Rethinking Cardiovascular Resilience in a Modern World
In an age where cardiovascular disease remains the leading cause of death worldwide, it’s clear that traditional strategies need refinement. While managing cholesterol, blood pressure, and weight are crucial, the time has come to introduce a new approach to prevent heart attacks—one rooted in proactive performance enhancement, metabolic balance, and whole-body resilience. For decades, heart health was synonymous with restrictive living: less fat, fewer calories, more medication. But science is now painting a more empowering picture—one where endurance training and nutritional precision not only protect the heart but optimize it.
This shift doesn’t mean abandoning medical guidance; it means augmenting it. Modern cardiologists and sports scientists now recognize that improving heart health is not just about surviving but thriving. When we rethink the heart not just as a pump, but as a dynamic, trainable muscle, we unlock new ways to protect against heart attacks through smarter, more strategic methods. Endurance and nutrition, when practiced with intention, become potent tools for long-term cardiovascular resilience.
You may also like: Smart Nutrition Choices for a Healthier Lifestyle: What to Know About Whole Grain Rice and Whole Wheat Rice

Endurance Training as a Cardiovascular Shield
Endurance training has long been associated with aerobic fitness, but its effects go far beyond VO2 max. Emerging research shows that regular, moderate-to-intense cardiovascular exercise can induce structural and functional changes within the heart muscle itself. The left ventricle becomes more efficient, stroke volume improves, and resting heart rate drops—hallmarks of a well-conditioned cardiovascular system. These adaptations are not cosmetic; they represent the body’s natural defense system against the precursors of cardiac arrest.
Yet, not all endurance is created equal. Smarter endurance training doesn’t mean running yourself into exhaustion; it means calibrating intensity, duration, and frequency to build resilience without creating stress overload. This balance is critical. Overtraining or relying on high-intensity intervals exclusively can backfire by increasing systemic inflammation and cortisol levels—both of which can heighten cardiovascular risk in the long term. The key is progressive overload, interspersed with recovery, and diversified movement patterns that challenge different energy systems. This new approach to prevent heart attacks leverages both science and sustainability.
Moreover, heart rate variability (HRV), a key marker of autonomic nervous system health, improves dramatically with strategic endurance training. Higher HRV is associated with a lower risk of sudden cardiac events and reflects a body that can adapt to internal and external stressors with ease. This adaptability is one of the most overlooked tools in a new way to protect against heart attacks. Instead of seeing training as punishment, it’s time to see it as preparation—for longevity, for strength, and for heart-smart living.

The Metabolic Link Between Nutrition and Cardiac Endurance
Nutrition is not simply fuel—it’s information. The nutrients we consume send molecular messages that regulate inflammation, vascular tone, oxidative stress, and mitochondrial efficiency. These factors are central to heart health, particularly in the context of endurance training. What we eat can determine whether the body recovers or breaks down. This is why a new way to prevent heart attacks must include nutritional strategies tailored to both energy demand and metabolic stability.
First and foremost, the overconsumption of refined carbohydrates and industrial seed oils has created an epidemic of insulin resistance and endothelial dysfunction—two major contributors to plaque formation and arterial rigidity. By contrast, diets rich in omega-3 fatty acids, antioxidants, polyphenols, and complex carbohydrates support nitric oxide production, reduce systemic inflammation, and enhance blood flow. These changes are not subtle; they directly impact one’s ability to train longer, recover faster, and reduce cardiovascular strain.
Additionally, nutrition periodization—an advanced concept in sports science—aligns macronutrient intake with training intensity and recovery phases. For example, increasing complex carbohydrate intake during high-intensity weeks supports glycogen replenishment and performance, while emphasizing healthy fats and lean protein during lower-intensity or rest periods supports metabolic flexibility. This fluid approach acknowledges that the body’s needs are not static. By adopting nutritional strategies that evolve with physical demand, we embody a new approach to prevent heart attacks that is dynamic, rather than dogmatic.
