Introduction: A Growing Concern for Today’s Youth
The teenage years are a critical stage of physical, emotional, and psychological development. Amidst hormonal shifts, academic pressures, social comparisons, and a search for identity, adolescents are especially vulnerable to a variety of mental health challenges. One area of increasing concern among healthcare professionals, educators, and parents alike is the rising incidence of eating disorders in teens. Eating disorders in adolescence are not only widespread but also deeply complex, often rooted in a combination of biological, psychological, and socio-cultural factors. Understanding how to support young individuals during this delicate period is essential, particularly through interventions that prioritize holistic wellness. One such approach is mindful nutrition, which can promote physical health, emotional resilience, and a more balanced relationship with food.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
In recent years, the media has drawn attention to the surge in cases of eating disorders and teenage girls have been especially affected. However, boys and nonbinary teens are also impacted, albeit sometimes in less visible ways. The gravity of childhood eating disorders, when left unaddressed, can result in long-term health consequences, including metabolic imbalances, organ damage, infertility, and increased risk of depression and suicide. Moreover, early intervention is key, as patterns established during adolescence often carry into adulthood. As we delve into the multifaceted nature of these conditions, it becomes evident that prevention and recovery are most effective when they involve a supportive environment, mental health guidance, and an informed approach to nutrition that encourages self-awareness and self-care.
Recognizing the Signs of Teenage Eating Disorders
Teenage eating disorders can manifest in a variety of forms, including anorexia nervosa, bulimia nervosa, binge eating disorder, and other less specified feeding and eating disorders. Recognizing the early signs is critical in initiating timely intervention. In some cases, these behaviors may be subtle at first: skipping meals, making frequent comments about body image, or engaging in secretive eating habits. Over time, these signs may escalate to more overt symptoms such as rapid weight loss, excessive exercise, withdrawal from social situations involving food, or unusual preoccupations with calorie counting and dieting.
Parents, caregivers, and educators must stay attuned to the behavioral, emotional, and physical indicators that may suggest the onset of eating disorders in adolescence. These conditions often co-occur with other mental health issues, including anxiety, depression, and obsessive-compulsive tendencies. Furthermore, eating disorders in children and teens are rarely about food alone; they often reflect deeper emotional struggles, such as a desire for control, low self-esteem, or unresolved trauma. This makes compassionate, nonjudgmental communication especially important when raising concerns with a teen.
