Understanding when to visit a healthcare provider is one of the most overlooked aspects of modern preventive medicine. In a world where we are constantly juggling multiple responsibilities, it is easy to delay routine medical appointments until symptoms force action. However, knowing how often should you see a doctor is crucial not only for managing acute issues but for ensuring long-term wellness and identifying potential problems before they escalate. For many, early detection is the line between timely intervention and more complicated, chronic conditions.
There is no one-size-fits-all answer to this important health question, but expert guidelines based on age, lifestyle, gender, risk factors, and medical history offer reliable frameworks. A proactive approach to healthcare empowers individuals to take control of their well-being, reduce healthcare costs over time, and enjoy a better quality of life. Let us explore the essential factors that determine medical visit frequency, the types of checkups that promote wellness, and why even those in seemingly perfect health should never skip routine evaluations.
You may also like: The Vital Health Benefits of Preventive Medicine: Why Early Detection Matters More Than Ever

Why Routine Checkups Matter: More Than Just a Quick Scan
Routine checkups serve as a foundational pillar of preventive medicine. These visits are not merely perfunctory or limited to taking your blood pressure or stepping on a scale. Rather, they offer a comprehensive opportunity to assess your overall health, update vaccinations, screen for diseases, and build a long-term relationship with your primary care physician. It is during these visits that doctors can spot trends, subtle changes, or early symptoms that might otherwise go unnoticed.
Many individuals, particularly those in their 20s and 30s, assume that good health in the present moment ensures wellness in the future. However, chronic illnesses such as hypertension, diabetes, and high cholesterol often begin to develop silently, without outward signs. By scheduling regular exams, individuals gain access to baseline measurements that can guide future treatment decisions. The frequency of these visits can vary based on specific needs, but the consistent thread is the same: early detection saves lives.
Equally important is the psychological benefit of checkups. Preventive visits often provide peace of mind, reassurance, and the motivation to adopt healthier habits. When doctors have the opportunity to review your health history, evaluate risk factors, and engage in honest conversations about your lifestyle, they can make personalized recommendations tailored to your unique needs. These discussions often include mental health, sexual wellness, sleep patterns, stress management, and nutrition—areas that contribute significantly to a person’s overall well-being.
How Often Should You See a Doctor in Your 20s and 30s?
The younger decades of adulthood are often marked by resilience and a sense of invincibility, which can lead many to skip their annual health visits. Yet this stage of life lays the groundwork for future health, making it critical to establish healthy habits and identify risks early on. So, how often should you get a physical in your 20s and 30s? While many health experts recommend at least one full physical exam every one to three years for healthy adults in this age range, more frequent visits may be warranted based on individual needs.
Key components of these visits should include a detailed family history review, mental health screening, sexual health consultation, and early metabolic screenings such as cholesterol and blood sugar checks. Additionally, women may need more frequent gynecological exams, especially those involving cervical cancer screening, which begins around age 21 and continues every three to five years depending on the testing method used.
Vaccinations and booster shots are also a significant part of preventive care during these years. For instance, Tdap, HPV, and influenza vaccines help safeguard against long-term illnesses. Lifestyle counseling plays a central role in these appointments as well, with a focus on physical activity, dietary habits, alcohol consumption, tobacco use, and substance abuse. These early interventions, when consistently applied, have long-lasting ripple effects on wellness into midlife and beyond.
The Role of Preventive Care in Middle Adulthood: Ages 40 to 64
As we move into middle adulthood, the focus of preventive care intensifies. At this stage, risks for chronic conditions increase substantially. For individuals between the ages of 40 and 64, how often should you get routine checkups at the doctor becomes a more urgent question. The general recommendation is to schedule a comprehensive physical exam annually, especially for those with a family history of cardiovascular disease, cancer, diabetes, or autoimmune conditions.
Annual physicals typically include screenings for blood pressure, cholesterol, blood glucose levels, thyroid function, and cancer markers. Colon cancer screening begins around age 45 for most adults, while women continue with mammograms, and men may begin discussions about prostate health. These visits also mark the period where bone density becomes relevant, particularly for post-menopausal women at risk of osteoporosis.
