Understanding the importance of early interventions in reducing the risk of colorectal malignancies is a crucial component of public health strategy today. Colon and rectal cancer prevention is not merely a medical goal but a social imperative, as these cancers rank among the most prevalent and deadly forms of cancer worldwide. Recognizing this reality, both individuals and health systems must prioritize early detection, lifestyle modification, and awareness campaigns to combat the incidence and severity of these conditions. Prevention strategies rooted in evidence-based practices can significantly lower cancer risks, improve patient outcomes, and reduce healthcare burdens. As our understanding of colorectal cancer evolves, so must our strategies to prevent it, starting from a foundation of knowledge and moving toward actionable, transformative behaviors.
You may also like: The Vital Health Benefits of Preventive Medicine: Why Early Detection Matters More Than Ever
The Growing Burden of Colorectal Cancer in Modern Society
Colorectal cancer has steadily climbed the ranks of global health concerns, particularly in developed nations where sedentary lifestyles and processed diets have become the norm. The disease’s prevalence has surged not only among older adults, as traditionally observed, but alarmingly among younger populations as well. This trend underscores the necessity of shifting our focus from reactive treatment to proactive prevention. While medical advances have increased survival rates, they have not stemmed the tide of new diagnoses. Addressing the roots of colon and rectal cancer through lifestyle interventions, dietary changes, and early screening can profoundly alter this trajectory.
In the United States alone, the American Cancer Society estimates over 150,000 new cases of colorectal cancer annually, with nearly 53,000 resulting in death. Globally, it is the third most commonly diagnosed cancer and the second leading cause of cancer-related deaths. These sobering statistics highlight a critical need for both systemic changes in public health policy and individual accountability in wellness practices. Understanding these trends empowers communities to take more control over their health outcomes and to advocate for greater access to preventative healthcare resources.
Recognizing Risk Factors and Their Role in Colon and Rectal Cancer Prevention
Effective colon and rectal cancer prevention hinges on a comprehensive understanding of risk factors. These can be broadly categorized into non-modifiable and modifiable risks. Non-modifiable risks include age, genetics, and personal history of inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis. Individuals with a first-degree relative who has had colorectal cancer have a two- to threefold increased risk of developing the disease themselves. Likewise, hereditary conditions like Lynch syndrome or familial adenomatous polyposis dramatically elevate risk levels.
However, modifiable risk factors provide a critical window for prevention. Diets high in red and processed meats, lack of physical activity, obesity, tobacco use, and excessive alcohol consumption all contribute significantly to colorectal cancer development. Studies have shown that people who adopt healthier lifestyles, rich in fruits, vegetables, and whole grains, and who maintain a healthy weight through regular exercise, have a substantially lower risk of developing these cancers. Understanding these modifiable risk factors enables individuals to make informed choices about their health while giving clinicians a framework for targeted interventions.

The Role of Diet and Nutrition in Colorectal Health
Nutrition is one of the most potent tools in the arsenal for cancer colorectal prevention. The gastrointestinal system is directly affected by dietary intake, meaning the food choices individuals make daily can either contribute to carcinogenesis or help ward it off. Diets high in fiber have been associated with a reduced risk of colorectal cancer due to their role in speeding up the digestive process and reducing the time potential carcinogens remain in the colon.
Conversely, high consumption of processed meats, such as sausages, bacon, and deli meats, has been classified as carcinogenic by the World Health Organization. Reducing intake of these foods while increasing consumption of plant-based foods can lead to significant improvements in colorectal health. Moreover, calcium and vitamin D have shown protective benefits against colorectal cancer in some studies, suggesting that dairy products and sunlight exposure, in moderation, can also be beneficial.
Incorporating anti-inflammatory foods, such as omega-3-rich fish, leafy greens, nuts, and berries, into one’s diet may further contribute to lowering cancer risk. These foods help regulate the body’s immune response and decrease chronic inflammation, a condition linked to cancer development. Thus, dietary modifications not only serve as preventive measures but also enhance overall digestive health and well-being.
