Optimizing Your Body and Heart: Why Nutrition Matters for Endurance and Wellness
Performance isn’t just about muscle mass, VO₂ max, or how fast you can finish a mile. At the core of true endurance and long-term vitality lies one of the most overlooked components: heart health. Whether you’re a seasoned triathlete, a weekend cyclist, or someone managing a cardiovascular condition, the right dietary foundation is essential. A scientifically backed cardiovascular diet plan doesn’t just support heart health in a clinical sense—it fuels sustained energy output, quicker recovery, and stronger long-term resilience. Understanding the synergy between what we eat and how our heart performs is the first step toward optimizing both daily activity and lifelong wellness.
Nutrition shapes everything from your blood pressure and cholesterol to your body’s ability to transport oxygen during a workout. A heart healthy eating plan rich in nutrients, antioxidants, and balanced macronutrients supports efficient blood circulation and protects your arteries. Meanwhile, poor dietary choices can lead to chronic inflammation, sluggish recovery, and increased risk of congestive heart disease. In the context of athleticism or rehabilitation, this makes diet not only a preventative tool but a performance-enhancing strategy. By choosing foods that align with the best diet for cardiovascular health, you’re empowering your body to go further—and your heart to last longer.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice
Fueling Endurance: The Science Behind the Best Heart Healthy Diet
Sustaining energy over long distances, intense workouts, or prolonged activity requires more than carbohydrates alone. The best heart healthy diet balances complex carbs with unsaturated fats and high-quality proteins to fuel your body efficiently. Omega-3 fatty acids—found in walnuts, chia seeds, and salmon—are key players in improving heart rate variability and reducing exercise-induced inflammation. Likewise, nitric oxide-rich vegetables like arugula, spinach, and beets help widen blood vessels, enhancing oxygen delivery to muscles under exertion. These physiological benefits translate directly to better stamina and less fatigue.
A diet for cardio endurance must also consider minerals like magnesium and potassium, which play vital roles in muscle contraction and hydration. Leafy greens, sweet potatoes, and lentils not only nourish the heart but also aid in fluid balance, a key factor in high-performance training. Adopting these elements into a heart healthy meal plan creates a nutritional ecosystem where every bite supports your cardiovascular function. It’s not about a one-time fix—it’s about consistent, intentional choices that align with your body’s energy demands.

Reducing Sodium Without Reducing Satisfaction: The Power of a Heart Healthy Low Sodium Diet
For both athletic individuals and heart failure patients, reducing sodium intake is a non-negotiable step toward better heart health. High sodium levels are known to increase blood pressure and fluid retention, both of which can put undue strain on the heart. Adopting a heart healthy low sodium diet isn’t about bland meals—it’s about smarter seasoning. Fresh herbs, lemon juice, garlic, and peppercorns can bring complexity to dishes without compromising your cardiac goals.
Those following a chronic heart failure diet must be even more vigilant. Processed foods often contain hidden sodium that exacerbates swelling, fatigue, and poor circulation. Whether you’re recovering from a cardiovascular event or training at high intensity, managing salt intake improves not only long-term health but also daily performance. With proper planning, a low sodium heart diet becomes less of a restriction and more of a refined lifestyle choice. The result is less water retention, better blood flow, and more energy to meet your goals.

The Recovery Advantage: How Heart Healthy Meal Plans Support Healing and Strength
Every athlete knows that progress happens during recovery. The body needs time—and nutrients—to rebuild stronger than before. For this reason, heart healthy meal plans must extend beyond performance fuel and include recovery support. After intense activity or cardiac strain, antioxidants like vitamin C, polyphenols, and selenium help reduce muscle damage and protect cardiovascular tissues. Foods like blueberries, dark chocolate, and tomatoes aren’t just delicious—they’re vital to your post-exercise regimen.
Protein intake also plays a key role. Lean sources like tofu, lentils, and skinless poultry provide amino acids that repair muscle fibers while being gentle on the heart. Incorporating these into a heart failure diet ensures that healing occurs without overburdening an already compromised cardiovascular system. Even for non-athletes, especially those recovering from events like heart attacks, healthy eating after a heart attack must focus on nutrient-rich, anti-inflammatory foods. This holistic approach helps reduce complications, accelerates healing, and rebuilds strength with every meal.

