In the complex landscape of mental health, certain conditions are more intertwined than many might initially assume. One of the most poignant intersections exists between depression and eating disorders, particularly anorexia nervosa. These co-occurring disorders often coexist in a deeply enmeshed cycle that affects both the mind and body. For readers navigating their own experiences or supporting a loved one, understanding the relationship between these mental health challenges—and how nutrition can play a pivotal role in healing—is not only essential but potentially life-changing.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
Mental health professionals have long recognized that eating disorders are not merely about food. At their core, they often stem from emotional pain, internalized stress, and the need for control when everything else feels unpredictable. Anorexia, defined by self-imposed food restriction and an intense fear of weight gain, frequently emerges alongside depression. But why is this link so common? And more importantly, how can a holistic view of nutrition contribute to recovery when both conditions are present?
Recognizing the Link Between Depression and Anorexia
To begin unraveling the connection between depression and eating disorders, it’s essential to understand how each condition presents itself. Depression is characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in daily activities. Anorexia nervosa, on the other hand, manifests through extreme dietary restriction, body image distortion, and a fear of gaining weight. Despite their differing surface symptoms, both disorders share deep psychological underpinnings, including low self-worth, perfectionism, and a desire for control.
The question often arises: can depression coexist with anorexia? Clinically, the answer is a resounding yes. Research indicates that up to 50-75% of individuals with anorexia also experience symptoms of depression. This comorbidity can complicate both diagnosis and treatment, as the two conditions often feed into one another. For instance, the malnutrition resulting from anorexia can exacerbate depressive symptoms by depleting essential neurotransmitters that regulate mood. Likewise, untreated depression can intensify restrictive eating behaviors as a misguided form of coping.
Understanding that depression and eating disorders often go hand in hand helps pave the way for more targeted interventions. When a person suffers from both, it becomes crucial to address each condition simultaneously, rather than viewing them in isolation. A purely nutritional intervention might fall short if the emotional triggers remain unexamined, just as talk therapy may have limited impact if physical health is rapidly declining.
The Role of Brain Chemistry and Malnutrition
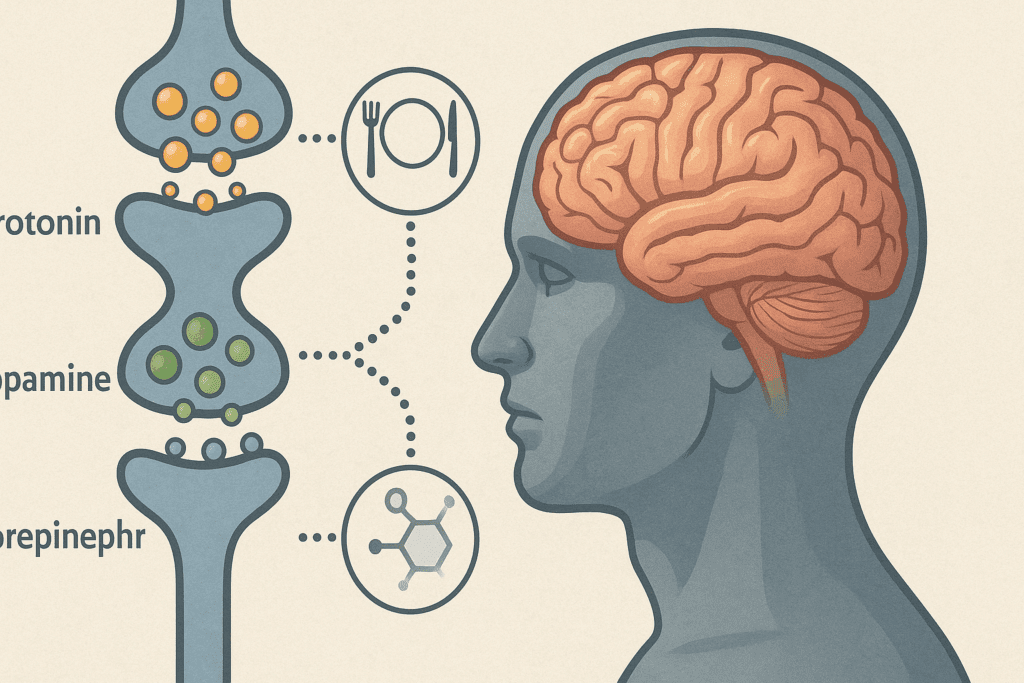
The biological interplay between depression and anorexia offers important insights into their coexistence. Both disorders impact neurotransmitter function, particularly involving serotonin, dopamine, and norepinephrine—chemicals that regulate mood, appetite, and energy. When the brain is deprived of the nutrients it needs to produce these neurotransmitters, mood regulation can suffer dramatically. This disruption may explain why those with anorexia frequently report feelings of emptiness, fatigue, and emotional numbness.