Exercise and Physical Activity as Preventive Strategies
Physical activity has been consistently linked to lower rates of colorectal cancer. Regular exercise reduces inflammation, improves immune function, enhances metabolism, and helps maintain a healthy weight—all factors associated with reduced cancer risk. Engaging in at least 150 minutes of moderate-intensity exercise per week can significantly influence one’s likelihood of developing colon and rectal cancer.
The protective effects of exercise are partly due to improved bowel motility, which reduces the contact time between potential carcinogens and the colon lining. Additionally, physical activity can positively influence hormone levels and insulin sensitivity, further reducing cancer risk. Whether through brisk walking, cycling, swimming, or structured fitness routines, the incorporation of physical activity into daily life should be a priority for those seeking to mitigate cancer risk.
Beyond its physiological benefits, exercise also contributes to mental health, which is often overlooked in cancer prevention. A positive mental state can lead to better adherence to healthy behaviors, improved sleep, and reduced stress—all of which play a role in holistic wellness. Encouraging communities to adopt active lifestyles through accessible programs and public health campaigns remains a pivotal strategy in the prevention effort.
The Importance of Early Detection and Screening in Colon and Rectal Cancer Prevention
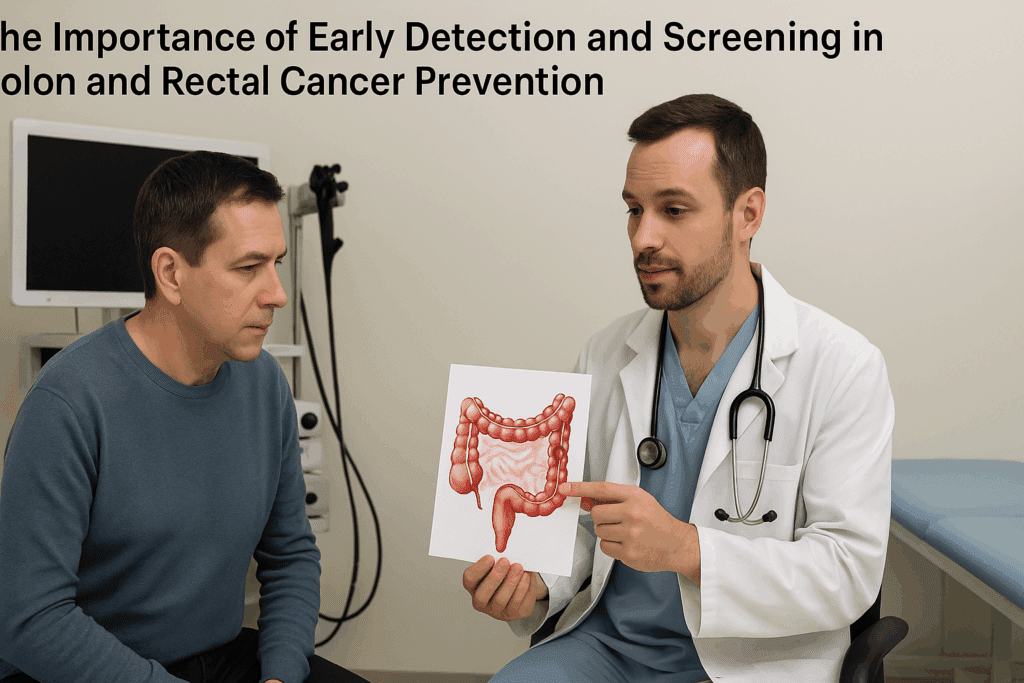
Among the most effective tools in colon and rectal cancer prevention is early detection through regular screening. Screening allows for the identification and removal of precancerous polyps before they progress to malignancy. Colonoscopy, the gold standard for colorectal screening, can detect both early-stage cancers and polyps that might later develop into cancer if left untreated.
