The evolving landscape of modern healthcare is increasingly recognizing the critical intersection of nutrition and mental health. Once viewed as separate domains, the fields of dietetics and psychology are now converging in both research and clinical practice. In recent years, scientists have discovered a profound relationship between food and mental health, leading to a deeper understanding of how eating habits can shape emotional stability, cognitive clarity, and psychological resilience. Whether addressing chronic stress, depression, anxiety, or overall well-being, the role of diet is more pivotal than ever. Understanding how nutrition and mental health are intertwined is not merely a matter of curiosity; it’s a crucial piece of the wellness puzzle that affects how we feel, think, and function on a daily basis.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
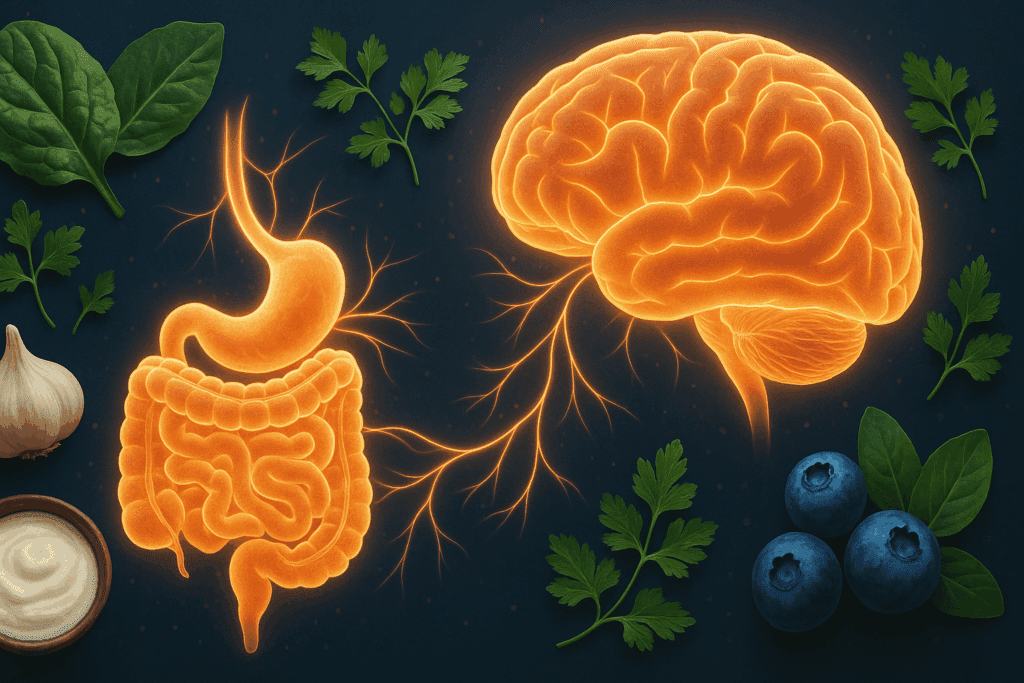
Modern studies consistently demonstrate that what we consume doesn’t just affect our bodies—it profoundly impacts our minds. As people begin to ask, “How does nutrition affect mental health?” or “Does diet affect mental disorder symptoms?” the answers are becoming clearer through the lens of emerging scientific evidence. From the gut-brain connection to the influence of micronutrients on neurotransmitter regulation, the mechanisms through which food affects our mental landscape are multifaceted and compelling. In this context, exploring the six benefits of mental health for nutrition allows us to appreciate how a well-balanced diet serves as a powerful tool for emotional wellness.
Why Is Eating Well Good for Mental Health?
