Depression is a multifaceted mental health condition that affects millions of individuals around the world. While its emotional and psychological symptoms are often emphasized, physical manifestations such as changes in appetite are equally significant but sometimes overlooked. Experiencing depression and not eating regularly can severely impact physical health, nutritional balance, and overall quality of life. The interplay between depression and appetite disturbances reflects the deeply interconnected nature of the mind and body. For individuals navigating the challenges of depression, mindful eating presents a compassionate and practical approach to supporting nutritional wellness without adding pressure or judgment.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
The Link Between Depression and Loss of Appetite
Appetite changes are among the most common physical symptoms of depressive disorders. While some individuals may experience increased cravings and emotional eating, others encounter the opposite: a marked decrease in appetite, known clinically as anorexia or hyporexia depending on severity. Depression no appetite scenarios are not simply a matter of preference or choice but are rooted in complex neurochemical and physiological disruptions. Serotonin and dopamine, neurotransmitters closely associated with mood regulation, also play essential roles in hunger and satiety signaling. When these chemical messengers become imbalanced due to depression, it can lead to a diminished desire for food and a disconnection from bodily hunger cues.
Beyond the biological mechanisms, the emotional toll of depression can dull motivation, interest, and energy. Activities that once brought pleasure—including eating—may feel burdensome or entirely unappealing. For some, the process of meal preparation becomes overwhelming, leading to skipped meals or reliance on processed convenience foods that lack nutritional value. The experience of depression and loss of appetite is further compounded by fatigue, negative self-talk, and distorted thoughts around self-worth, which can inhibit self-care behaviors, including maintaining proper nourishment. This creates a vicious cycle where malnutrition exacerbates fatigue and cognitive fog, further deepening depressive symptoms.

Recognizing Signs of Nutritional Decline During Depression
Identifying when depression is negatively impacting nutrition can be challenging, especially since symptoms may develop gradually. However, there are critical signs that signal when the body is not receiving the nutrients it needs. Significant weight loss without intention, reduced muscle tone, brittle hair and nails, dry skin, and persistent fatigue are physical manifestations of undernutrition. From a cognitive and emotional standpoint, worsened concentration, irritability, increased anxiety, and heightened sensitivity to stress may also result from inadequate dietary intake.
The phrase “depression and not eating” often captures a profound internal struggle. A person may feel emotionally numb, yet physically weak—caught between the desire to feel better and the absence of appetite to support recovery. It’s important to differentiate between typical fluctuations in appetite and chronic patterns that indicate an underlying issue. When depression loss appetite symptoms persist for weeks or begin interfering with daily function, professional support becomes essential. A licensed therapist or physician can assess whether nutritional concerns are contributing to the severity of depressive symptoms and offer guidance for addressing both physical and psychological needs simultaneously.

The Role of Mindful Eating in Depression Recovery
Mindful eating is a non-judgmental approach that encourages individuals to become more aware of their food-related experiences without pressure or criticism. Unlike restrictive diets or rigid meal plans, mindful eating emphasizes presence, curiosity, and self-compassion. For those navigating depression and loss of appetite, mindful eating offers a gentle way to reconnect with internal cues and reestablish a nourishing relationship with food. This practice does not demand sudden or drastic changes but instead invites individuals to tune into sensations of hunger and fullness, notice the flavors and textures of food, and explore emotional associations with eating.
Research supports the use of mindful eating interventions as part of integrative mental health care. Studies have shown that mindfulness practices can reduce depressive symptoms, promote emotional regulation, and improve self-efficacy related to health behaviors. Through consistent practice, individuals may begin to notice small but meaningful shifts—such as feeling more inclined to eat breakfast, preparing a favorite comfort dish, or recognizing the satisfaction that comes from a nourishing meal. These small steps, when repeated with intention and kindness, contribute to long-term healing and emotional resilience.
Practical Strategies for Eating When You Don’t Feel Like It
One of the most challenging aspects of depression no appetite scenarios is finding the motivation to eat when there is no physical or emotional desire to do so. In these moments, it’s essential to adopt practical, manageable strategies that honor both your mental state and your body’s nutritional needs. Starting with small, nutrient-dense meals or snacks can reduce the pressure of eating a full plate. Smoothies, soups, yogurt with granola, and nut butter on whole grain toast offer comforting, easy-to-digest options that provide energy without overwhelming the senses.
Setting gentle routines around eating can also help rebuild appetite. While depression may disrupt daily structure, introducing small rituals—such as sitting by a window while eating, using your favorite bowl, or lighting a candle at mealtime—can create positive associations and a sense of calm. Visual reminders or phone alarms may encourage consistency without judgment. Partnering with a supportive friend, therapist, or nutritionist can add a layer of accountability and reduce feelings of isolation. For those who feel overwhelmed by grocery shopping or cooking, meal delivery services or simple meal prep ideas can alleviate some of the cognitive load.