It is also important to consider that not all teens with disordered eating behaviors will meet the full diagnostic criteria for an eating disorder. However, subclinical symptoms can still cause significant distress and functional impairment. Left unchecked, these patterns can progress into more severe conditions. Consequently, early recognition and professional evaluation are essential to improve outcomes and mitigate long-term risks.
Root Causes: Psychological, Biological, and Social Drivers
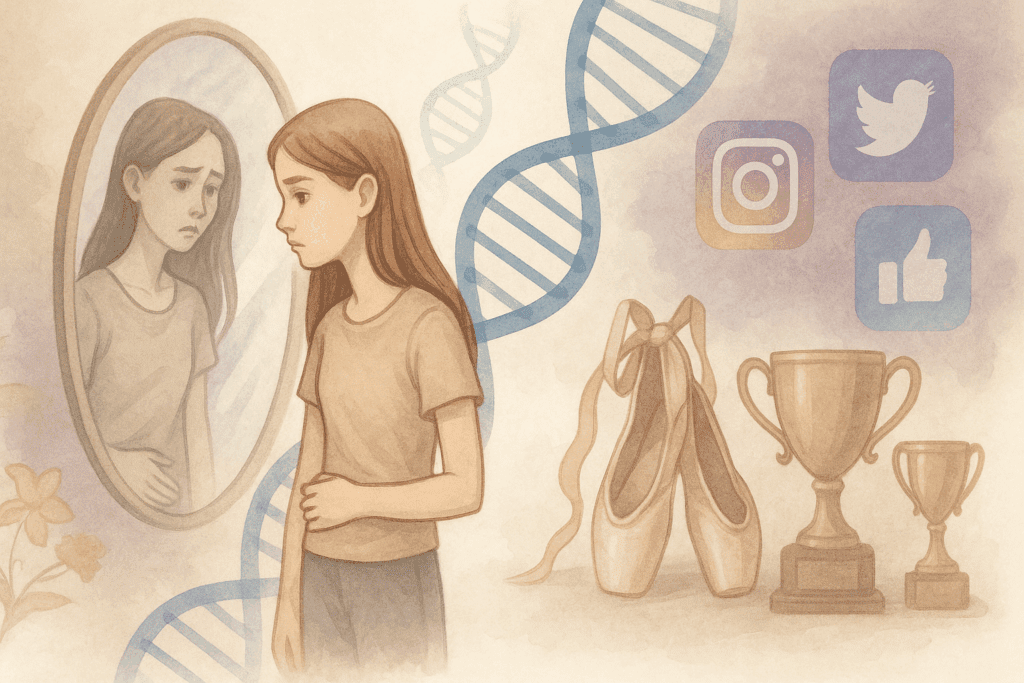
Understanding the root causes of eating disorders in teens requires a nuanced, multi-dimensional lens. On a psychological level, adolescents who struggle with perfectionism, low self-worth, or a history of trauma may be at higher risk. Biological factors also play a role, as genetic predisposition and neurochemical imbalances can influence appetite regulation, mood, and impulse control. Hormonal fluctuations during puberty may further exacerbate these vulnerabilities, making this developmental stage a uniquely sensitive period.
On a broader scale, the social environment contributes significantly to the prevalence of teenage eating disorders. In today’s digitally saturated world, social media platforms often promote unrealistic beauty ideals, leading many teens to engage in harmful comparisons and develop distorted body images. Peer pressure, bullying, and weight-related teasing can reinforce feelings of inadequacy, especially among eating disorders and teenage girls, who are often subjected to narrow societal standards of beauty. However, boys and gender-diverse teens are not immune; pressure to achieve a lean or muscular physique can also drive disordered eating behaviors in these groups.
Moreover, certain extracurricular environments—such as competitive sports, dance, or modeling—may inadvertently perpetuate disordered eating by emphasizing weight control or specific body types as a condition for success. These influences, when combined with underlying emotional issues, create a fertile ground for the development of eating disorders in adolescence. Addressing these root causes requires not just clinical intervention but also systemic changes in how society promotes and perceives health, beauty, and worth.
The Importance of Early Intervention and Multidisciplinary Care
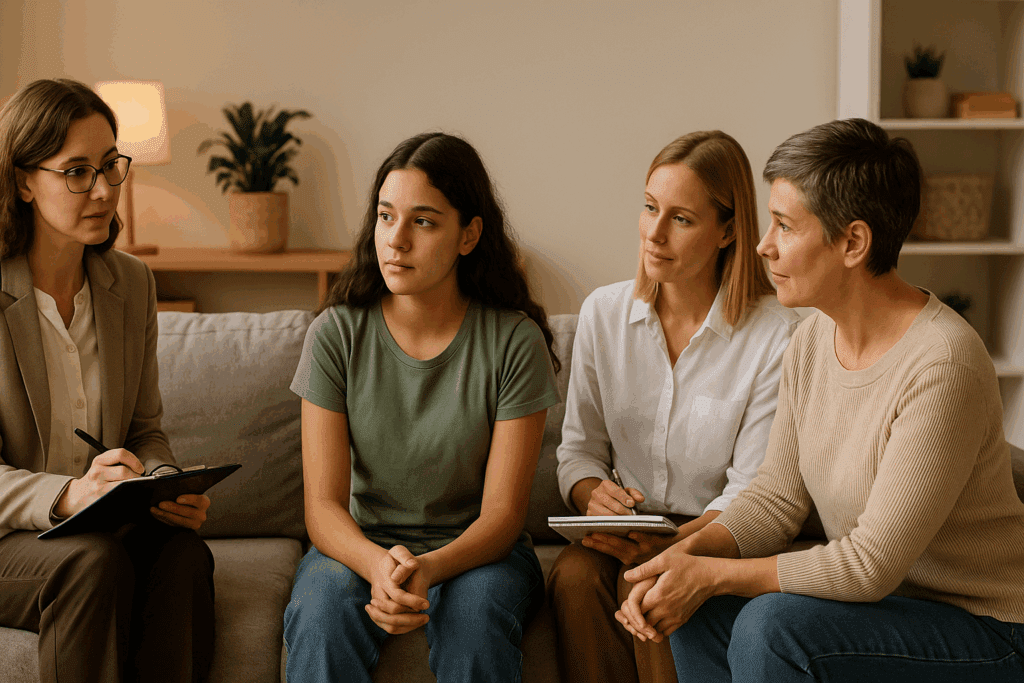
Early intervention in teenage eating disorders is crucial to improving recovery outcomes and preventing long-term physical and psychological consequences. The earlier a teen receives support, the more responsive they tend to be to treatment. Research indicates that family-based therapy (FBT), cognitive behavioral therapy (CBT), and nutritional counseling can all play integral roles in the healing process. These evidence-based approaches provide both structure and flexibility, helping teens rebuild a healthier relationship with food, body image, and self-concept.