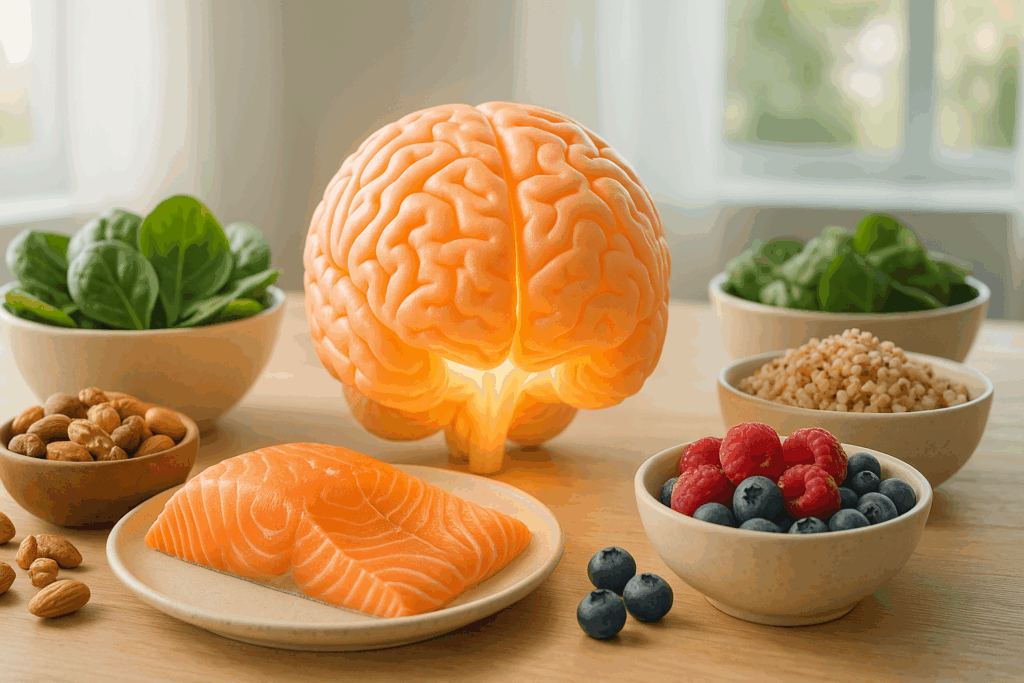
Eating well provides the brain with the essential nutrients required to function optimally. Just like the body needs fuel to run, so does the brain. Whole foods rich in vitamins, minerals, antioxidants, and healthy fats support the brain’s structure and biochemical processes. For instance, omega-3 fatty acids found in fatty fish have been shown to reduce symptoms of depression and anxiety. Similarly, complex carbohydrates from whole grains help stabilize blood sugar levels, contributing to mood regulation.
Diet and psychological health are intricately linked because nutrients influence the production and activity of neurotransmitters like serotonin and dopamine, which are directly tied to feelings of happiness, calm, and motivation. When the body lacks these nutrients, it can result in emotional instability, cognitive impairment, and increased susceptibility to mood disorders. In essence, a nutrient-dense diet builds a biochemical foundation that supports emotional resilience. This is one reason why the mental benefits of nutrition are now being emphasized in both preventative care and mental health treatment strategies.
Furthermore, eating well establishes healthy routines that promote psychological structure and mindfulness. Meal planning, preparing nourishing dishes, and enjoying food in a relaxed setting all contribute to emotional balance. These small rituals can help reduce stress, build a sense of control, and foster a more conscious relationship with the body. Ultimately, understanding what nutrition can do for mental health enables us to adopt eating habits that protect and promote emotional well-being.
How Can Not Eating Affect Your Mental Health?
When we skip meals, restrict food groups, or consume diets that lack essential nutrients, our mental health can suffer significantly. Poor nutrition is not just a risk factor for physical ailments but also a contributor to mental distress. Individuals who do not eat regularly or who consume highly processed, low-nutrient foods often experience mood swings, fatigue, irritability, and concentration problems. This highlights the very real effects on mental health with bad nutrition, which can manifest quickly and sometimes severely.
The human brain is highly metabolically active and requires a constant supply of glucose, amino acids, and micronutrients to function properly. Deprivation of these essentials can impair cognitive performance and emotional regulation. This explains why disordered eating patterns, including those seen in anorexia nervosa or chronic dieting, are strongly associated with increased rates of anxiety and depression. Asking how can not eating affect your mental health leads us to acknowledge the brain’s dependency on regular nourishment.
Beyond physiological consequences, erratic or insufficient eating habits can also trigger psychological stress. The body may interpret food scarcity as a form of chronic stress, activating the hypothalamic-pituitary-adrenal (HPA) axis and raising cortisol levels, which are associated with heightened anxiety. In turn, this creates a feedback loop where stress suppresses appetite or leads to emotional eating, further exacerbating mental health issues. To support emotional wellness, consistent, balanced eating must be recognized as a cornerstone practice.
The Gut-Brain Axis and Its Role in Emotional Wellness
The gut-brain axis has become a focal point of research in understanding the bidirectional relationship between food and mental health. This complex communication network between the gastrointestinal tract and the central nervous system suggests that our gut health can directly influence our mood, behavior, and mental clarity. Beneficial gut bacteria produce neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), which play key roles in emotional regulation. This emerging field helps explain why nutrition and psychological health are so deeply interconnected.