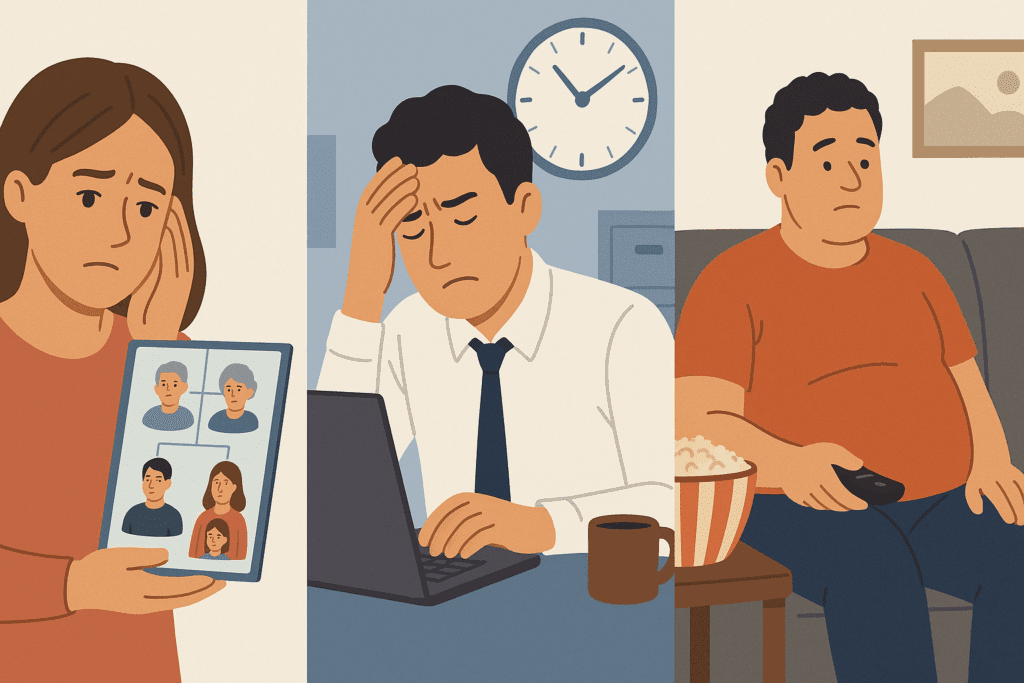
This period of life often includes shifts in metabolism, energy levels, and mental health. Midlife stress, workplace burnout, caregiving responsibilities, and hormonal changes can affect overall vitality. Annual appointments provide a crucial opportunity to discuss these changes with your physician and ensure that both physical and emotional health are being addressed. Vaccinations, including shingles and pneumococcal vaccines, also become part of the preventive care conversation in this age group.
How Often Should You Get a Check Up After Age 65?
The senior years introduce a different rhythm of healthcare, one that prioritizes both prevention and the management of existing health conditions. After the age of 65, how often should you have a check up depends heavily on a person’s health status. For most seniors, annual physicals are considered essential, and additional follow-up visits may be scheduled to manage medications, monitor chronic illnesses, or assess cognitive and physical function.
Geriatric care emphasizes functional ability, mobility, memory, vision, and hearing assessments. Preventive screenings continue, but the approach becomes more personalized, focusing on quality of life and maintaining independence. Older adults are also more susceptible to immunization-preventable diseases; therefore, vaccinations for influenza, pneumonia, shingles, and COVID-19 boosters are emphasized. Mental health evaluations, particularly for depression and dementia, are a core part of routine visits.
Beyond the clinic, discussions around advanced care planning and end-of-life preferences are encouraged. While these topics can be emotionally charged, they are necessary for ensuring that a patient’s values and wishes are honored. As older adults navigate polypharmacy and complex health regimens, the doctor-patient relationship becomes a lifeline—a trusted partnership that supports informed decision-making, independence, and holistic wellness.

Specialty Visits: When to Go Beyond the Primary Care Physician
While primary care forms the bedrock of preventive medicine, certain health needs require specialty evaluation. So, how often do you need a physical may depend on whether a particular condition necessitates the input of a specialist. For example, individuals with cardiovascular risk factors might need to see a cardiologist annually or biannually, depending on test results and lifestyle changes. Similarly, those with autoimmune disorders, endocrine issues, or complex gastrointestinal symptoms benefit from specialist-led care that complements routine exams.
Women may see a gynecologist regularly for reproductive health assessments, while men might visit a urologist for prostate screenings or concerns related to sexual function. Dermatological checkups for mole mapping and skin cancer screening become relevant, particularly for those with high sun exposure or a history of melanoma. Eye exams, hearing tests, and dental checkups should also be scheduled regularly, even when symptoms are not present.
