Binge eating disorder (BED) is a serious and complex mental health condition that affects millions of people across the globe. Characterized by recurrent episodes of consuming unusually large quantities of food in a short period, often accompanied by feelings of shame, guilt, and a lack of control, BED is more than a behavioral issue. It is a diagnosable psychiatric disorder with intricate biological, psychological, and social underpinnings. As understanding of BED has evolved, so too have the treatment strategies. While therapy and nutritional counseling remain foundational, the potential of pharmacological interventions like naltrexone for binge eating and Wellbutrin for binge eating has sparked considerable interest in both clinical and public health communities.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
The conversation around pharmacologic support for binge eating brings together neuroscience, psychology, and lifestyle interventions in ways that illustrate the multifactorial nature of this condition. In this article, we delve into the mechanisms of naltrexone and Wellbutrin, explore their clinical relevance, and examine how they fit within a holistic framework of treatment. By integrating current research, expert insight, and lifestyle context, this discussion aims to provide a thoughtful, medically grounded perspective suitable for a college-educated audience seeking nuanced information.
Understanding the Neurobiology of Binge Eating Disorder
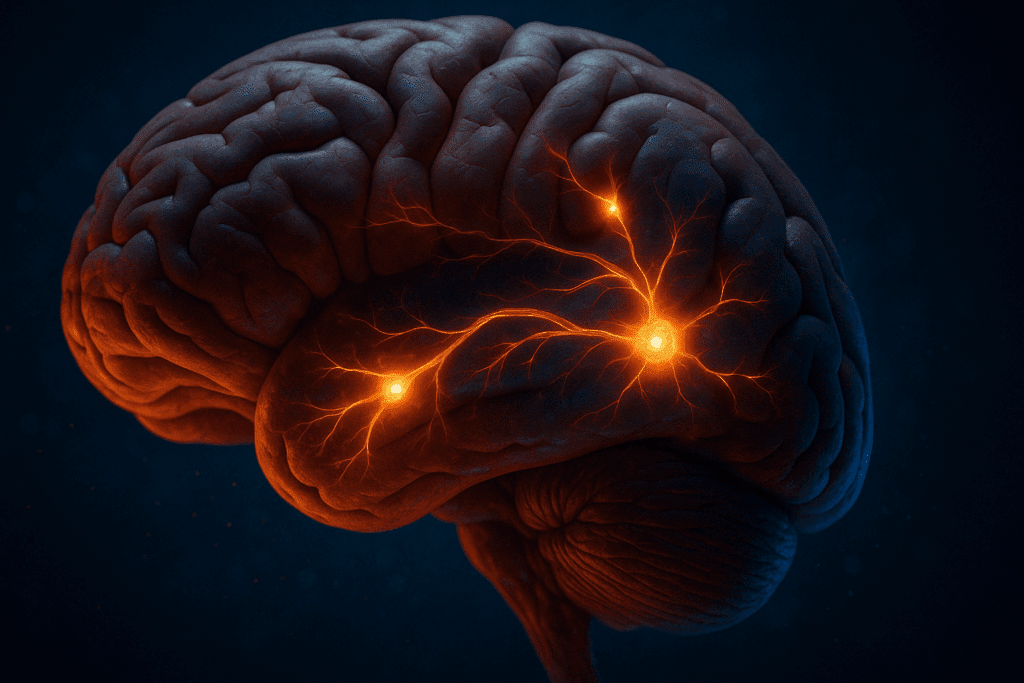
To appreciate how medications like naltrexone and Wellbutrin might help manage binge eating, it’s essential to first understand the neurobiological mechanisms that underlie the disorder. BED is closely tied to disruptions in the brain’s reward circuitry, particularly the dopaminergic pathways. These pathways, which involve areas like the nucleus accumbens and the prefrontal cortex, are implicated in impulsivity, compulsivity, and the pursuit of pleasure—all central to binge eating behavior.
Individuals with BED often exhibit heightened sensitivity to food-related cues and impaired inhibitory control, leading to episodes of compulsive eating. Neuroimaging studies have shown increased activation in the brain’s reward centers when individuals with BED are exposed to images or smells of palatable foods. This neural overactivation is akin to that seen in substance use disorders, reinforcing the notion that BED shares features with addictive behaviors. Consequently, medications that target these neural circuits may offer therapeutic benefit.