The U.S. Preventive Services Task Force recommends that individuals at average risk begin colorectal screening at age 45. However, those with a family history or other risk factors may need to start earlier. Screening options also include stool tests, such as the fecal immunochemical test (FIT) and stool DNA tests, which detect signs of cancer or polyps through non-invasive means. While these tests do not replace colonoscopy, they serve as valuable alternatives for individuals unwilling or unable to undergo more invasive procedures.
Early detection significantly improves prognosis. When colorectal cancer is caught at an early stage, the five-year survival rate exceeds 90%. Unfortunately, many cases are still diagnosed at advanced stages due to lack of screening. Increasing awareness about the benefits of early detection and breaking down barriers to screening access—whether due to cost, fear, or misinformation—is critical in reducing colorectal cancer mortality.
Colon and Rectal Cancer Prevention Through Gut Microbiome Health
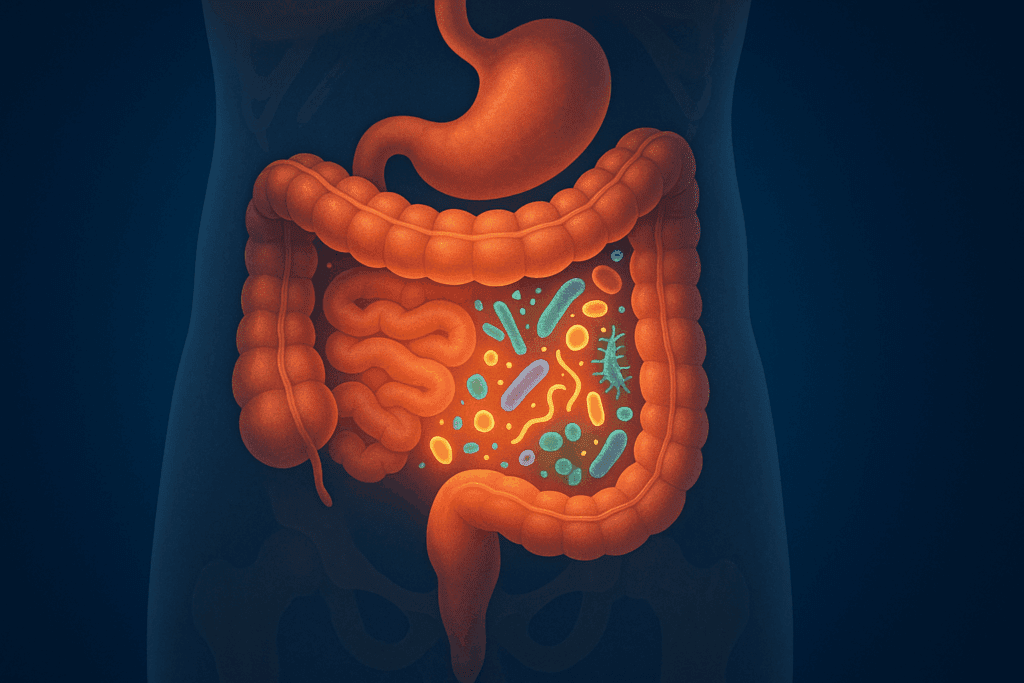
Recent research has illuminated the role of the gut microbiome in colon and rectal cancer prevention. The human gut contains trillions of microorganisms that influence digestion, immune function, and even gene expression. Disruptions in the balance of this microbiome—often due to poor diet, antibiotic overuse, or chronic stress—have been linked to inflammation and carcinogenesis in the colon.
Promoting a healthy microbiome through diet and lifestyle can enhance colorectal cancer prevention efforts. Prebiotics (found in foods like onions, garlic, bananas, and oats) and probiotics (such as those found in yogurt, kefir, and fermented vegetables) help cultivate beneficial bacteria in the gut. These microbes produce short-chain fatty acids, such as butyrate, that protect colon cells and may inhibit tumor formation.
In addition to diet, avoiding unnecessary antibiotic use and managing stress also support microbial diversity. Emerging research even suggests that the microbiome could one day inform personalized screening protocols or targeted therapies. While more studies are needed to fully understand this connection, fostering microbiome health represents a promising frontier in cancer colorectal prevention.