These specialist visits should not replace general physical exams but rather act as a coordinated component of comprehensive health management. Effective communication between your primary care provider and specialists helps ensure that your care is integrated, medications are not duplicated, and no critical detail falls through the cracks. When your doctor recommends a specialist, it’s a signal that your care needs a focused lens—a sign not of illness, but of attentive and proactive healthcare.
Factors That Influence Doctor Visit Frequency
While general age-based guidelines offer helpful direction, they don’t tell the full story. The question of how often should you see a doctor ultimately hinges on several personal variables. Lifestyle choices, including smoking, diet, exercise habits, and alcohol use, can all affect your risk profile. Individuals who lead high-stress lives or have sedentary jobs might benefit from more frequent wellness visits to mitigate long-term health risks.
Family history is another crucial determinant. A parent with early-onset heart disease, breast cancer, or type 2 diabetes increases your likelihood of developing similar conditions. In such cases, screenings may begin earlier or occur more frequently. Racial and ethnic background can also play a role, as certain populations face increased susceptibility to specific diseases. For instance, African Americans have higher rates of hypertension and kidney disease, while Ashkenazi Jews may carry genetic mutations linked to cancer.
Furthermore, socioeconomic status and access to healthcare significantly impact checkup regularity. Those without insurance or living in underserved areas may face barriers to care that delay diagnosis and treatment. In contrast, individuals with regular healthcare access may undergo more preventive services and, in turn, experience better long-term outcomes. Understanding these nuances reinforces the importance of personalized care strategies that reflect the realities of each patient’s life.
How Often Should You Have a Physical if You Feel Healthy?
Perhaps the most common reason people skip doctor visits is the assumption that good health means no need for evaluation. This mindset, while understandable, can be misleading. Many conditions develop silently, presenting no symptoms until they are advanced. So, how often should you get a physical even when you’re feeling fine? The answer: at least once a year, particularly as you age or if risk factors are present.
Preventive medicine hinges on early intervention. Blood pressure, cholesterol, and glucose abnormalities often go unnoticed until they cause complications. Cancer screenings, such as Pap smears, mammograms, colonoscopies, and skin checks, are essential in asymptomatic stages. These screenings offer the best chance for successful treatment and, in some cases, full recovery.
Moreover, a physical exam is an opportunity to talk about mental and emotional health—areas that patients may not bring up unless asked. Sleep disturbances, fatigue, mood changes, and anxiety can all emerge in subtle ways and often benefit from early management. Your doctor may also review your medications, discuss health goals, and provide lifestyle coaching that reinforces long-term wellness. Feeling well should never be a reason to avoid your doctor; rather, it is the perfect time to build a strategy for staying that way.
How Often Should You Get Routine Checkups at the Doctor for Chronic Conditions?
For individuals managing chronic health issues, routine checkups are more than preventive—they are foundational. Patients with diabetes, hypertension, asthma, thyroid disease, or autoimmune disorders should maintain regular follow-up visits, often every three to six months, depending on condition stability and treatment complexity. These visits monitor disease progression, track medication effectiveness, and adjust regimens as needed.
Regular lab work is a core component of these visits. Glycated hemoglobin (A1C) tests, lipid panels, kidney function, and inflammatory markers provide essential data for chronic disease management. Imaging studies, such as X-rays, MRIs, and ultrasounds, may also be part of ongoing surveillance, particularly in conditions like rheumatoid arthritis, cardiovascular disease, or liver dysfunction.
Patient engagement is key in chronic care. Tracking blood pressure, blood sugar, or symptom logs at home can provide valuable insights to your doctor and promote shared decision-making. These collaborative appointments allow for treatment optimization, complication prevention, and enhanced quality of life. While the frequency of visits may vary, the goal remains constant: personalized, consistent, and proactive care.
The Connection Between Mental Health and Physical Checkups
Increasingly, healthcare providers are recognizing the integral role mental health plays in overall wellness. During a routine visit, a doctor may assess not only physical signs but also emotional well-being. How often should you see a doctor becomes even more critical when mental health concerns are present or suspected. For individuals managing depression, anxiety, PTSD, or substance use disorders, regular appointments can offer a supportive environment for evaluation, medication management, and referral to counseling.