An imbalance in gut microbiota, often caused by poor dietary habits, can contribute to inflammation and neurochemical imbalances linked to depression and anxiety. Diets high in sugar and processed foods reduce microbial diversity and foster the growth of harmful bacteria, while fiber-rich, plant-based foods support a healthy gut ecosystem. This relationship sheds light on why statistics on how diet affects mental health are showing a consistent correlation between poor nutrition and increased prevalence of mental disorders.
Probiotics and prebiotics—found in foods like yogurt, kefir, sauerkraut, garlic, and onions—can help restore gut health and improve mood. These foods support the balance of beneficial microbes, which in turn communicate with the brain to influence emotional states. As the scientific community continues to explore this connection, more evidence supports the idea that dietary changes can complement mental health treatments. Understanding this interplay is essential for anyone seeking to improve emotional wellness through dietary choices.
Six Ways Nutrition and Mental Health Are Linked
Appreciating the six ways nutrition and benefits mental health requires a comprehensive understanding of how different aspects of diet influence various dimensions of mental well-being. First, nutrient-rich diets help regulate neurotransmitter activity, improving mood stability and reducing the risk of depression. Second, balanced meals support blood sugar control, which directly impacts energy levels and emotional consistency. Third, anti-inflammatory foods help reduce systemic inflammation, which has been implicated in mood disorders.
Fourth, a healthy diet fosters improved sleep quality, which is essential for emotional resilience and cognitive function. Tryptophan, found in turkey and other protein-rich foods, aids in melatonin production and supports better sleep hygiene. Fifth, hydration and electrolyte balance—achieved through fruits, vegetables, and adequate water intake—support brain function and reduce irritability and mental fog. Sixth, the act of engaging in mindful eating can promote self-awareness, reduce stress, and create a positive relationship with food. These insights reveal the holistic nature of mental benefits for good nutrition.
By identifying these core benefits, we can reframe dietary habits as a form of mental health care. Rather than viewing nutrition solely through the lens of physical health or weight management, integrating its role in mental well-being transforms how we approach food. For individuals asking how does diet affect mental health near me, these findings offer practical, evidence-based answers that apply across diverse populations and settings.
What Are the Best Foods for Mental Health?
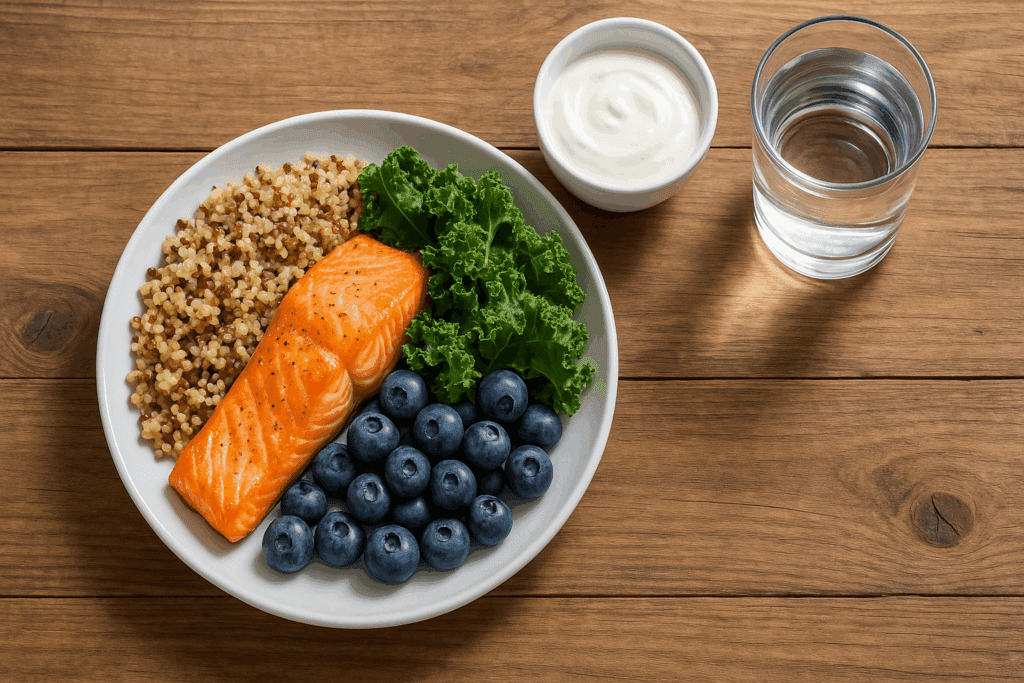
Certain foods stand out for their ability to support mood, focus, and emotional stability. Fatty fish like salmon and mackerel are rich in omega-3 fatty acids, which are crucial for brain development and mood regulation. Leafy greens such as spinach and kale provide folate, which is involved in dopamine production. Nuts and seeds deliver magnesium and zinc, minerals that are essential for managing stress and maintaining cognitive clarity. These are among the best foods for mental health due to their high nutrient density and proven psychological benefits.