Micronutrient sufficiency also plays a critical role. Magnesium, potassium, and coenzyme Q10 are essential for electrical stability in the heart, especially under physical stress. Deficiencies in these nutrients can go unnoticed until arrhythmias or blood pressure dysregulation occur. Through both food and smart supplementation, we can proactively correct these imbalances before they manifest as clinical conditions. This layered, preventative mindset is central to a new way to protect against heart attacks that goes beyond emergency medicine and into everyday empowerment.

Recovery and Autonomic Nervous System Mastery
Endurance and nutrition are only part of the picture. Recovery, especially as it relates to autonomic balance, plays a decisive role in cardiovascular protection. The sympathetic and parasympathetic branches of the nervous system regulate heart rate, blood pressure, and vascular tone. When the body is chronically in fight-or-flight mode—due to stress, poor sleep, or overtraining—the heart becomes more vulnerable to arrhythmias, inflammation, and eventual failure.
What many miss is that rest is not a passive process—it’s active adaptation. Sleep quality, meditation, breathing exercises, and even cold exposure or contrast therapy can stimulate parasympathetic dominance, leading to better recovery and more stable cardiac output. Practices like heart-focused breathing (where exhalation is emphasized) have been shown to lower blood pressure and improve HRV. These are simple yet profound habits that build a heart capable of handling both physical and emotional stress.
One of the most overlooked facets of this new way to prevent heart attacks is the integration of recovery metrics into training programs. Tools like wearable trackers, biofeedback apps, and sleep scoring allow individuals to align effort with recovery in real time. Instead of pushing through fatigue, this data-informed approach emphasizes smarter progression and a deep respect for physiological rhythms. This is not merely about self-care—it’s about cardiovascular literacy in action.
Moreover, chronic inflammation—often stemming from poor gut health, unmanaged stress, and inadequate recovery—can degrade arterial flexibility and provoke immune responses that lead to atherosclerosis. Anti-inflammatory practices such as consuming polyphenol-rich foods (berries, olive oil, turmeric), optimizing sleep hygiene, and maintaining circadian rhythm coherence are foundational in this regard. These strategies reinforce a new way to protect against heart attacks that blends technology, biology, and mindfulness.
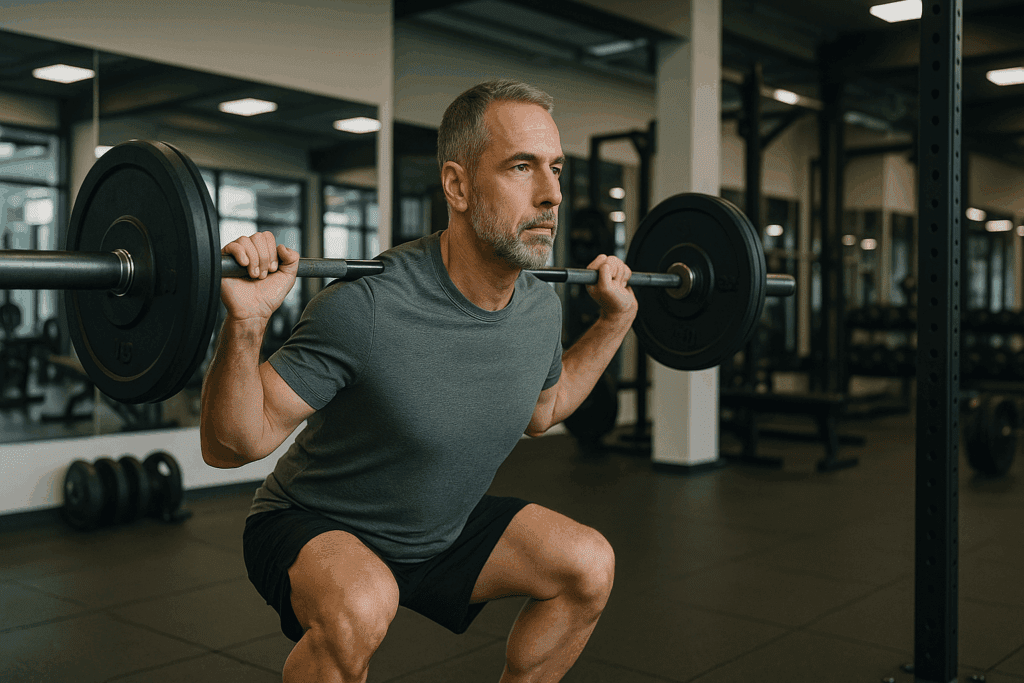
Strength Training as Cardiovascular Insurance
While endurance training improves cardiovascular efficiency, strength training is the unsung hero of heart health. Resistance work enhances insulin sensitivity, builds lean mass, and reduces the mechanical burden on the heart by improving movement economy and postural alignment. Particularly for older adults, maintaining muscle mass is directly linked to lower mortality and better cardiovascular outcomes.