Designing a Performance-Based Cardiovascular Diet Plan
Unlike fad diets that focus on calorie-cutting, a cardiovascular diet plan is rooted in functionality. It considers the body’s need for endurance, energy regulation, and cellular health. Before a workout, a balanced meal such as oatmeal topped with berries and flaxseed can deliver sustained energy. During long endurance sessions, portable snacks like bananas or homemade energy bites offer a quick glucose boost without spiking blood sugar. Post-workout, replenishing glycogen and supporting muscle recovery with dishes like quinoa bowls or chickpea salads aligns with both athletic needs and the best diet for heart health.
For those aiming to lose weight while managing heart issues, a cardiac diet for weight loss must delicately balance reduced calories with optimal nutrition. This is particularly important for those wondering how to lose weight with heart failure. High-volume, low-calorie foods such as vegetables, legumes, and lean proteins support satiety while minimizing cardiovascular stress. Whether you’re training for a race or following a congestive heart failure diet, this personalized and purposeful approach can dramatically improve results.
Living with Heart Failure: What Is the Appropriate Diet for a Heart Failure Patient?
A heart failure diagnosis brings not just emotional stress but complex dietary considerations. For these patients, the question of what is the appropriate diet for a heart failure patient is paramount. A comprehensive heart failure nutrition plan involves limiting sodium to reduce fluid buildup, avoiding saturated fats, and increasing potassium to balance electrolytes. At the same time, maintaining sufficient caloric intake is crucial to avoid muscle wasting and fatigue.
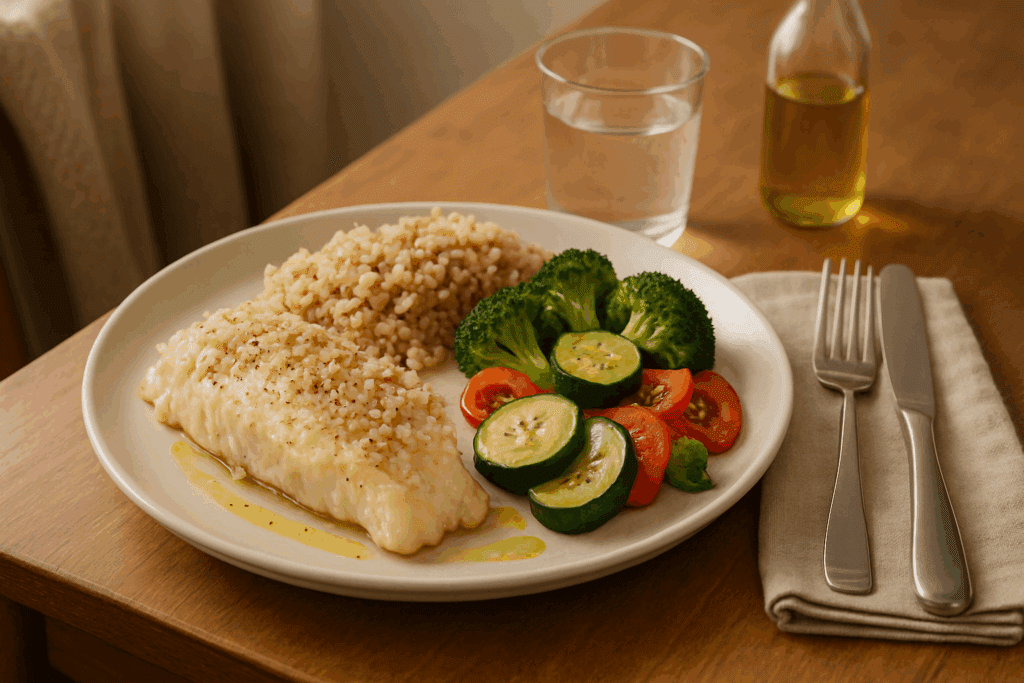
Practical implementation of a heart diet plan includes meals like grilled vegetables with olive oil, brown rice pilaf, or baked white fish with lemon and herbs. These meals are satisfying, flavorful, and align with a congestive heart disease diet. By focusing on nutrient-dense foods and eliminating processed, salty items, patients can support cardiac output and reduce readmission rates. Over time, such a regimen helps stabilize symptoms, improve quality of life, and extend longevity.