Genetics, Family History, and Personalized Prevention Plans
Genetic predispositions play a significant role in colorectal cancer risk, particularly in individuals with inherited conditions such as Lynch syndrome or familial adenomatous polyposis. Genetic counseling and testing can help identify high-risk individuals who may benefit from more aggressive screening or preventative interventions. These personalized plans may include earlier and more frequent colonoscopies, prophylactic surgeries, or chemoprevention strategies.
Family history also serves as a strong indicator of potential risk. Individuals with one or more first-degree relatives diagnosed with colorectal cancer should consult with their healthcare providers to determine an appropriate screening schedule. Understanding genetic risks empowers individuals and families to take proactive steps toward prevention.
Furthermore, advancements in precision medicine are enabling tailored risk assessments based on genetic markers and lifestyle factors. These individualized approaches offer more nuanced strategies for prevention, moving away from one-size-fits-all recommendations and toward a future where prevention is as personalized as treatment.
The Influence of Socioeconomic and Cultural Factors on Prevention Access
Access to preventive healthcare services, including screening and nutritional counseling, varies widely based on socioeconomic status, geographic location, and cultural background. Populations in rural or underserved areas often face significant barriers to care, including transportation challenges, lack of healthcare providers, and financial constraints.
Cultural beliefs and stigmas also impact willingness to undergo screening or discuss digestive health. In some communities, talking about bowel movements or undergoing invasive procedures may be considered taboo, deterring individuals from seeking timely care. Public health initiatives must therefore be culturally sensitive and linguistically appropriate to bridge these gaps.
Addressing these disparities requires systemic changes, such as expanding insurance coverage, investing in mobile screening units, and training community health workers. By acknowledging and actively working to eliminate these barriers, society can ensure that colon and rectal cancer prevention is equitable and inclusive.
Medical Innovations Advancing Colon and Rectal Cancer Prevention
The medical field continues to develop innovative technologies that enhance colorectal cancer prevention and detection. Advanced imaging techniques, such as high-definition colonoscopy and narrow-band imaging, have improved the accuracy of polyp detection. Meanwhile, artificial intelligence is being integrated into colonoscopy software to help identify abnormalities that may be missed by the human eye.
Non-invasive tests are also advancing rapidly. Liquid biopsies that detect circulating tumor DNA offer the potential for earlier and less invasive diagnosis. Researchers are developing blood-based tests that could supplement or even replace traditional stool tests, making screening more accessible and less burdensome.
In addition, research into chemoprevention—the use of medications to prevent cancer—is showing promise. Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) have been linked to a reduced risk of colorectal cancer in some populations, although their use must be carefully considered due to potential side effects. As these innovations mature, they offer new avenues for prevention and broaden the scope of available tools.
Integrating Colon and Rectal Cancer Prevention into Daily Life
Prevention is most effective when it becomes an integral part of daily living rather than an occasional consideration. Individuals can take meaningful steps each day to reduce their risk of colorectal cancer. These include preparing balanced meals rich in fiber and nutrients, scheduling routine screenings, engaging in regular physical activity, managing stress, and avoiding tobacco and excessive alcohol.
Workplaces and schools can play a role by promoting healthy environments. Offering nutritious meal options, encouraging movement breaks, and providing educational resources about cancer prevention fosters a culture of wellness. Communities can further support prevention through accessible parks, walking trails, and wellness programs that bring health education directly to the public.
Creating supportive environments that normalize conversations about digestive health and remove stigma is also essential. Open dialogue with healthcare providers about symptoms, family history, and risk factors enables timely interventions. Prevention is not a solitary effort; it requires the participation of families, communities, healthcare systems, and policymakers.
Education, Awareness, and the Power of Public Health Campaigns
Public health campaigns have the power to transform awareness into action. Educational initiatives that demystify colonoscopy, highlight the importance of early detection, and provide clear guidance on prevention strategies can motivate individuals to prioritize their health. Effective campaigns use storytelling, visual media, and community engagement to resonate with diverse audiences.