But strength training’s role in a new approach to prevent heart attacks extends beyond physiology. It improves bone density, joint integrity, and metabolic rate—all of which indirectly reduce cardiovascular risk. Moreover, compound lifts like squats and deadlifts engage large muscle groups and stimulate systemic adaptations that translate into better glucose regulation and fat oxidation.
Importantly, strength training supports cardiovascular remodeling in a balanced way. Unlike the chronic stress sometimes induced by excessive cardio, resistance training allows for hormonal recalibration. Growth hormone and testosterone levels improve, both of which have cardioprotective effects when maintained within healthy ranges. In other words, lifting weights isn’t just for aesthetics—it’s for arterial health and metabolic resilience.
A comprehensive training plan that includes resistance training at least two to three times per week, in combination with aerobic and flexibility work, represents a new way to protect against heart attacks that is holistic, efficient, and accessible to people across age groups and fitness levels.

Gut Health and the Cardiovascular Connection
One of the most intriguing frontiers in cardiovascular medicine involves the gut microbiome. An imbalance in gut flora, known as dysbiosis, is now linked to increased risk of hypertension, metabolic syndrome, and inflammatory heart disease. This connection is mediated through metabolites such as TMAO (trimethylamine N-oxide), which has been shown to increase plaque accumulation in arteries.
Restoring gut integrity through prebiotic and probiotic-rich foods like fermented vegetables, kefir, fiber-dense legumes, and polyphenol-rich fruits improves not only digestion but also cardiovascular markers. A healthy microbiome supports optimal cholesterol metabolism, modulates immune response, and even impacts blood pressure regulation.
This emerging field reinforces a new approach to prevent heart attacks that views the body as an integrated ecosystem. By supporting gut health, we support the heart—not in isolation, but as part of a network of interrelated systems. It’s an elegant, systems-based perspective that aligns with the evolving understanding of preventive cardiology.
Functional Testing and Personalized Optimization
No two hearts are the same, and no prevention strategy should be either. Functional medicine and performance diagnostics are revolutionizing how we assess cardiac risk. Tools such as advanced lipid panels, coronary calcium scoring, metabolic flexibility testing, and inflammatory marker profiling allow for early detection and individualized strategies.
Instead of waiting for symptoms to appear, this data-driven approach enables targeted interventions. For example, someone with a genetic predisposition to high Lp(a) levels may require different dietary and pharmacological support than someone whose primary issue is insulin resistance. Personalization is not a luxury—it’s a necessity in any effective, new way to protect against heart attacks.
Moreover, performance testing (such as lactate threshold assessments or VO2 max evaluations) can guide training plans that are not only performance-enhancing but also cardioprotective. When we understand an individual’s unique physiological response to effort, we can fine-tune intensity zones that stimulate adaptation without overreaching. This is how we transition from generic advice to elite-level precision—accessible to anyone willing to listen to their data.