Creating Long-Term Success: How to Create a Handout for a Diet for a Healthy Heart
Healthcare providers often empower patients by helping them create handouts for a diet for a healthy heart. These resources distill essential information into manageable steps: what to eat, what to limit, and how to portion meals. A good handout doesn’t just list restrictions; it offers substitution ideas, meal plans, and motivational tips that make behavior change feel achievable.
For example, a handout might recommend swapping white bread for whole grain varieties or replacing red meat with lentils. It could explain how much sodium for a heart healthy diet is appropriate—usually less than 1,500 to 2,300 mg per day, depending on the patient’s condition. Tools like these help individuals transition from a cardiac diet in hospital settings to sustainable home practices. They’re especially valuable for those managing a coronary heart disease diet or returning home post-heart attack.

Understanding the Cardiac Diet Menu Plan and the 3 Day Heart Association Diet
A common question among newly diagnosed patients and fitness-conscious individuals alike is: what is a cardiac diet menu plan? It’s a structured outline of meals that support cardiovascular health through strategic food selection. It typically includes three balanced meals a day with one or two snacks, emphasizing whole foods and low sodium content. For instance, breakfast might be steel-cut oats with berries and flax seeds, while lunch could feature grilled salmon with quinoa and arugula.
Short-term interventions like the 3 day heart association diet can serve as jump-starts. While not meant for long-term use, they offer a quick way to reduce sodium, manage cholesterol, and build dietary momentum. Such tools should always be used under guidance, especially for those already following a cad diet or coping with heart failure. When combined with long-term meal planning, they provide a useful structure for beginning or refining a heart healthy eating plan.
Frequently Asked Questions: Optimizing Cardiovascular Health and Performance Through Diet
1. How can heart healthy meal plans be adapted for high-performance athletes? Heart healthy meal plans can absolutely meet the nutritional demands of high-performance athletes when designed with intention. Unlike generic plans, these diets can be strategically adjusted to increase complex carbohydrates, heart-healthy fats, and lean proteins to fuel longer training sessions without compromising cardiovascular health. Athletes may benefit from nitrate-rich vegetables like beetroot and arugula, which support oxygen delivery, and omega-3s that reduce inflammation post-workout. For those recovering from injury or surgery, incorporating elements of a cardiac diet plan can support vascular healing while maintaining performance. Overall, the flexibility of a cardiovascular diet plan means it can support athleticism while minimizing long-term cardiac strain.
2. What’s the difference between a cardiac diet in hospital settings and a long-term heart diet plan at home? A cardiac diet in hospital environments is typically more restrictive and medically controlled, designed to stabilize patients post-cardiac event. It emphasizes low sodium, limited fluid intake, and reduced saturated fats. In contrast, a long-term heart diet plan evolves with the individual’s health progress and lifestyle. It often incorporates broader nutritional goals like increasing fiber, introducing more plant-based meals, and integrating sustainable cooking habits. While the hospital version initiates dietary change, the at-home model personalizes it into a lifelong heart healthy eating plan.
3. Can the 3 day heart association diet be used regularly or long-term? The 3 day heart association diet is not designed for continuous use but can be a helpful reset for those needing structure to kickstart lifestyle change. It’s effective in temporarily reducing sodium and cholesterol levels, and it helps people build awareness of portion sizes and food choices. However, it’s best used under medical supervision, particularly for individuals on a chronic heart failure diet or those recovering from cardiac surgery. For sustainable health improvements, transitioning to the best heart healthy diet with varied, nutrient-dense foods is more effective. Using the short-term plan as a stepping stone toward a full cardiovascular diet plan ensures both safety and success.
4. How much sodium for a heart healthy diet is considered safe? The general recommendation is to consume no more than 1,500 to 2,300 mg of sodium per day, depending on age, medical history, and activity level. For individuals following a congestive heart failure diet or a coronary heart disease diet, staying closer to the 1,500 mg mark is often advised. It’s important to be aware that most sodium doesn’t come from the salt shaker, but from processed and packaged foods. Reading nutrition labels and preparing meals at home using whole ingredients is the most effective way to follow a low sodium heart diet. Over time, the palate adjusts, and many people find they prefer the nuanced flavors of herbs and spices over salt.