Furthermore, BED is often comorbid with other psychiatric conditions such as depression, anxiety, and substance use disorders. These co-occurrences underscore the need for treatments that not only address the eating behavior itself but also the broader emotional and cognitive dysregulation that often accompany it. Naltrexone and Wellbutrin, with their distinct yet complementary pharmacological profiles, have emerged as promising candidates in this regard.
How Naltrexone Works in the Context of Binge Eating
Naltrexone is an opioid antagonist that has traditionally been used in the treatment of alcohol and opioid dependence. By binding to and blocking opioid receptors in the brain, naltrexone inhibits the release of dopamine that typically follows the activation of these receptors. This blunting of the dopamine response reduces the feelings of pleasure and reward associated with addictive substances—and, as research increasingly shows, with highly palatable foods as well.
The rationale for using naltrexone for binge eating stems from its ability to disrupt the hedonic drive that characterizes compulsive eating episodes. In individuals who binge eat, food may trigger a dopamine surge similar to that seen with drugs of abuse. Naltrexone dampens this neurochemical response, thereby reducing the reinforcement that perpetuates the binge cycle.
Clinical studies have begun to explore the efficacy of naltrexone for binge eating. Some randomized controlled trials suggest that naltrexone, particularly when combined with other medications like bupropion (the generic form of Wellbutrin), can lead to significant reductions in binge episodes, food cravings, and emotional eating. The FDA-approved medication Contrave, which combines naltrexone and bupropion, reflects this synergistic approach.
However, naltrexone is not without its limitations. Side effects such as nausea, headache, and fatigue are not uncommon, and its efficacy may vary based on individual neurobiology and the presence of co-occurring mental health conditions. Nevertheless, for certain individuals, particularly those with strong cravings and addictive-like eating patterns, naltrexone can play a valuable role within a comprehensive treatment plan.

The Role of Wellbutrin in Managing Binge Eating Disorder
Wellbutrin, also known by its generic name bupropion, is a norepinephrine-dopamine reuptake inhibitor (NDRI) commonly prescribed for depression and smoking cessation. Unlike selective serotonin reuptake inhibitors (SSRIs), Wellbutrin enhances the availability of dopamine and norepinephrine in the brain—neurotransmitters that play crucial roles in motivation, attention, and mood regulation.
The use of Wellbutrin for binge eating is grounded in its potential to alleviate the low mood and executive dysfunction that often underlie disordered eating patterns. Individuals with BED frequently report depressive symptoms, anhedonia (the inability to feel pleasure), and a lack of energy—all of which can fuel the cycle of emotional eating. By boosting dopamine and norepinephrine, Wellbutrin may help restore motivation and self-regulation, thereby reducing the frequency and severity of binge episodes.
Several clinical trials have evaluated the efficacy of bupropion for weight loss and eating disorders. While results vary, there is a growing body of evidence suggesting that Wellbutrin can contribute to weight reduction and improved mood, particularly when used alongside behavioral therapy. Its dual action on mood and appetite makes it a compelling option for individuals whose binge eating is closely tied to affective dysregulation.
Moreover, when combined with naltrexone, Wellbutrin’s stimulant-like properties may counteract some of the sedative side effects of opioid antagonists. This combination, as seen in Contrave, represents a strategic pharmacologic pairing that addresses both the emotional and reward-driven components of BED. Still, as with any psychiatric medication, the decision to use Wellbutrin should be based on a thorough clinical evaluation and personalized risk-benefit analysis.