Nutritional Considerations and Key Nutrients for Mood Support
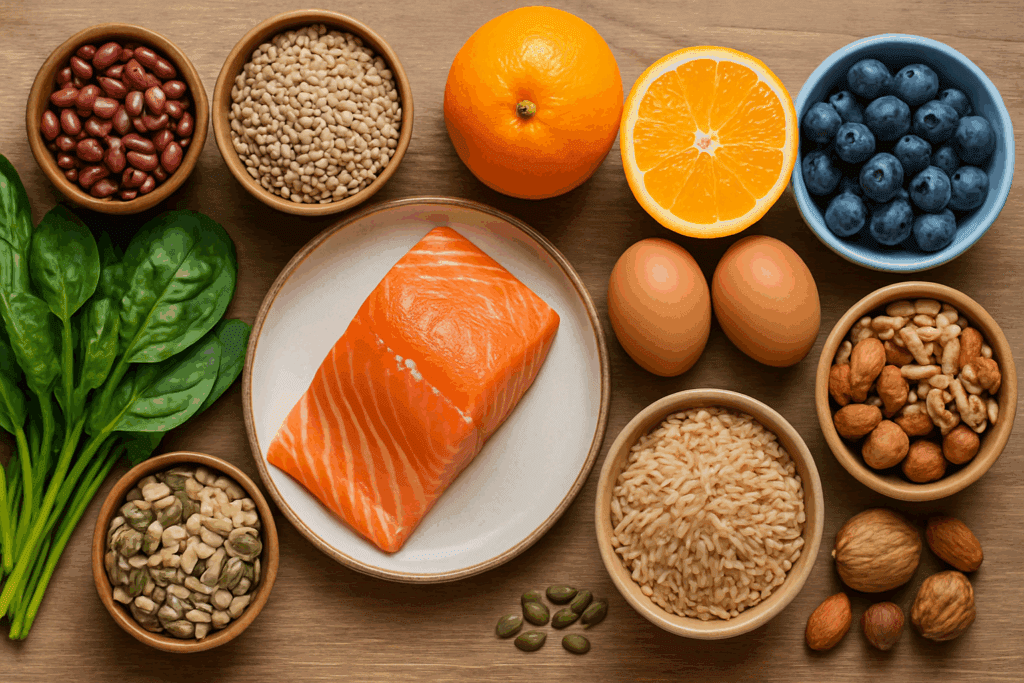
When navigating depression and not eating, it’s important to ensure that the food consumed delivers meaningful nutritional value. Even in small amounts, certain nutrients play critical roles in supporting brain health, mood regulation, and energy levels. Omega-3 fatty acids, found in fatty fish like salmon or plant-based sources such as flaxseeds and walnuts, have anti-inflammatory properties that support cognitive function and emotional balance. B vitamins, particularly B6, B9 (folate), and B12, are essential for neurotransmitter synthesis and nervous system function.
Iron, zinc, and magnesium also contribute to mood stability and can be found in foods like legumes, lean meats, seeds, and leafy greens. Protein, whether from animal or plant sources, is necessary for repairing tissues and maintaining muscle mass—especially important for those experiencing depression loss appetite over extended periods. Including a colorful variety of fruits and vegetables can provide antioxidants that reduce oxidative stress, which is often elevated in individuals with chronic mental health conditions. Hydration should not be overlooked either, as even mild dehydration can impair concentration and mood.
The Emotional Dimensions of Eating During Depression
Eating is not merely a biological necessity; it is an emotionally rich experience shaped by memories, culture, relationships, and self-perception. When depression interferes with this connection, food can evoke complex feelings—guilt for not eating enough, shame for needing support, or frustration over lack of appetite. These emotional layers must be acknowledged with compassion rather than criticism. The phrase “depression and not eating” often reflects an internal dialogue that is fraught with self-judgment and fear. By reframing the act of eating as an act of self-care rather than a chore, individuals can begin to heal both physically and emotionally.
Practicing self-kindness in moments of struggle is vital. Instead of berating oneself for skipping a meal, it may be more helpful to ask, “What would nourish me right now, in this moment?” This might lead to sipping warm tea, nibbling on a comforting snack, or simply preparing something for later. The goal is not perfection but presence—honoring the body’s signals, however subtle, and choosing to respond with care. Mindful eating invites this gentle reorientation, offering a space where food becomes a pathway to connection rather than another source of stress.
Mindful Eating and the Power of Sensory Engagement
Depression can blunt sensory experiences, making food taste bland or unappealing. Mindful eating can counter this by encouraging intentional engagement with the senses. Taking a moment to observe the colors of a meal, inhale its aroma, feel its texture, and listen to the sounds of chewing or cooking can reawaken sensory pleasure. This may seem like a small or insignificant step, but over time, it can rekindle appreciation for food and stimulate appetite.