Malnutrition is not merely a consequence of anorexia; it is a driver of worsening mental health. The restriction of calories, particularly carbohydrates and fats, impairs the body’s ability to maintain hormonal balance and cognitive function. Over time, this nutritional deficiency creates a biochemical environment that fosters depressive symptoms. In a tragic feedback loop, the more the person restricts their intake, the worse they feel—emotionally, mentally, and physically.
This understanding underscores the importance of nutritional rehabilitation as an integral component of treatment. Reintroducing essential nutrients, often under the guidance of a registered dietitian specializing in eating disorders, can help stabilize brain chemistry and improve emotional resilience. Nutritional support, when combined with psychological therapy, can interrupt the cycle that keeps both anorexia and depression in place.

Emotional Triggers and Psychological Patterns
Beyond biology, the psychological dimensions of these coexisting disorders warrant close examination. Individuals struggling with depression and eating disorders often grapple with similar emotional challenges: intense self-criticism, guilt, shame, and an internalized sense of not being “good enough.” These feelings frequently stem from early life experiences such as trauma, neglect, or chronic stress, which shape one’s beliefs about self-worth and control.
Perfectionism is another hallmark shared by both conditions. Many individuals with anorexia also exhibit high-achieving, perfectionistic tendencies. When they fall short of self-imposed standards, depressive thoughts can flood in, reinforcing a cycle of self-punishment and restriction. The eating disorder becomes a tool for exerting control over one area of life when everything else feels unmanageable.
Therapeutic approaches such as Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) are particularly effective in addressing these psychological patterns. These therapies help individuals identify distorted thought processes and replace them with more adaptive beliefs. When applied in the context of both depression and anorexia, they provide a framework for healing that honors the interconnected nature of mind and body.
Family and Social Influences
It’s impossible to discuss depression and eating disorders without acknowledging the profound role of family and social dynamics. Societal pressures around body image, success, and productivity can create an environment where restrictive eating behaviors are not only tolerated but sometimes even rewarded. In families where appearance is highly valued or emotional expression is discouraged, individuals may learn to suppress their feelings and focus instead on controlling food intake as a way to cope.
Additionally, the stigma surrounding both mental illness and eating disorders can prevent people from seeking help. They may fear judgment, misunderstanding, or rejection. This social isolation only deepens depressive symptoms and reinforces disordered eating patterns. For this reason, education and open conversations are crucial. When communities are equipped with accurate information about these conditions, they can offer more compassionate and informed support.
Family-based therapy, particularly for adolescents, has shown promising results in treating co-occurring anorexia and depression. In this approach, parents and caregivers are empowered to play an active role in their child’s nutritional and emotional recovery. While family therapy may not be the right fit for everyone, involving loved ones in the treatment process can foster connection and reduce the sense of isolation that often accompanies these disorders.