Even when no formal diagnosis exists, conversations about stress, burnout, and life transitions provide opportunities for early support. These discussions might uncover sleep disturbances, appetite changes, or emotional fatigue that affect both mind and body. Preventive medicine, therefore, extends beyond the physical exam to include empathetic, whole-person care.
Incorporating mental health screenings, such as PHQ-9 or GAD-7 questionnaires, into annual exams creates a foundation for addressing psychological concerns early. Moreover, patients who feel seen and heard by their providers are more likely to adhere to treatment plans and return for follow-up care. This connection fosters a therapeutic alliance that promotes both resilience and healing.
When to Seek Immediate Medical Attention Outside of Routine Visits
While routine checkups form the cornerstone of health maintenance, there are moments when immediate attention is necessary. Knowing when to act can prevent complications or even save a life. Symptoms such as chest pain, difficulty breathing, sudden weakness, uncontrolled bleeding, or changes in vision, speech, or balance require emergency evaluation. These are not moments to wait for your next physical—they demand prompt intervention.
Other red flags include unexplained weight loss, persistent fatigue, new lumps, or changes in bowel or bladder habits. These symptoms may signal serious conditions and should be addressed as soon as possible. Even when unsure, erring on the side of caution and contacting your provider is a wise decision. Many clinics offer same-day appointments or telehealth consultations that can quickly assess whether a trip to the emergency room is warranted.
Your intuition about your body is also valuable. If something feels off or different, it often is. While not every symptom is cause for alarm, timely evaluation ensures peace of mind and, when necessary, swift action. Integrating this mindset with your routine care plan creates a dynamic health strategy that is both preventive and responsive.
Frequently Asked Questions (FAQ)
How Often Should You See a Doctor: Addressing the Hidden Factors That Influence Frequency
1. Can mental health concerns affect how often you should see a doctor?
Absolutely, mental health is a powerful determinant in deciding how often you should see a doctor. Individuals dealing with anxiety, depression, PTSD, or chronic stress may benefit from more frequent primary care visits to ensure both their emotional and physical health are monitored cohesively. Routine checkups can serve as a safe space to explore symptoms like fatigue, poor concentration, or chronic insomnia, which often mask underlying psychological challenges. In recent years, many general practitioners have incorporated mental health screenings into their wellness protocols, making these appointments a valuable opportunity to address psychological well-being. Even in the absence of a formal diagnosis, discussing mental health during regular visits helps prevent burnout and encourages early interventions that support long-term wellness.
2. How does your job or lifestyle influence how often you should have a physical?
The nature of your occupation and daily routine significantly shapes how often you should have a physical. Sedentary office jobs may increase risks for cardiovascular issues, poor posture, or weight gain, while high-stress professions often correlate with elevated blood pressure and adrenal fatigue. Individuals exposed to toxins, shift work, or irregular sleep patterns may need more comprehensive annual evaluations, including metabolic, neurological, and endocrine screenings. Those in physically demanding roles might require periodic musculoskeletal evaluations or injury prevention counseling. Your doctor can tailor your checkup schedule based on these variables to ensure early detection of occupation-related health challenges.
3. How often should you get a physical in your 20s if you’re an athlete or high-performance individual?
Athletes and fitness enthusiasts in their 20s often assume peak physical condition eliminates the need for routine care—but that’s a misconception. If you’re highly active, how often should you get a physical in your 20s depends on your training intensity and recovery patterns. High-performance individuals are more prone to repetitive strain injuries, cardiac anomalies, or nutritional deficiencies, particularly if dietary intake doesn’t match output. A biannual checkup may be beneficial to assess electrolyte levels, heart health, joint function, and recovery status. This proactive approach ensures you’re not only performing optimally but also protecting your body from cumulative wear and tear.
4. Is it necessary to adjust your checkup frequency after major life events like childbirth or surgery?
Yes, major life events such as childbirth, major surgery, or a significant illness require a temporary shift in how often you should get a check up. For postpartum women, multiple follow-ups are recommended within the first year to assess physical recovery, mental health, and hormonal balance. Similarly, individuals recovering from surgery need periodic evaluations to track healing, manage pain, and monitor for complications such as infections or adhesions. These transitional periods place unique physiological demands on the body, warranting closer monitoring. Even seemingly straightforward recoveries can benefit from structured medical oversight to ensure a full return to health.