Colorectal Cancer Awareness Month, observed every March, serves as a focal point for such efforts. During this time, healthcare providers, advocacy organizations, and media outlets collaborate to spread crucial information. Social media campaigns, community events, and partnerships with influencers further amplify the message.
These campaigns are most effective when sustained year-round and supported by policy changes that facilitate access to screening and wellness services. Education and awareness are powerful tools that equip individuals with the knowledge and motivation to make health-conscious choices that reduce their cancer risk.
Frequently Asked Questions: Colon and Rectal Cancer Prevention
How does stress influence colon and rectal cancer prevention?
Chronic stress may seem disconnected from gastrointestinal health, but long-term psychological strain can subtly impair immune function and gut microbiota, both of which play a role in cancer colorectal prevention. Cortisol, the body’s primary stress hormone, can increase inflammation and disrupt cellular repair mechanisms, potentially creating an environment more conducive to carcinogenesis. Furthermore, stressed individuals are more likely to adopt unhealthy coping habits, such as poor dietary choices, alcohol overconsumption, or smoking, which are well-established risk factors. Incorporating mindfulness practices, cognitive behavioral therapy, or regular physical activity can buffer these effects and support both mental and physical well-being. Although stress alone does not cause cancer, managing it is an often-overlooked element of a holistic prevention strategy.
What is the role of environmental toxins in colon and rectal cancer risk?
Environmental exposure to certain toxins can subtly influence long-term colorectal cancer risk, particularly for those working in industries involving heavy metals, pesticides, or industrial solvents. Prolonged contact with such substances may increase systemic inflammation and oxidative stress, potentially triggering DNA mutations over time. Drinking water contaminants like arsenic or nitrates have also been investigated for their links to gastrointestinal malignancies. While the evidence is still emerging, individuals in high-risk regions may benefit from water filtration systems and occupational health evaluations. A proactive approach to minimizing environmental exposure aligns well with broader cancer colorectal prevention strategies.
Are there early signs of risk that are not yet classified as symptoms?
Yes, there are several physiological changes that may precede obvious symptoms and warrant attention even if they are not yet classified as clinical signs. For instance, subtle shifts in bowel regularity, mild but consistent bloating, or the presence of microinflammation in colon tissue may signal increased risk, especially for individuals with a family history. Emerging research also suggests that epigenetic changes—alterations in gene expression without DNA mutation—can serve as early biomarkers for susceptibility. Tracking these indicators through advanced screening or digital health monitoring tools may lead to earlier interventions. Awareness of these subclinical changes enhances the overall effort in colon and rectal cancer prevention.
How can artificial intelligence help improve colonoscopy outcomes?
Artificial intelligence (AI) is revolutionizing colonoscopy by enhancing the detection of polyps, particularly flat or small lesions that are easy to miss. AI algorithms can now analyze video feeds in real time, flagging suspicious growths for closer inspection. Studies show that AI-assisted colonoscopy improves adenoma detection rates significantly compared to traditional methods. This not only improves diagnostic accuracy but also contributes to long-term colon and rectal cancer prevention by ensuring fewer precancerous polyps go unnoticed. In the future, AI might also personalize screening intervals based on individual risk profiles, optimizing both safety and resource use.
What emerging trends are shaping future cancer colorectal prevention strategies?
One compelling trend is the shift toward precision prevention—using genetic, environmental, and lifestyle data to create customized risk reduction plans. Another is the integration of wearable health technology, such as smartwatches and biosensors, which can track indicators like inflammation, sleep patterns, and exercise levels. These insights provide real-time feedback and help individuals adhere more closely to prevention guidelines. Nutrigenomics, the study of how diet interacts with genes, is also gaining traction, suggesting that some people may benefit from personalized nutrition plans to reduce cancer risk. Together, these innovations are paving the way for a more proactive, individualized approach to colon and rectal cancer prevention.
How can workplace culture influence colon and rectal cancer prevention?