Nutrition as a Foundational Pillar of Recovery
While psychotherapy addresses the emotional roots of eating disorders and depression, nutrition serves as the physiological foundation upon which recovery is built. Replenishing the body with essential macronutrients and micronutrients helps restore not only physical health but also cognitive function and emotional regulation. For example, omega-3 fatty acids, B vitamins, iron, and zinc all play critical roles in supporting mood stability and brain health.
The refeeding process must be handled with care, particularly in individuals with severe anorexia, to avoid refeeding syndrome—a potentially life-threatening shift in fluids and electrolytes. Thus, nutritional rehabilitation is best conducted in collaboration with a multidisciplinary team, including physicians, registered dietitians, and therapists. Together, they can craft a recovery plan that meets the individual’s unique needs and preferences.
It’s important to dispel the myth that nutrition alone can “cure” anorexia or depression. However, when used alongside therapeutic interventions, proper nutrition becomes a powerful ally in the healing process. Over time, as the body regains strength and balance, individuals are often better equipped to engage in therapy, process difficult emotions, and rebuild their sense of self.

The Power of Mindful Eating Practices
Mindful eating—an approach rooted in attentiveness and non-judgment—has emerged as a valuable tool in treating depression and eating disorders. Unlike restrictive diets or rigid meal plans, mindful eating encourages individuals to tune into their body’s cues, explore their relationship with food, and foster a sense of compassion toward themselves. This shift in perspective can be profoundly healing for those whose eating habits have been shaped by self-criticism and fear.
Incorporating mindfulness into meals involves slowing down, appreciating the sensory experience of food, and noticing hunger and fullness signals. Over time, this practice can help disrupt automatic behaviors, such as bingeing or restricting, and replace them with intentional choices. For individuals with depression, mindful eating may also serve as a grounding ritual that brings awareness to the present moment—offering a temporary reprieve from ruminative thoughts.
Nutritionists and therapists trained in mindfulness-based approaches can guide clients through exercises that foster self-awareness and emotional regulation. These practices are particularly effective when integrated into a larger recovery framework, reinforcing both psychological insight and nutritional stability. By learning to eat mindfully, individuals not only nourish their bodies but also cultivate a deeper connection with themselves.
Barriers to Treatment and the Importance of Early Intervention
Despite increased awareness, many people with depression and eating disorders remain undiagnosed or untreated. Stigma, lack of access to care, and cultural misconceptions continue to pose significant barriers. For instance, anorexia is still often associated solely with young, white, affluent women—overlooking the fact that it affects people of all genders, races, and socioeconomic backgrounds. Similarly, depression is frequently minimized or dismissed as a phase rather than recognized as a legitimate medical condition.
Early intervention significantly improves outcomes for both conditions. When treatment begins before the disorders become deeply entrenched, individuals are more likely to achieve full recovery. Regular screenings by primary care providers, educators, and mental health professionals can help identify warning signs before they escalate. These may include sudden weight loss, social withdrawal, irritability, obsessive behaviors around food, or expressions of hopelessness.
Increasing access to integrated treatment programs that address both depression and eating disorders is vital. These programs should offer medical monitoring, individualized therapy, nutritional support, and psychoeducation. When services are accessible, inclusive, and grounded in evidence-based practices, more individuals can receive the support they need to heal.
Reframing Recovery: A Holistic and Compassionate Approach
Recovery from depression and anorexia is rarely linear. It involves setbacks, breakthroughs, and moments of uncertainty. Yet with a holistic approach that honors both the psychological and physiological aspects of healing, recovery becomes not only possible but sustainable. This means recognizing that nutrition, therapy, social support, and personal agency all play critical roles in the journey toward wellness.
Rather than focusing solely on weight restoration or symptom reduction, effective treatment embraces the full humanity of the individual. It asks not only how to alleviate suffering but also how to cultivate joy, meaning, and resilience. For someone struggling with depression and an eating disorder, this may involve exploring new ways of relating to their body, processing past trauma, or rediscovering passions that had been buried beneath the weight of mental illness.