5. How often do you need a physical if you’re managing multiple medications?
Polypharmacy, or the use of multiple medications, complicates how often you need a physical. People taking three or more long-term prescriptions—common among older adults or individuals with chronic conditions—should schedule checkups at least every six months. These visits help identify potential drug interactions, assess side effects, and confirm that dosages remain effective over time. Bloodwork to monitor liver and kidney function, as well as periodic medication reconciliation, becomes essential. A thorough physical also provides space to evaluate whether lifestyle changes might reduce the need for certain prescriptions altogether.
6. How often should you get routine checkups at the doctor if you have a strong family history of disease?
A strong family history of disease significantly alters how often you should get routine checkups at the doctor. If immediate relatives have had early-onset cancer, heart disease, or genetic conditions, your physician may recommend earlier and more frequent screenings. For example, someone with a parent who had colon cancer at 45 might begin colonoscopies a decade earlier. Genetic counseling may also be advised to better understand inherited risk and tailor surveillance strategies. In these cases, annual physicals often include advanced imaging or blood panels designed to catch subtle signs before symptoms appear.
7. What role do technology and at-home health monitoring play in reducing checkup frequency?
Wearable tech and at-home diagnostics have revolutionized preventive care, yet they don’t replace in-person checkups entirely. Devices that track blood pressure, heart rate, sleep, and glucose can alert users to potential issues between visits, enhancing how often should you have a check up based on real-time data. However, these tools still rely on physician interpretation and can’t fully replicate a comprehensive physical exam. In some cases, consistent normal readings may allow for less frequent visits under medical supervision. That said, these innovations are best viewed as complements to, not replacements for, traditional care.
8. How often should you have a physical during transitional decades, like your 30s and 50s?
Transitional decades are periods when the body undergoes subtle yet significant changes, making it critical to re-evaluate how often should you have a physical. In your 30s, emerging metabolic shifts, fertility discussions, and early signs of stress-related disorders become more common. In your 50s, hormonal changes, cardiovascular risks, and bone density issues begin to surface even in asymptomatic individuals. Annual checkups during these decades serve as health recalibrations, ensuring that evolving needs are met with updated strategies. Regular lab work, cancer screenings, and lifestyle coaching become increasingly valuable in these age groups.
9. How do social determinants like income, housing, or education affect how often should you get a physical?
Social determinants have a profound, though often overlooked, impact on how often should you get a physical. Individuals facing housing instability, financial strain, or limited education may delay care, resulting in late diagnoses or untreated conditions. These barriers not only limit access but can also influence trust in healthcare systems. Outreach efforts, mobile clinics, and community-based healthcare models are critical tools in addressing these gaps. Encouraging health literacy and removing cost-related barriers helps ensure everyone can access the care they need at appropriate intervals, regardless of socioeconomic background.
10. How often should you see a doctor if you travel frequently or live abroad?
Frequent travelers and expatriates face unique healthcare challenges that affect how often should you see a doctor. Exposure to different climates, pathogens, and healthcare systems increases the need for pre-travel consultations and follow-up visits upon return. For long-term expatriates, continuity of care is key; maintaining a relationship with a primary provider back home or abroad helps track changes over time. Annual or semi-annual checkups become essential to ensure vaccinations are current, chronic conditions remain managed, and country-specific health risks are addressed. A proactive approach also includes maintaining a portable health record to share with international providers as needed.
Conclusion: Making Informed Choices About How Often You Should See a Doctor
Navigating how often should you see a doctor is a personal yet profoundly important decision. It requires a thoughtful understanding of your body, family history, lifestyle, and health goals. From the early years of adulthood through the complexities of aging, regular checkups form the scaffolding upon which lasting wellness is built. They empower you to make informed choices, catch potential problems early, and cultivate a proactive relationship with healthcare.
There is no magic number that fits everyone, but clear patterns emerge. Young, healthy adults benefit from visits every one to three years, while those over 40 or managing chronic conditions require annual or more frequent care. Feeling well should not be a reason to skip appointments; in fact, it is the best time to invest in preventive strategies that help you remain well.
In the end, knowing how often should you get a check up, how often should you have a physical, or how often should you get routine checkups at the doctor is not just about answering a question—it is about embracing a mindset of vigilance, empowerment, and resilience. Prioritizing your health, one visit at a time, is the ultimate expression of self-care and a gift to your future self. In doing so, you champion a life of vitality, clarity, and enduring wellness.