Integrating Medication with Lifestyle and Behavioral Interventions
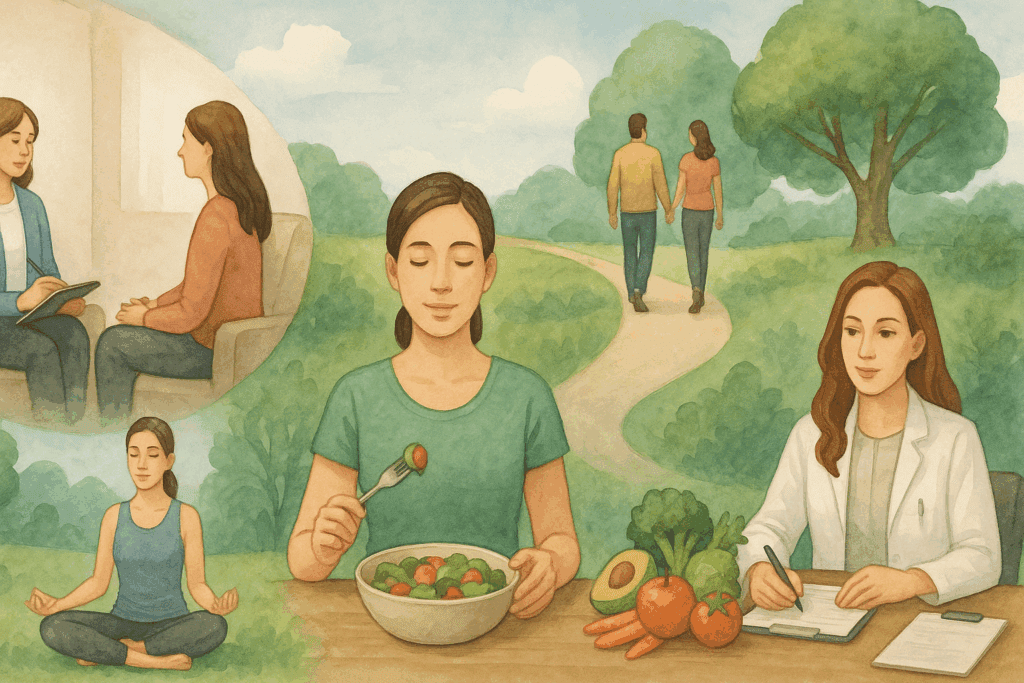
While pharmacological treatments like naltrexone for binge eating and Wellbutrin for binge eating offer promising avenues for symptom management, they are not standalone cures. Lasting recovery from BED often requires a multimodal approach that includes therapy, nutrition education, stress management, and physical activity. Cognitive-behavioral therapy (CBT) remains the gold standard psychological intervention for BED, helping individuals identify and change unhelpful thought patterns and behaviors.
Mindful eating practices can further support this recovery process. By cultivating awareness of hunger and satiety cues, and fostering a non-judgmental relationship with food, individuals can begin to rebuild trust in their bodies and their ability to make nourishing choices. Mindfulness-based interventions have been shown to reduce binge frequency and improve emotional regulation, making them valuable complements to medication.
Nutritional counseling is also essential. Many individuals with BED have a history of chronic dieting, which can contribute to disordered eating patterns and nutritional imbalances. Registered dietitians specializing in eating disorders can help clients develop balanced meal plans that promote satiety, reduce cravings, and support overall health. This holistic perspective ensures that biological, psychological, and environmental factors are all addressed.
Importantly, lifestyle interventions must be sustainable and individualized. There is no one-size-fits-all solution, and what works for one person may not work for another. When medications like naltrexone or Wellbutrin are used, they should be seen as tools within a broader toolbox—supporting, but not replacing, the internal work of healing and self-discovery.
The Role of Co-Occurring Conditions in Treatment Outcomes
One of the key challenges in treating BED is the high prevalence of co-occurring conditions. Depression, anxiety, ADHD, and substance use disorders are all commonly seen in individuals with binge eating disorder. These overlapping diagnoses complicate treatment but also provide opportunities for integrated care. Both naltrexone for binge eating and Wellbutrin for binge eating may be especially helpful in these contexts, as their pharmacological profiles allow them to target multiple symptom domains simultaneously.
For example, someone with BED and major depressive disorder may experience significant relief from Wellbutrin, which addresses both mood dysregulation and binge behaviors. Similarly, an individual with BED and a history of alcohol use disorder may benefit from naltrexone, which can curb both cravings for alcohol and food. This dual benefit enhances the efficiency of treatment and may improve adherence.
However, managing comorbidities requires careful clinical oversight. The presence of multiple diagnoses increases the risk of medication interactions, side effects, and psychological complexity. Coordination among healthcare providers—including psychiatrists, primary care physicians, therapists, and dietitians—is crucial to ensure safe and effective treatment. Integrated care models that emphasize communication and continuity have been shown to yield better outcomes for individuals with complex mental health needs.
Moreover, addressing comorbid conditions can have a ripple effect on binge eating behaviors. For instance, treating underlying anxiety can reduce emotional eating triggered by stress, while improving sleep hygiene can enhance impulse control and mood stability. In this way, the treatment of BED must be understood within the broader context of mental and physical health.