Hope is a powerful force in recovery. While the coexistence of depression and anorexia can feel overwhelming, it is important to remember that healing is possible—with time, support, and the right resources. As individuals rebuild their relationship with food and their sense of self, they begin to reclaim the vitality and connection that had once felt out of reach.
Frequently Asked Questions: Understanding the Link Between Depression and Eating Disorders
What are some early behavioral signs that depression and eating disorders may be developing together?
When depression and eating disorders begin to coexist, subtle behavioral changes often appear before more noticeable symptoms emerge. These can include withdrawing from social situations, especially those involving food, increased irritability, disrupted sleep, or fixation on body image beyond typical concern. A person might begin skipping meals or making excuses to avoid eating in public, citing vague health issues. At the same time, they may exhibit signs of hopelessness or a lack of motivation that go beyond situational sadness. Recognizing these patterns early is vital, particularly since depression and eating disorders can reinforce each other and accelerate in severity if left unaddressed.
How can depression coexist with anorexia without being immediately obvious to others?
It is entirely possible for depression to coexist with anorexia while remaining hidden due to the way individuals with these conditions often mask their symptoms. People may maintain high levels of functionality in work or academics while privately battling severe mental health challenges. In such cases, high-functioning depression combined with disordered eating can be mistaken for discipline or ambition. The internalization of distress—manifesting in restrictive eating and self-criticism—can go unnoticed by others who may only see outward productivity. Because both depression and eating disorders can be deeply concealed, it’s crucial to approach behavioral changes with compassion rather than assumptions.
What treatment challenges arise when depression and eating disorders occur simultaneously?
When depression and eating disorders coexist, treatment becomes more complex due to the interplay between emotional and physical symptoms. For example, therapy may be less effective when a person is malnourished, as cognitive processing and emotional regulation are impaired. Conversely, nutritional rehabilitation may be resisted if the underlying depression causes apathy or resistance to self-care. Healthcare providers must navigate these dynamics carefully, creating integrated plans that address both the physiological and psychological needs of the patient. These plans often include multidisciplinary support involving dietitians, psychotherapists, and medical professionals to ensure holistic care.
Are there gender differences in how depression and eating disorders manifest together?
Yes, the way depression and eating disorders manifest can vary significantly across genders, often influencing how they are recognized and treated. For example, while anorexia is more commonly diagnosed in females, males are more likely to present with atypical symptoms or use exercise and muscle-building as a form of disordered behavior. Men may also be less likely to report depressive symptoms due to societal stigma, leading to underdiagnosis or misdiagnosis. When depression coexists with anorexia in males or non-binary individuals, it may go undetected for longer due to these differences in expression and cultural biases. This highlights the importance of gender-sensitive approaches in screening and treatment.
How do digital culture and social media influence the co-occurrence of depression and eating disorders?
Digital culture can significantly intensify the connection between depression and eating disorders, especially among adolescents and young adults. Social media platforms often promote unrealistic beauty standards and diet culture, contributing to body dissatisfaction and negative self-comparisons. Algorithms may even amplify exposure to triggering content, further deepening mental health challenges. When a person is already vulnerable to depression, this digital environment can push them toward disordered eating behaviors as a misguided form of control or self-validation. Addressing these influences requires digital literacy education, boundaries around online content consumption, and therapeutic strategies to help individuals separate self-worth from appearance.
Can family dynamics affect whether depression and eating disorders appear together?
Family dynamics play a powerful role in shaping vulnerability to co-occurring mental health conditions. Environments where emotional needs are minimized, perfectionism is emphasized, or food is moralized may increase the risk that depression and eating disorders develop together. In some families, emotional communication may be limited, leaving young people to manage distress through food restriction or internalization. Additionally, a family history of mental illness or disordered eating behaviors can increase genetic and environmental risk factors. Creating open channels of dialogue and fostering emotionally supportive environments can act as a preventative measure and also facilitate recovery when these disorders are present.