Creating a soothing eating environment also supports sensory engagement. Soft lighting, calming music, and a clean, uncluttered space can reduce external stress and make meals feel more inviting. Eating without distractions—such as turning off the television or putting away your phone—can deepen the experience and foster a sense of calm. These small acts of intentionality transform mealtimes from mechanical routines into opportunities for grounding and emotional nourishment.

When to Seek Professional Support for Depression and Nutrition
While mindful eating and self-care practices offer meaningful support, they are not substitutes for professional treatment. If depression no appetite symptoms persist or worsen despite your best efforts, it is crucial to seek guidance from a qualified healthcare provider. A mental health professional can assess the severity of your symptoms and recommend therapeutic interventions such as cognitive-behavioral therapy (CBT), medication, or other evidence-based approaches. A registered dietitian or integrative nutritionist can help design a personalized eating plan that accommodates your emotional and physical needs without adding stress.
In some cases, a coordinated care approach may be necessary. This might involve collaboration between your primary care physician, therapist, and nutrition specialist to ensure all aspects of your well-being are addressed. If weight loss becomes severe or nutrient deficiencies are suspected, laboratory testing may be recommended. Timely intervention can prevent complications and pave the way for more effective recovery. Remember that seeking help is a sign of strength, not failure. You do not need to navigate depression and loss of appetite alone.
Restoring Your Relationship with Food and Body
Recovery from depression is not linear, and neither is the journey to rebuilding a healthy relationship with food. There may be setbacks, days when eating feels like a monumental task, or moments of progress that feel fleeting. These fluctuations are part of the process and do not indicate failure. Over time, consistent practices like mindful eating, compassionate self-reflection, and supportive dialogue can help restore a sense of trust in one’s body and instincts.
Engaging in creative food-related activities—such as gardening, visiting a farmers’ market, or exploring new recipes—can also reignite curiosity and enjoyment around food. These activities provide a sense of agency and connection, reminding individuals that food is not just fuel but also a source of pleasure, tradition, and expression. By embracing food as a partner in healing rather than a battleground, individuals living with depression can rediscover moments of joy and vitality even in the midst of emotional difficulty.
Frequently Asked Questions: Depression and Appetite
What are some long-term risks associated with chronic under-eating due to depression?
Chronic under-eating tied to depression can result in more than just short-term fatigue or malnutrition. Over time, consistent nutrient deprivation may impair immune function, increase the risk of anemia, and even lead to hormonal imbalances that affect reproductive and thyroid health. For individuals experiencing depression and not eating consistently for weeks or months, bone density may begin to decrease due to calcium and vitamin D deficiencies, raising the risk of fractures and osteoporosis. Additionally, prolonged undernutrition can alter gut microbiota diversity, which has been increasingly linked to mood regulation and cognitive clarity. These long-term complications demonstrate how deeply depression no appetite patterns can influence overall physiological resilience.
Can social support help improve appetite during depressive episodes?
Yes, social interaction can play a critical role in encouraging consistent eating behaviors during depressive episodes. Sharing meals with a trusted friend or family member can help reduce the isolation that often accompanies depression and loss of appetite. Even casual conversations during mealtimes may help shift the focus away from internal distress and toward connection, making the act of eating feel less mechanical and more emotionally fulfilling. Support systems also provide gentle accountability, such as checking in with reminders or offering to assist with grocery shopping or food preparation. This kind of external motivation can often initiate changes that feel impossible to achieve alone, especially when depression and not eating have become deeply intertwined.
Are there specific therapeutic interventions focused on appetite recovery in depression?
Several therapeutic modalities can support appetite recovery for those struggling with depression no appetite symptoms. Cognitive-behavioral therapy (CBT) is particularly effective in addressing negative thought patterns that discourage self-care, including eating. Interpersonal therapy (IPT) may be useful when appetite disruptions are tied to grief or relationship stressors. More specialized options, such as behavioral activation therapy, include practical steps to increase daily functioning and routine building—including meal routines. Emerging interventions like nutritional psychiatry and integrative therapy also blend talk therapy with dietary guidance to address the dual impact of depression and loss of appetite. These approaches work best when personalized to an individual’s unique emotional and physiological profile.
How can sensory stimulation help reawaken appetite in depression?
Sensory desensitization is a common experience for people dealing with depression and loss of appetite, where food seems bland, unappealing, or even nauseating. Reintroducing sensory pleasure can be a surprisingly effective way to rekindle interest in eating. Warm, aromatic spices like cinnamon, cardamom, or ginger can stimulate olfactory pathways and enhance food appeal. Visual presentation—such as colorful fruits and vibrant dishes—can also subtly encourage appetite by invoking visual pleasure. Playing soft music, eating with textured utensils, or using scented candles may seem trivial, but such sensory engagement helps counter the emotional flatness often associated with depression and not eating.