5. What should be included when you create a handout for a diet for a healthy heart? An effective handout should go beyond just listing “good” and “bad” foods. It should include practical meal examples, easy-to-follow cooking tips, and guidance on how to balance meals using the principles of the best diet for cardiovascular health. Including grocery shopping lists, label reading strategies, and sodium-swapping ideas makes the advice actionable. It should also provide information on how to build meals for different health goals, whether someone needs a cardiac diet for weight loss or a diet for cardio performance. Visual tools, such as plate diagrams or portion charts, can make the heart healthy meal plan more approachable.
6. How can someone stick to a heart failure diet when traveling or dining out? Following a heart failure diet while away from home requires planning but is absolutely manageable. Choosing grilled over fried items, requesting no added salt, and prioritizing steamed vegetables are simple ways to stay on track. Bringing heart healthy snacks, like unsalted nuts or fresh fruit, can prevent impulse eating. Many restaurants now offer lower-sodium or heart-healthy menu sections, making it easier to follow a chronic heart failure diet on the go. By maintaining awareness and making informed choices, individuals can uphold the best diet for heart health even in less controlled environments.
7. What role does psychological support play in maintaining a heart healthy eating plan? Changing long-standing eating habits can be emotionally taxing, especially after a life-altering diagnosis like congestive heart failure. Psychological support—from therapists, group counseling, or online communities—can help individuals navigate the stress, grief, or frustration that may accompany dietary change. Emotional eating, food guilt, and resistance to new habits are common barriers that can derail a heart diet plan. By addressing the mental and emotional aspects of dietary transition, patients are more likely to stick to a heart failure nutrition regimen. Building a support system around the best heart healthy diet allows individuals to feel less isolated and more empowered.
8. How can a diet for cardio fitness differ from a coronary heart disease diet? While both diets focus on heart protection, a diet for cardio fitness emphasizes fuel efficiency, muscle recovery, and hydration alongside cardiovascular health. In contrast, a coronary heart disease diet is often more restrictive, aiming to reduce plaque buildup and prevent further complications. For example, athletes might consume more natural sugars and starches for quick energy, while those managing heart disease may avoid these in favor of blood sugar stability. The best diet for heart health can be adapted to serve both populations, but the priorities and caloric needs differ significantly. A personalized cardiovascular diet plan ensures optimal results for either scenario.
9. Is it possible to integrate cultural and family food traditions into a heart healthy low sodium diet? Absolutely. A heart healthy low sodium diet does not require abandoning cultural traditions—it requires adapting them. Many traditional dishes can be reimagined using less salt and healthier cooking methods. For instance, using herbs, citrus, or vinegar in place of salted sauces can retain flavor while meeting the needs of a cardiac diet plan. Including family members in the process also improves compliance and creates a shared health goal. This approach not only supports adherence to a congestive heart disease diet but also promotes heart healthy meal plans that respect personal identity and cultural heritage.
10. What innovations are emerging in cardiac diet planning and technology? The intersection of digital health and nutrition is revolutionizing the way people approach the best diet for cardiovascular health. Mobile apps now track sodium intake, suggest heart healthy recipes, and provide real-time feedback on grocery choices. Wearable tech that monitors heart rate variability and hydration status can inform meal timing for those on a diet for cardio performance. Personalized nutrition platforms are also gaining traction, using genetic testing to tailor a heart failure diet based on metabolism and inflammation markers. These innovations make it easier than ever to implement a sustainable heart diet plan, especially for younger generations more comfortable with tech. As AI and telehealth continue to advance, access to expert-guided heart healthy eating plans is becoming more widespread and user-friendly.
Conclusion: Investing in Performance and Longevity with the Best Diet for Cardiovascular Health
When it comes to endurance, recovery, and lifelong well-being, food is more than fuel—it’s a powerful therapeutic tool. A heart healthy eating plan built around unprocessed, nutrient-dense foods can elevate physical performance while reducing the risk of long-term heart disease. Athletes, patients recovering from cardiac events, and individuals seeking improved health outcomes all benefit from aligning their nutrition with the best heart healthy diet available.
Whether you’re exploring a coronary heart disease diet, transitioning from a cardiac diet in hospital care, or looking to personalize your cardiovascular diet plan for performance, the principles remain the same: reduce sodium, embrace whole foods, balance your plate, and stay consistent. With intention, education, and ongoing support, every individual has the capacity to turn daily meals into heart-supporting medicine. In doing so, you not only improve your cardiovascular resilience—you build a foundation for a longer, stronger, and more vibrant life.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Foods, Diets, and Tips to Follow for a Healthy Heart