Fermented foods like kimchi, miso, and yogurt supply probiotics that enhance gut health, thus positively influencing the gut-brain axis. Whole grains such as quinoa, brown rice, and oats help stabilize blood sugar levels and promote steady energy throughout the day. Berries, rich in antioxidants, help combat oxidative stress in the brain and are associated with lower rates of cognitive decline and depressive symptoms.
It’s also essential to consider the synergy of these foods when consumed together as part of a balanced diet. A Mediterranean-style eating pattern, for example, incorporates many of these components and has been linked to reduced risks of depression and anxiety. When we explore what nutrition can do for mental health, these dietary patterns emerge as both preventive and therapeutic tools for emotional wellness. Making small, intentional changes—such as replacing refined carbs with whole grains or adding a serving of fatty fish each week—can yield significant mental health improvements over time.
How Does Diet Affect Mental Disorder Risk and Recovery?
Understanding how diet and mental health interact is especially important in the context of mental disorder prevention and recovery. Nutritional psychiatry, a growing field that examines the role of diet in mental illness, provides compelling evidence that dietary choices can influence the course and severity of conditions such as depression, anxiety, and even schizophrenia. Although diet is not a cure, it is increasingly being viewed as a complementary strategy that enhances standard treatments like therapy and medication.
Inflammation, oxidative stress, and neurochemical imbalances are biological mechanisms that link poor diet with mental disorders. A pro-inflammatory diet—high in sugar, trans fats, and refined carbohydrates—can exacerbate these processes, leading to worsened symptoms. Conversely, anti-inflammatory foods such as berries, leafy greens, and omega-3s offer protective effects. These findings underscore the mental benefits of nutrition in the prevention and management of psychological illness.
Clinical studies show that patients with depression who adopt healthier eating patterns experience reductions in symptom severity and improved treatment outcomes. This evidence supports the integration of nutritional counseling into psychiatric care. For those wondering does diet affect mental disorder recovery or prognosis, the growing body of literature suggests that it certainly can. Nutrient repletion—such as supplementing B vitamins or addressing iron deficiency—can also alleviate cognitive symptoms like brain fog and fatigue.
Moreover, community-based interventions that include access to healthier foods, cooking education, and support for dietary changes are proving effective in populations with high rates of mental illness. These initiatives highlight how local environments—reflected in questions like how does diet affect mental health near me—can influence mental wellness outcomes. Promoting dietary improvements at the societal level could be a key strategy in reducing the burden of mental health disorders.
What Do the Numbers Say? Key Statistics on Diet and Mental Health
Emerging data consistently reinforces the connection between diet and mental health. Epidemiological studies reveal that individuals who follow diets high in fruits, vegetables, whole grains, lean proteins, and healthy fats have significantly lower risks of depression and anxiety. In contrast, those who consume a Western-style diet rich in processed foods, sugars, and saturated fats exhibit higher rates of mental health issues. These statistics on how diet affects mental health provide a compelling case for nutritional intervention.
For instance, the SMILES trial—a landmark clinical study in nutritional psychiatry—demonstrated that a modified Mediterranean diet significantly reduced depressive symptoms in participants with moderate to severe depression. This controlled trial provided the first robust evidence that dietary improvement could directly affect mood disorder outcomes. Similarly, population studies in countries like Japan and Norway show that traditional diets correlate with better mental health compared to fast-food-heavy Western patterns.
Data also highlights that children and adolescents are especially vulnerable to the mental effects of poor nutrition. Research shows that early dietary habits can influence the risk of developing mental disorders later in life. This has sparked public health initiatives aimed at improving childhood nutrition as a means of long-term mental health promotion. By tracking dietary patterns and mental health outcomes, researchers can better understand the role food plays across the lifespan. These findings contribute to our collective understanding of the diet and psychological health connection and support the integration of nutrition into mental healthcare policies.
A Holistic Understanding of Food and Mental Health
Developing a holistic perspective on food and mental health means acknowledging the full spectrum of how dietary habits affect our emotional and psychological landscape. It’s not only about choosing the best foods for mental health, but also about how we relate to eating as a daily ritual. Nutrition and mental health are mutually reinforcing: when we eat well, we tend to feel better, and when we feel better, we’re more likely to continue making positive food choices.