Can certain eating patterns worsen depressive symptoms if not managed properly?
Yes, irregular or highly restrictive eating patterns can significantly worsen mood symptoms. Skipping meals or consuming nutritionally empty foods may cause blood sugar fluctuations, which can lead to irritability, fatigue, and difficulty concentrating—all of which intensify depressive states. In people experiencing depression no appetite tendencies, even mild hypoglycemia can mimic anxiety or exacerbate emotional volatility. Intermittent fasting, while popular in wellness circles, can be risky for individuals with a history of depression and not eating consistently, especially if the practice becomes rigid or obsessive. Eating at regular intervals, even in small amounts, helps stabilize mood and support neurological function over time.
Is loss of appetite in depression more common in certain age groups?
Research suggests that appetite loss in depression manifests differently across age groups, influenced by developmental, hormonal, and psychosocial factors. Teenagers and young adults may experience depression no appetite patterns due to peer pressure, body image issues, or academic stress, while older adults often face appetite changes linked to loneliness, grief, or underlying medical conditions. In elderly populations, depression and not eating regularly can be especially dangerous due to increased vulnerability to nutrient deficiencies and decreased muscle mass. Regardless of age, understanding the unique drivers of appetite loss is key to providing targeted interventions. Family dynamics, cultural expectations, and life transitions all influence how depression loss appetite symptoms are expressed and experienced.
Are there any natural supplements that can support appetite during depression?
Some natural supplements have shown promise in improving appetite and mood in people experiencing depression. Adaptogens like ashwagandha and rhodiola are often used to manage stress-related appetite disruptions, while omega-3 fatty acids—particularly EPA and DHA—are known to support both brain health and appetite regulation. Zinc and vitamin B-complex supplements can be helpful as well, especially when depression and loss of appetite are accompanied by fatigue or cognitive fog. However, it is crucial to consult with a healthcare provider before starting any new supplement, especially if the individual is taking antidepressants or has underlying health conditions. Supplements may enhance—but should never replace—medical and psychological care for depression and not eating.
How does sleep affect appetite in individuals with depression?
Sleep quality and appetite are closely linked, especially in individuals with depression. Disrupted sleep can disturb the hormones ghrelin and leptin, which regulate hunger and fullness. For someone already dealing with depression no appetite symptoms, poor sleep may further suppress hunger cues or impair judgment around food choices. Conversely, sleep deprivation can also lead to increased cravings for high-calorie, high-sugar foods, which may not support long-term recovery. Establishing a consistent sleep routine and addressing insomnia or hypersomnia—both common in depression—can indirectly improve appetite regulation and nutritional consistency.
Can mindfulness-based eating practices be adapted for people with severe appetite loss?
Yes, mindfulness-based eating can be tailored to meet the needs of individuals facing severe appetite challenges. Instead of beginning with full meals, the practice might start with one mindful bite or sip—bringing awareness to texture, temperature, and internal reactions without judgment. Over time, these micro-moments can reintroduce a sense of control and curiosity around food, even for those with persistent depression and not eating patterns. Some therapists recommend combining mindfulness with journaling to track subtle sensations and progress. These strategies help foster self-compassion and reduce the shame that often accompanies depression loss appetite struggles.
What role do cultural beliefs play in how we manage appetite loss during depression?
Cultural attitudes toward food and mental health significantly influence how people interpret and respond to depression and loss of appetite. In some cultures, food is a primary expression of care and community, so not eating may be perceived as a sign of disrespect or detachment, potentially worsening feelings of guilt or alienation. In others, stoicism and emotional suppression are valued, making it harder to discuss appetite changes openly. These dynamics can complicate diagnosis and support. Recognizing cultural nuances allows practitioners and caregivers to approach depression no appetite concerns with greater empathy and contextual awareness, offering support that aligns with the individual’s identity and values.
Reclaiming Wellness Through Gentle Nutrition and Mindful Awareness
Depression and not eating may seem like an inescapable pairing, but through intentional practices and compassionate support, it is possible to break this cycle. Mindful eating does not demand perfection or discipline but rather encourages gentle awareness and respect for the body’s needs. By approaching nutrition as an act of self-care rather than obligation, individuals can begin to heal both physiologically and emotionally. Supporting the body with nutrient-dense foods, honoring internal hunger cues, and creating positive associations with eating all contribute to improved mood, energy, and overall wellness.
As the journey unfolds, patience and kindness are essential. Healing from depression and loss of appetite requires a multifaceted approach that includes emotional support, medical guidance, and nourishing practices. Each step taken in the direction of mindfulness, no matter how small, is a powerful declaration of self-worth. Through this integrated path, individuals can restore not only their appetite but also their connection to life, vitality, and hope.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Food and mood: how do diet and nutrition affect mental wellbeing?