Incorporating a multidisciplinary care team is often the most effective strategy for addressing eating disorders in children and teens. Psychiatrists, dietitians, therapists, pediatricians, and school counselors can work collaboratively to provide holistic support tailored to the teen’s unique needs. This comprehensive care model helps to address not only the disordered eating itself but also any co-occurring mental health conditions and environmental stressors that may be contributing to the behavior.
Equally important is family involvement. Parents and caregivers can play a pivotal role in both the detection and treatment of childhood eating disorders by creating a supportive and structured home environment. Empowering parents with education about the nature of eating disorders, as well as strategies for responding to meal-related anxiety and body image distress, can dramatically improve the effectiveness of treatment.

Mindful Nutrition as a Preventive and Supportive Strategy
Mindful nutrition represents a powerful and compassionate approach to supporting teens at risk for or recovering from eating disorders. Unlike traditional dieting, which often reinforces restriction and guilt, mindful nutrition encourages curiosity, self-awareness, and nonjudgmental attention to internal cues. This includes recognizing hunger and satiety signals, honoring cravings without shame, and cultivating a sense of gratitude and pleasure in the act of eating.
Integrating mindful eating practices into the daily lives of teens can foster a healthier relationship with food and body. For example, teaching adolescents to slow down during meals, savor flavors, and reflect on how different foods make them feel can help them reconnect with their bodies in a positive way. This shift away from external diet rules toward internal wisdom can be particularly healing for those recovering from teenage eating disorders, where the relationship with food has often been marked by fear and control.
Moreover, mindful nutrition aligns well with other therapeutic strategies such as intuitive eating and Health at Every Size (HAES), which promote body respect and self-compassion. In contrast to diet culture’s focus on appearance and weight manipulation, these approaches prioritize overall well-being, helping teens understand that health is not a one-size-fits-all concept. For teens navigating the challenges of adolescence and societal pressure, this message can be profoundly empowering.
The Role of Schools and Community in Prevention
Schools and community organizations have a vital role to play in the prevention and early identification of eating disorders in teens. Educational institutions can implement programs that teach students about media literacy, body image resilience, emotional regulation, and balanced nutrition. By fostering an environment of inclusivity and respect for diverse body types, schools can counteract some of the harmful messages that contribute to the development of eating disorders in adolescence.
Health education curricula that include evidence-based discussions on mindful eating, mental wellness, and the dangers of disordered eating can equip students with the tools they need to make informed choices. Moreover, training teachers, coaches, and school counselors to recognize the signs of eating disorders and intervene appropriately is crucial. These adults often spend significant time with students and may be among the first to notice changes in behavior or appearance.
Community initiatives such as peer support groups, mental health awareness campaigns, and parent education workshops can also serve as protective factors. These efforts can create a safety net that reinforces positive messages around self-worth, emotional intelligence, and holistic well-being. Together, schools and communities can act as a front line in both the prevention and early treatment of childhood eating disorders.