This feedback loop is vital for individuals working through mental health challenges. Emotional eating, for example, often emerges in response to stress or sadness, leading to poor food choices that compound negative feelings. Building a mindful, nourishing relationship with food can disrupt this cycle. Practicing intuitive eating—tuning into hunger and satiety cues, avoiding restrictive behaviors, and savoring meals—supports both psychological and physiological balance.
Additionally, food environments play a significant role. Access to healthy, affordable food varies across communities, and disparities in nutrition often mirror disparities in mental health. Promoting equity in food systems is therefore not just a matter of physical health—it is also a mental health imperative. Whether through policy, education, or community initiatives, expanding access to nourishing food is a foundational step toward a mentally healthier society.
Frequently Asked Questions (FAQ): Nutrition and Mental Health
How do long-term dietary patterns shape psychological resilience over time?
The connection between long-term diet and psychological resilience is increasingly supported by clinical and epidemiological research. When we examine the six benefits of mental health for nutrition, one standout theme is that dietary consistency plays a crucial role in reinforcing emotional balance and adaptability. Over time, diets high in phytonutrients, omega-3 fatty acids, and complex carbohydrates can improve stress recovery, reduce inflammation, and fortify the gut-brain axis—all key contributors to mental strength. The mental benefits of nutrition unfold gradually, as the cumulative effect of nutrient sufficiency fosters better neurochemical stability. Beyond acute symptom relief, enduring dietary patterns influence the brain’s plasticity and ability to cope with trauma, which highlights the long-range implications of nutrition and psychological health.
Are there overlooked nutrients that significantly impact mood and cognition?
While most people are aware of vitamins like B12 and omega-3s, lesser-discussed nutrients such as choline, selenium, and chromium also have a substantial impact on mood and cognition. Choline, found in eggs and liver, supports acetylcholine production—a neurotransmitter tied to memory and concentration. Selenium, present in Brazil nuts and sunflower seeds, has antioxidant properties that reduce oxidative stress, which is increasingly implicated in mood disorders. Chromium, a trace mineral, helps regulate insulin function, indirectly influencing energy levels and mood stability. These elements illustrate what nutrition can do for mental health when a diverse range of micronutrients is prioritized. Including these lesser-known nutrients reinforces the idea that food and mental health are interconnected in more complex ways than many realize.
What role does cultural diet diversity play in supporting mental well-being?
Cultural dietary diversity is a critical but underappreciated factor in promoting mental well-being. Traditional eating patterns often include a wide array of plant-based and fermented foods that support gut health, contributing positively to both nutrition and mental health. The psychological comfort of cultural familiarity in food also plays a major role in emotional stability, helping individuals feel connected to their identity and community. Recent studies comparing Mediterranean, Japanese, and Nordic diets show a consistent link between culturally rooted nutrition and reduced rates of depression. These findings suggest that diet and mental health outcomes are not only biological but also influenced by social and emotional dimensions of eating. Embracing diverse food traditions could be one of the six ways nutrition and benefits mental health on a population level.
Can poor eating habits during adolescence have long-term psychological consequences?
Absolutely. Adolescence is a pivotal period for brain development, and poor dietary choices during this stage can have lasting effects on mental function and emotional regulation. The effects on mental health with bad nutrition during youth are often underestimated but can result in a higher risk for conditions like anxiety, depression, and ADHD later in life. Research reveals that diets high in sugar and low in essential nutrients impair the formation of critical neural pathways. Moreover, the establishment of unhealthy eating patterns during adolescence tends to persist into adulthood, compounding mental health challenges. Parents and educators should recognize that encouraging healthy food choices in teens isn’t just about physical growth—it’s an investment in their long-term psychological health.
How do restrictive diets or food avoidance patterns influence mood stability?
Restrictive diets, especially those that eliminate entire food groups without medical necessity, can destabilize mood and energy levels. These patterns often lead to deficiencies in vital nutrients such as iron, magnesium, or B vitamins, which are essential for neurotransmitter synthesis and nervous system function. For instance, individuals following extreme low-carb regimens may experience irritability due to reduced serotonin production, as carbohydrates facilitate its release. Understanding how can not eating affect your mental health becomes especially important in this context, as disordered eating behaviors can initiate or worsen emotional distress. Clinicians are beginning to factor in the psychological toll of restrictive diets when evaluating diet and psychological health concerns, underscoring the need for balanced, inclusive eating strategies.
