked to fatty liver disease. When excess fats accumulate in the liver, it often coincides with dyslipidemia, characterized by elevated triglycerides and low HDL (good cholesterol). A lipid panel is a crucial component of fatty liver disease labs because it provides insight into metabolic health and cardiovascular risk. Managing cholesterol and triglyceride levels through diet, exercise, and medication (if necessary) can help prevent the progression of fatty liver disease. Doctors may also monitor non-HDL cholesterol as a better predictor of fatty liver-related complications.
6. How does insulin resistance impact fatty liver disease lab results?
Insulin resistance is a key driver of fatty liver disease and can influence various lab markers. When the body becomes resistant to insulin, it leads to increased fat storage in the liver and higher fasting glucose levels. Many patients with hepatic steatosis labs show elevated fasting insulin and HOMA-IR (homeostatic model assessment of insulin resistance), a calculation used to assess insulin sensitivity. Elevated hemoglobin A1c (HbA1c) can also indicate prediabetes or diabetes, which often coexist with fatty liver disease. Addressing insulin resistance through diet and exercise is one of the most effective strategies for reversing fatty liver.
7. Can elevated liver enzymes mean something other than fatty liver disease?
Yes, while elevated liver enzymes are common in fatty liver disease labs, they can also indicate other conditions. Viral hepatitis (such as Hepatitis B or C), autoimmune liver diseases, medication-induced liver injury, and genetic disorders like hemochromatosis can all lead to increased ALT and AST levels. Doctors typically conduct additional tests, including hepatitis panels, autoimmune markers, and iron studies, to rule out other causes. If liver enzymes remain persistently high without a clear cause, a liver biopsy may be necessary to assess the extent of damage.
8. What additional tests can help confirm fatty liver disease beyond blood work?
Blood tests provide valuable insights, but imaging techniques are often necessary to confirm hepatic steatosis. An abdominal ultrasound is a widely used, non-invasive test that can detect liver fat accumulation. More advanced imaging, such as MRI-based proton density fat fraction (MRI-PDFF) or transient elastography (FibroScan), can provide a more precise assessment of fat content and liver stiffness, which helps evaluate fibrosis risk. In some cases, a liver biopsy is required for definitive diagnosis, particularly if there is concern about inflammation or advanced fibrosis.
9. How can I improve my fatty liver disease lab results?
Improving fatty liver disease lab results requires a comprehensive approach to lifestyle changes. Weight loss is one of the most effective interventions, as even a 5-10% reduction in body weight can significantly decrease liver fat. A diet rich in whole foods, including lean proteins, vegetables, and healthy fats, while reducing sugar and processed carbohydrates, is beneficial. Regular exercise, particularly resistance training and aerobic workouts, helps improve insulin sensitivity and reduce liver fat. Additionally, limiting alcohol intake and avoiding unnecessary medications that stress the liver can further support liver health.
10. How often should I monitor my hepatic steatosis labs if I have fatty liver disease?
The frequency of monitoring hepatic steatosis labs depends on the severity of the condition and individual risk factors. For those with mild fatty liver disease and no signs of fibrosis, annual testing of liver enzymes, lipid panels, and metabolic markers may be sufficient. However, individuals with elevated liver enzymes, obesity, or diabetes should have more frequent follow-ups every 3-6 months. If fibrosis or liver scarring is suspected, imaging tests such as FibroScan or MRI may be recommended periodically. Ongoing monitoring is essential to track disease progression and ensure lifestyle interventions are effectively improving liver health.
Conclusion: Understanding Lab Results for Better Liver Health Management
Interpreting fatty liver disease lab results requires a thorough understanding of liver function tests, metabolic markers, and fibrosis indicators. Blood tests such as ALT, AST, fasting blood glucose, lipid panels, and inflammatory markers provide crucial insights into liver health, allowing for early detection and targeted interventions. Additionally, fibrosis markers such as FIB-4, ELF, and APRI help assess disease progression and guide clinical decision-making.
Managing fatty liver disease involves a multifaceted approach that includes dietary modifications, regular exercise, weight management, and, in some cases, medical treatment. Understanding lab results empowers patients to take proactive steps toward liver health, enabling them to make informed lifestyle choices and work collaboratively with healthcare providers. As research continues to advance, more precise diagnostic tools and therapeutic options will further enhance the ability to detect, monitor, and manage fatty liver disease effectively.
fatty liver symptoms and diagnosis, liver enzyme tests, liver function blood tests, nonalcoholic fatty liver disease, NAFLD lab markers, metabolic syndrome and liver health, liver fibrosis assessment, ALT and AST levels, inflammatory markers in liver disease, lipid profile and fatty liver, cirrhosis risk assessment, insulin resistance and hepatic steatosis, early detection of liver disease, lifestyle changes for fatty liver, medical management of fatty liver disease, liver biopsy alternatives, noninvasive liver fibrosis tests, triglycerides and liver health, cholesterol and fatty liver, understanding liver health markers, hepatic steatosis progression
Further Reading:
Diagnosis and Evaluation of Nonalcoholic Fatty Liver Disease
Non-alcoholic fatty liver disease: pathophysiological concepts and treatment options
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.