Long-Term Adherence and Lifestyle Design
Perhaps the most overlooked factor in cardiovascular prevention is adherence. The best strategy is the one you’ll stick to. That means crafting a lifestyle—rather than a temporary regimen—that supports consistent training, enjoyable eating, meaningful rest, and stress mastery. This lifestyle must feel sustainable, flexible, and empowering—not rigid or fear-based.
Simplicity matters. Walking regularly, cooking at home, prioritizing sleep, lifting twice a week, and staying hydrated may sound mundane, but these habits compound over time. Layering in occasional performance peaks, retreats, or challenges keeps the process exciting without sacrificing balance. This is the ethos of a new approach to prevent heart attacks: intelligent consistency, not perfection.
Moreover, social connection, purpose, and mindset play powerful roles in cardiovascular resilience. People who maintain strong social ties and a sense of meaning live longer, healthier lives. Emotional wellbeing is not secondary to heart health—it’s central. As we design lives that support endurance and vitality, we find that the best medicine often lies in how we live, love, and lead.
Frequently Asked Questions (FAQ): Boosting Endurance and Heart Health
1. How can psychological stress impact heart health even when someone exercises regularly?
Even with consistent physical activity, unmanaged psychological stress can silently undermine cardiovascular health. Chronic stress triggers the release of cortisol and adrenaline, which, over time, may contribute to high blood pressure, endothelial dysfunction, and increased arterial inflammation. These biochemical changes can override the benefits of exercise if left unchecked. Adopting a new approach to prevent heart attacks includes understanding the impact of emotional regulation and stress reduction techniques such as breathwork, meditation, or cognitive behavioral therapy. Without addressing stress holistically, even the best endurance plan might fail to serve as a new way to protect against heart attacks.
2. What role does environmental exposure play in cardiovascular endurance and heart disease risk?
Air pollution, exposure to industrial toxins, and even heavy metals in water or food can negatively influence heart health. Long-term exposure to these environmental factors has been linked to increased oxidative stress and inflammation—both major contributors to heart disease. For individuals pursuing a new way to prevent heart attacks, reducing environmental risk by using HEPA filters, avoiding ultra-processed foods, and prioritizing clean hydration sources is critical. These steps complement training and nutrition by reducing the systemic burden on the body. This adds another layer to a new approach to prevent heart attacks, one that integrates personal and planetary health.
3. How do wearable technologies contribute to smarter cardiovascular training?
Wearable devices now offer real-time data on heart rate variability, sleep quality, and exertion levels, allowing individuals to tailor their training with precision. This biofeedback helps avoid overtraining and supports more informed recovery strategies. Integrating wearables into your routine is a new way to protect against heart attacks by detecting red flags before they escalate into real problems. It empowers people to shift from reactive to proactive heart health. As technology advances, using devices intelligently becomes central to a new approach to prevent heart attacks.
4. Why is metabolic flexibility important for heart protection and endurance?
Metabolic flexibility refers to the body’s ability to efficiently switch between using carbohydrates and fats for energy, depending on demand. This capacity not only enhances athletic performance but also reduces the buildup of oxidative byproducts that can stress the heart. Supporting metabolic flexibility through fasting protocols, carbohydrate periodization, and anti-inflammatory nutrition is a cornerstone of a new way to prevent heart attacks. Athletes and non-athletes alike benefit from this metabolic resilience, especially in high-stress or high-demand situations. Enhancing this capacity offers a nuanced, functional approach to long-term heart health.
5. Can social connection really influence cardiovascular outcomes?
Surprisingly, yes. Loneliness and social isolation are now recognized as significant risk factors for heart disease—on par with smoking and obesity. Deep, meaningful connections stimulate parasympathetic activity, lower resting heart rate, and promote hormonal balance. Building community and prioritizing social health are essential aspects of a new approach to prevent heart attacks that often go overlooked. A new way to protect against heart attacks includes not only what you eat or how you train, but also who you connect with and how you live emotionally.