What emerging trends are shaping the future of nutritional psychiatry?
Nutritional psychiatry is quickly gaining momentum as new research and technologies redefine how we view the intersection of diet and psychological wellness. One significant trend is the integration of microbiome analysis into personalized nutrition plans, which tailors food recommendations based on gut bacteria profiles. Another exciting development is the use of nutrigenomics, a field that explores how individual genetic differences affect responses to specific nutrients. These innovations provide deeper insight into how does nutrition affect mental health at a personalized level, making treatment more precise. Additionally, artificial intelligence is being used to analyze large datasets from dietary journals and psychological assessments to predict mental health outcomes, offering an expanded lens through which we understand the mental benefits of nutrition.
How should people interpret local data when asking, ‘How does diet affect mental health near me?’
Local data provides context-specific insights that can help answer how does diet affect mental health near me in ways that national averages cannot. Regional dietary patterns, access to fresh food, and cultural attitudes toward eating all play a role in shaping community-level mental health outcomes. For example, a city with limited access to whole foods but high consumption of processed snacks may show increased rates of depression and cognitive disorders. These statistics on how diet affects mental health at a local level are invaluable for shaping public health initiatives and informing resource allocation. Community gardens, school lunch programs, and urban food policies are all influenced by such data, revealing a crucial connection between diet and mental health that’s rooted in place-based analysis.
Can dietary interventions aid in reducing reliance on psychiatric medications?
While dietary changes should never replace prescribed medication without a clinician’s supervision, emerging evidence shows that nutrition can play a supportive role in reducing reliance on certain psychiatric drugs. In some studies, patients with mild to moderate depression who adopted nutrient-rich diets required lower doses of antidepressants over time. This outcome is closely linked to the mental benefits for of good nutrition, which can enhance baseline emotional stability and reduce the frequency of symptom flare-ups. High-quality diets also mitigate the side effects of medications, such as fatigue or gastrointestinal discomfort, making treatment more tolerable. As nutritional science evolves, healthcare providers are more frequently integrating diet into holistic care plans, reflecting growing awareness of the role food plays in psychiatric treatment.
Why is eating well good for mental health in high-stress professions or environments?
In high-stress professions—such as healthcare, law enforcement, or finance—cognitive performance and emotional regulation are essential. A nutrient-dense diet supports neurotransmitter balance and stress hormone regulation, helping individuals navigate demanding environments with greater composure. The mental benefits of nutrition in such contexts extend to improved focus, faster decision-making, and better sleep quality. Moreover, individuals who consume regular, balanced meals are less likely to experience blood sugar crashes, which can amplify feelings of anxiety or irritability. Recognizing why is eating well good for mental health in these high-pressure settings opens the door to workplace wellness programs that incorporate nutritional strategies as a preventive tool for burnout.
How can educational institutions integrate food and mental health awareness into their curricula?
Educational institutions are uniquely positioned to educate the next generation on the intersection of food and mental health. Integrating this knowledge into health education courses, psychology curricula, and even culinary classes can equip students with life-long wellness tools. Teaching students about the six benefits of mental health for nutrition within a structured academic setting ensures they understand the real-world implications of dietary choices. Schools can also partner with local farms or nutritionists to provide experiential learning opportunities such as school gardens or cooking demonstrations. By embedding nutrition and psychological health education into mainstream academics, institutions can create a ripple effect that promotes long-term mental resilience across communities.
Conclusion: Reframing Nutrition as a Mental Health Strategy
The link between nutrition and mental health is no longer speculative—it is scientifically grounded and deeply compelling. Across cultures, age groups, and clinical populations, the evidence points to a strong, consistent relationship between what we eat and how we feel. From understanding how can not eating affect your mental health to identifying the six benefits of mental health for nutrition, it becomes clear that diet plays a central role in emotional wellness. When we ask questions like how does diet affect mental health near me, the answers often lie not only in clinical studies but also in everyday habits and community resources.
By integrating the mental benefits of good nutrition into healthcare, education, and public policy, we can shift the conversation around mental health toward prevention and empowerment. Dietary change is not a silver bullet, but it is a powerful tool that complements traditional treatments. For anyone seeking a sustainable path toward emotional resilience, food is a profound place to begin. Let this be a call to action: to nourish not only the body but also the mind—one mindful bite at a time.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Diet and Mental Health: How Nutrition Shapes Your Well-Being
Food and mood: how do diet and nutrition affect mental wellbeing?