What role does identity and self-concept play in the overlap of depression and eating disorders?
Self-concept is central to understanding how depression and eating disorders coexist. Many individuals with these conditions experience a fractured sense of identity, often tying their self-worth to achievement, appearance, or control. This fragile self-concept is susceptible to feelings of failure or shame, which can fuel both depressive episodes and disordered eating behaviors. Adolescents and emerging adults are particularly vulnerable as their identities are still forming and may be heavily influenced by peer and societal expectations. Therapeutic interventions that help individuals explore values, redefine self-worth, and build resilience are especially helpful in restoring a more stable and positive sense of self.
How can healthcare providers better identify when depression and eating disorders are co-occurring?
Improving identification of co-occurring depression and eating disorders starts with more nuanced screening tools and practitioner training. Standard depression assessments should include questions that probe for disordered eating patterns, body dissatisfaction, and extreme dietary behaviors. Likewise, evaluations for eating disorders must also consider mood symptoms like apathy, guilt, or persistent sadness. Healthcare providers should be trained to look beyond weight or appearance, recognizing that eating disorders can present across a range of body types. A trauma-informed and culturally sensitive approach also increases the likelihood of accurate diagnosis, particularly in marginalized populations who may express symptoms differently.
What are the long-term health risks if depression and eating disorders are not treated together?
When depression and eating disorders go untreated or are addressed in isolation, the consequences can be both medically and psychologically devastating. Long-term malnutrition weakens virtually every organ system, increasing the risk of cardiovascular complications, osteoporosis, reproductive issues, and cognitive impairment. At the same time, chronic depression can erode relationships, reduce academic or career performance, and lead to substance misuse or suicidal ideation. Without integrated treatment, individuals may cycle between partial recoveries and relapses, unable to sustain long-term wellness. Coordinated care that addresses both conditions concurrently is essential for breaking this cycle and supporting enduring recovery.
How can support networks help individuals manage the challenges of having both depression and anorexia?
Support networks—including family, friends, mentors, and recovery communities—can make a profound difference in navigating co-occurring mental health challenges. When depression and eating disorders coexist, individuals often feel isolated and misunderstood, making external validation and connection even more important. Support networks can provide practical help, such as meal support or accompanying someone to appointments, as well as emotional reinforcement during periods of doubt or relapse. Encouraging open conversations, educating oneself about the nuances of these conditions, and offering nonjudgmental presence are powerful ways to foster healing. Moreover, involving support networks in therapy, when appropriate, can strengthen the continuity of care and reinforce treatment goals.
Final Thoughts: How Understanding the Link Between Depression and Eating Disorders Can Support Long-Term Wellness
Recognizing that depression and eating disorders often share psychological roots and biochemical pathways allows for more effective, compassionate care. Understanding that depression can coexist with anorexia is crucial for early diagnosis and integrated treatment planning. When healthcare providers, loved ones, and individuals themselves are aware of this connection, they can take meaningful steps toward recovery.
Nutrition emerges not merely as a means of physical restoration but as a bridge to emotional and cognitive healing. From mindful eating to strategic refeeding, nutrition plays a critical role in stabilizing mood, restoring energy, and supporting brain function. When combined with therapy and community support, it becomes a cornerstone of sustainable recovery.
By approaching these conditions through the lens of empathy, expertise, and evidence-based practice, we can begin to dismantle the stigma that too often keeps people suffering in silence. With early intervention, holistic care, and the belief that healing is possible, individuals affected by depression and eating disorders can reclaim their lives and build a foundation for long-term wellness.
As we continue to educate ourselves and others about the intricate relationship between depression and eating disorders, we not only foster better mental health outcomes but also cultivate a culture of understanding and compassion. And in doing so, we offer hope—not just for survival, but for a life defined by connection, nourishment, and meaning.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Eating Disorders: What You Need to Know
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.