Workplace environments play a surprisingly impactful role in promoting or inhibiting preventive behaviors. Offices that encourage long periods of sedentary work, for instance, may inadvertently raise colorectal cancer risk due to reduced physical activity. Conversely, companies that provide healthy meal options, on-site fitness classes, or flexible schedules for medical appointments foster a culture of well-being. Offering educational sessions about cancer colorectal prevention can empower employees to make informed health decisions. By integrating wellness into daily operations, workplaces can serve as a frontline defense in public health efforts.
What lesser-known dietary strategies support prevention?
Beyond fiber intake, certain phytochemicals found in herbs and spices may offer protective benefits. Curcumin, a compound in turmeric, has demonstrated anti-inflammatory and anti-carcinogenic properties in lab studies, while garlic’s allicin may support gut immunity. Incorporating fermented foods, such as miso or kimchi, further enhances gut flora diversity, a key aspect of cancer colorectal prevention. Additionally, time-restricted eating, which aligns eating schedules with circadian rhythms, may improve metabolic efficiency and reduce systemic inflammation. These nuanced dietary shifts can complement broader nutritional guidelines for prevention.
How do sleep patterns relate to colon and rectal cancer risk?
Poor sleep has been linked to increased inflammation, hormonal imbalance, and insulin resistance—all of which can heighten cancer susceptibility. Shift workers, in particular, face disrupted circadian rhythms that have been associated with increased colorectal cancer incidence. Ensuring adequate and consistent sleep allows the body to regulate cellular repair processes critical for long-term health. Sleep hygiene practices such as limiting screen time before bed, creating a dark sleep environment, and sticking to regular sleep schedules can bolster preventive efforts. Integrating sleep quality assessments into routine health evaluations could offer additional layers of insight for colon and rectal cancer prevention.
Is there a link between hormone therapy and colorectal cancer risk?
Hormone replacement therapy (HRT), often used during menopause, has been associated with both risks and benefits regarding colorectal cancer. Some studies suggest that certain forms of HRT may lower colorectal cancer incidence, possibly due to hormonal regulation of cell growth in the colon. However, the type, dosage, and duration of hormone therapy matter significantly, and these benefits must be weighed against other potential health risks. It’s essential for individuals considering HRT to engage in shared decision-making with their healthcare providers. Personalized assessments are critical to determine whether HRT aligns with comprehensive cancer colorectal prevention goals.
How do community health programs enhance prevention success?
Community health programs bring awareness and services directly to populations that may face barriers to traditional healthcare systems. By offering mobile screening units, culturally tailored education, and language-accessible resources, these initiatives address social determinants of health. Programs that involve trusted local leaders often achieve greater engagement, particularly in marginalized or rural communities. Collaborative partnerships between public health agencies and community organizations can drive early screening and foster sustainable behavior change. Through localized efforts, community health programs act as a powerful extension of broader colon and rectal cancer prevention campaigns.
Conclusion: Embracing a Lifelong Commitment to Colon and Rectal Cancer Prevention
Colon and rectal cancer prevention is not a one-time initiative but a lifelong commitment to proactive health management. From understanding risk factors and adopting healthy habits to prioritizing early detection and embracing medical innovations, the journey toward prevention is multifaceted and dynamic. As individuals become more informed and empowered, and as systems evolve to support equitable access to care, the potential to reduce the global burden of colorectal cancer becomes increasingly attainable.
This commitment requires action at every level: personal responsibility for lifestyle choices, familial awareness of genetic risks, community support for wellness initiatives, and societal investment in accessible healthcare. By integrating these strategies into everyday life and advocating for systemic change, we can make significant strides in reducing the incidence and impact of this disease.
Ultimately, prevention is about more than avoiding illness; it is about cultivating a life of vitality, awareness, and resilience. As we move forward, let us prioritize colon and rectal cancer prevention as a cornerstone of public health and individual well-being, recognizing that early steps today lay the foundation for a healthier, cancer-free future tomorrow.
Further Reading:
Reducing your risk for colorectal cancer