Considerations, Side Effects, and Monitoring
As with any pharmacological treatment, using naltrexone for binge eating or Wellbutrin for binge eating involves certain risks and considerations. Naltrexone, for example, can cause gastrointestinal discomfort, dizziness, and, in rare cases, liver toxicity. It is contraindicated in individuals with acute hepatitis or liver failure, and liver function should be monitored periodically during treatment.
Wellbutrin, while generally well-tolerated, carries a risk of increased anxiety, insomnia, and—at high doses—seizures. It is not recommended for individuals with a history of seizure disorders or eating disorders involving purging, such as bulimia nervosa. This makes accurate diagnosis essential, as the wrong medication can exacerbate symptoms rather than alleviate them.
Additionally, both medications require careful titration and regular follow-up to assess efficacy and side effects. Patient education is critical in this process. Individuals must understand what to expect from these medications, how to take them consistently, and when to report adverse effects. This informed approach fosters a sense of agency and collaboration, which is vital for long-term success.
Another consideration is the potential for relapse. Even with medication, binge eating can reemerge in times of stress or emotional upheaval. Continued engagement in therapy and self-care practices is essential to maintain progress. Relapse should not be seen as a failure, but as a signal that additional support may be needed.
Frequently Asked Questions (FAQ): Can Naltrexone or Wellbutrin Help with Binge Eating?
What are some lesser-known benefits of using Wellbutrin for binge eating beyond appetite suppression? Wellbutrin for binge eating has benefits that extend beyond simply curbing appetite. One important yet often overlooked advantage is its impact on executive functioning. Individuals with binge eating disorder often struggle with attention, planning, and impulse regulation—areas that Wellbutrin can help enhance through its dopaminergic and noradrenergic activity. This can lead to improved decision-making around food and better adherence to therapeutic strategies. Additionally, Wellbutrin has been noted to improve energy levels and motivation, which can make individuals more likely to engage in physical activity and other lifestyle behaviors that support long-term recovery from disordered eating patterns.
How does the timing of medication affect outcomes when using naltrexone for binge eating? The effectiveness of naltrexone for binge eating can be influenced by when the medication is taken relative to known binge triggers. Some clinicians recommend timing the dose to coincide with periods of heightened craving or emotional vulnerability, such as late afternoon or evening, when many individuals are more prone to binge episodes. Taking naltrexone preemptively during these windows may help blunt the anticipated dopamine-driven pleasure response to binge eating. This strategic timing can strengthen the medication’s ability to interrupt habitual patterns. Personalization of dosing schedules under medical supervision is key to optimizing treatment outcomes.
Is it possible to develop tolerance to naltrexone or Wellbutrin when treating binge eating? Unlike many medications used to treat addictive behaviors, tolerance to naltrexone for binge eating is not commonly reported in clinical practice. Naltrexone does not create a reinforcing high, so the brain is less likely to adapt in ways that require escalating doses. Similarly, while Wellbutrin for binge eating does influence dopamine and norepinephrine pathways, it does not generally result in tolerance when used as prescribed. However, some patients may feel the effects become less noticeable over time, which can be more about neurochemical stabilization than true pharmacologic tolerance. Periodic treatment reviews are essential to adjust strategies and ensure ongoing effectiveness.
What lifestyle factors can amplify the benefits of Wellbutrin for binge eating? While Wellbutrin for binge eating can be a powerful tool, its efficacy is often enhanced when combined with certain lifestyle practices. Regular aerobic exercise, for example, can synergize with the medication’s effects on dopamine by further improving mood and reducing food cravings. Consistent sleep patterns also support neurotransmitter regulation and reduce the fatigue that may trigger emotional eating. Nutritionally, a balanced intake of protein and complex carbohydrates helps stabilize blood sugar and reduces impulsive eating, complementing Wellbutrin’s role in mood stabilization. When these lifestyle elements are in place, the medication has a stronger foundation to deliver positive change.
Can naltrexone for binge eating be effective in people who do not identify with food addiction models? Yes, naltrexone for binge eating can still be effective in individuals who do not necessarily view their eating behaviors through the lens of addiction. Although the medication was originally developed for substance use disorders, its utility in binge eating is based more on its neurochemical effects than on adherence to any one theoretical model. Naltrexone helps reduce the rewarding properties of highly palatable foods, which can benefit people who binge eat in response to stress, routine, or emotional discomfort rather than addictive urges. For those with more cognitive-based triggers, naltrexone can still disrupt the feedback loop that perpetuates overeating behaviors.