6. How do circadian rhythms affect cardiovascular performance and repair?
The heart, like every other organ, functions according to circadian rhythms. Disruptions from shift work, excessive screen time at night, or inconsistent sleep patterns can impair blood pressure regulation and vascular repair. Optimizing sleep timing and aligning training with daylight exposure support a more robust cardiovascular profile. Embracing circadian health is a subtle yet powerful part of a new approach to prevent heart attacks. Recovery and adaptation happen during rest, and aligning with natural cycles enhances those benefits.
7. Are there specific breathing techniques that support heart health?
Yes—techniques such as box breathing, diaphragmatic breathing, and coherent breathing (e.g., 5 seconds in, 5 seconds out) help activate the parasympathetic nervous system. This reduces resting heart rate, lowers blood pressure, and improves heart rate variability over time. Integrating these techniques into daily life represents a new way to protect against heart attacks that doesn’t require a gym or fancy equipment. They serve as accessible, scalable tools for nervous system regulation and cardiovascular balance. Regular practice reinforces a new approach to prevent heart attacks that prioritizes internal stability.
8. How can travel or frequent time zone changes influence cardiovascular endurance?
Jet lag and frequent travel disrupt circadian timing, meal timing, and sleep cycles—key components of cardiovascular stability. These disruptions can cause temporary spikes in blood pressure and inflammation, especially in those with preexisting risk factors. To counteract this, smart travelers adopt light exposure strategies, hydration protocols, and strategic meal timing to re-anchor biological rhythms. These adjustments reflect a new approach to prevent heart attacks that adapts wellness strategies to modern lifestyles. It’s a new way to protect against heart attacks that values flexibility and foresight.
9. What innovations in cardiology could reshape prevention strategies in the next decade?
Emerging tools like continuous glucose monitors, advanced lipid particle testing, AI-driven diagnostics, and gut-heart axis mapping are already transforming care. These innovations allow clinicians to detect risk patterns earlier and personalize interventions more accurately. As access to these tools improves, a new way to prevent heart attacks will become more personalized, data-driven, and precise. Integrative and functional medicine approaches will likely merge with mainstream cardiology to offer layered prevention models. This represents not just progress, but a fundamentally new approach to prevent heart attacks for the 21st century.
10. How does mindset influence the effectiveness of heart health strategies?
Mindset acts as the filter through which all health strategies succeed or fail. A rigid, fear-based approach often leads to burnout, while a growth-oriented mindset fosters consistency and resilience. Viewing heart health as an opportunity to thrive—not just avoid illness—creates psychological momentum. A new way to protect against heart attacks includes cultivating optimism, adaptability, and long-term thinking. This mindset shift is foundational to embracing a new approach to prevent heart attacks that feels empowering rather than burdensome.
Conclusion: Embracing a Smarter, Stronger Path to Heart Health
Preventing heart attacks isn’t just about lowering numbers on a lab report—it’s about building a life that fortifies the heart from the inside out. With smarter training, targeted nutrition, and holistic recovery strategies, we now have a new way to protect against heart attacks that is proactive, empowering, and scientifically sound. This approach doesn’t rely on fear or deprivation. Instead, it focuses on building capacity—cardiovascular, metabolic, emotional, and physical.
We are at the frontier of a performance-based cardiology, where the line between fitness and health dissolves. By weaving together endurance, strength, functional nutrition, gut health, and precision testing, we create a system that not only protects but optimizes. This isn’t a temporary fix; it’s a lifelong evolution.
The heart is not fragile—it’s adaptive. When we treat it with respect, train it with intention, and nourish it with wisdom, it becomes our greatest asset in the pursuit of a vibrant, enduring life. This is the promise and power of a new approach to prevent heart attacks. And it starts with a single step, taken mindfully and repeated consistently, in service of something greater than mere survival—thriving in every heartbeat.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Lifestyle Changes to Prevent a Heart Attack
Strategies to prevent heart disease
Effects of Exercise to Improve Cardiovascular Health
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.