How do clinicians determine whether to prescribe Wellbutrin or naltrexone for binge eating? The decision to prescribe Wellbutrin or naltrexone for binge eating is typically based on a patient’s symptom profile, medical history, and psychiatric background. For example, someone who struggles primarily with low mood, poor concentration, or fatigue alongside binge eating may be more likely to benefit from Wellbutrin due to its antidepressant properties. Conversely, individuals with strong cravings for specific foods or who describe a “high” from eating may respond better to naltrexone. In some cases, both medications may be used together, such as in the form of Contrave, to target multiple aspects of binge eating simultaneously. The clinician’s role is to tailor treatment to the patient’s unique neurobiology and personal context.
What are some strategies to manage initial side effects of naltrexone for binge eating? Some individuals starting naltrexone for binge eating experience side effects like nausea, headache, or fatigue, especially in the early weeks. Gradual titration of the dose can help mitigate these symptoms by allowing the body time to adjust. Taking the medication with food and staying hydrated throughout the day also helps reduce gastrointestinal discomfort. Patients can work closely with their healthcare providers to track side effects and adjust dosing as needed. Often, these symptoms are transient and resolve as the body acclimates, making it possible for patients to continue benefiting from the medication long-term.
Are there specific emotional or psychological profiles that predict better responses to Wellbutrin for binge eating? Emerging evidence suggests that individuals with certain emotional traits may respond more favorably to Wellbutrin for binge eating. For example, people who exhibit low levels of emotional reactivity but struggle with anhedonia and cognitive fatigue often report improved mood and motivation when using the medication. Additionally, those with depressive symptoms that worsen during periods of dietary restraint or weight gain may benefit from Wellbutrin’s capacity to regulate appetite and enhance energy. Individuals with co-occurring ADHD may also see improvement in both focus and eating behaviors due to the drug’s stimulant-like properties. These patterns highlight the importance of psychological assessment in determining the best treatment fit.
Can long-term use of naltrexone for binge eating lead to nutritional changes? Though naltrexone for binge eating is not directly associated with specific nutritional deficiencies, it can indirectly lead to changes in dietary habits. By reducing the pleasurable response to highly processed, calorie-dense foods, individuals may shift toward more nutrient-dense options over time. This behavioral shift can improve overall diet quality, especially when paired with nutritional counseling. However, some users may experience a temporary reduction in overall appetite, which could unintentionally lead to inadequate calorie or nutrient intake if not monitored. Regular check-ins with a dietitian can ensure that nutritional adequacy is maintained throughout treatment.
What role does self-monitoring play when using Wellbutrin for binge eating? Self-monitoring is a crucial complement to pharmacological treatment with Wellbutrin for binge eating. Keeping a daily log of eating patterns, emotional states, and medication timing can help patients and providers identify trends and refine treatment strategies. For instance, tracking may reveal a correlation between improved mood and reduced binge frequency, confirming the medication’s effect. It can also help pinpoint moments of vulnerability where additional coping strategies are needed. This reflective process empowers patients to play an active role in their own care and can foster a sense of agency in their recovery journey.
Conclusion: A Nuanced Path Forward in Binge Eating Treatment
In the evolving landscape of mental health and nutrition, the integration of medication into the treatment of binge eating disorder represents both progress and complexity. The emerging roles of naltrexone for binge eating and Wellbutrin for binge eating offer hope for individuals who have struggled with traditional approaches alone. By targeting key neurochemical pathways involved in reward, mood, and impulse control, these medications can help disrupt the cycle of binge eating and create space for meaningful behavioral change.
However, medication should never be viewed in isolation. The most effective treatment for BED remains holistic, combining medical support with psychological therapy, nutritional guidance, and lifestyle adjustments. Every individual brings a unique constellation of experiences, challenges, and strengths to the recovery journey, and treatment must honor that individuality.
For those considering pharmacological treatment, consultation with a qualified healthcare provider is essential. The decision to use medications like naltrexone or Wellbutrin should be grounded in a thorough understanding of the individual’s history, symptoms, and goals. When thoughtfully prescribed and supported with integrative care, these medications can be powerful tools in the pursuit of mental wellness and nutritional balance.
As research continues to shed light on the biology of binge eating and the potential of pharmacologic therapies, the path toward healing becomes clearer. It is a path that requires courage, commitment, and compassion—but one that is absolutely within reach.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
Naltrexone/bupropion for binge-eating disorder: A randomized, double-blind, placebo-controlled trial