Parental Guidance and Family Dynamics in Healing
Parents and caregivers are often the most consistent and influential figures in a teen’s life. Their attitudes toward food, weight, and health can significantly shape a young person’s beliefs and behaviors. As such, fostering a home environment that emphasizes nourishment, balance, and open communication can play a crucial role in preventing eating disorders in children and adolescents.
Family meals, when approached mindfully and without pressure, can be a grounding ritual that offers connection and security. Encouraging positive body talk, avoiding weight-based criticism, and modeling a balanced relationship with food can all contribute to a healthier family dynamic. Parents should also be mindful of their own behaviors and language around dieting and exercise, as these can unintentionally send powerful messages to impressionable teens.
When a teen is in recovery from an eating disorder, the support and stability of their home environment are paramount. Structured meal plans developed with the help of a dietitian, consistent routines, and a low-stress atmosphere can all support healing. Additionally, family therapy can be an invaluable tool in addressing communication patterns, emotional expression, and relational dynamics that may be contributing to or affected by the disorder.

Addressing Stigma and Promoting Mental Health Literacy
Despite growing awareness, stigma remains a significant barrier to treatment for eating disorders and teenage girls and boys alike. Many teens fear being judged, misunderstood, or dismissed, which can prevent them from seeking help. In some cases, cultural beliefs or misinformation may lead families to minimize the severity of symptoms or delay professional intervention. Addressing stigma requires ongoing public education and a shift in how we talk about mental health.
Promoting mental health literacy can empower teens, parents, and educators to recognize the signs of distress and understand the pathways to support. Clear, compassionate messaging that eating disorders are not a choice or a phase, but legitimate medical conditions that require care, is essential. Public health campaigns, media representation, and inclusive policy initiatives can all help destigmatize these conditions and encourage earlier intervention.
Additionally, fostering open conversations about emotional well-being and normalizing the experience of seeking therapy can create a culture of support rather than shame. Schools, healthcare providers, and community leaders can model this openness by providing safe spaces and resources that prioritize empathy, inclusion, and holistic health.
Frequently Asked Questions: Understanding and Supporting Teens with Eating Disorders
1. How can eating disorders in teens affect long-term physical development?
Eating disorders in teens can significantly interfere with the body’s natural growth and development. Because adolescence is a time of rapid physical change, nutritional deficiencies caused by restricted eating or purging can lead to stunted growth, delayed puberty, and reduced bone density. In some cases, this can result in lifelong consequences such as brittle bones or compromised reproductive health. For teenage girls, irregular or absent menstrual cycles may signal underlying hormonal imbalances due to malnutrition. The earlier that eating disorders in adolescence are identified and treated, the better the chances of minimizing long-term developmental harm.
2. What role does social media play in the development of eating disorders in children and teens?
Social media can be a powerful influence on how children and teens perceive themselves. Platforms like Instagram, TikTok, and Snapchat often amplify narrow beauty standards and promote diet culture, which can fuel body dissatisfaction and disordered eating behaviors. This is especially relevant when it comes to eating disorders and teenage girls, who are statistically more likely to compare themselves to influencers or peers online. Constant exposure to filtered images and unrealistic portrayals of bodies can contribute to the internalization of harmful ideals. While social media is not the sole cause of eating disorders in children or adolescents, it can act as a catalyst for those already vulnerable to self-esteem issues.
3. Are there emerging therapeutic approaches for treating teenage eating disorders beyond traditional talk therapy?
Yes, several innovative approaches are being explored to supplement traditional therapy for teenage eating disorders. One such method is somatic therapy, which helps teens reconnect with their bodily sensations and foster trust in their physical experiences. Art and music therapies can also allow expression of emotions that may be too difficult to articulate verbally. For some adolescents, equine-assisted therapy has shown promise in building emotional awareness and resilience. These alternatives, when integrated with evidence-based treatments, offer new dimensions of healing for eating disorders in adolescence and can enhance engagement in the recovery process.
4. How do co-occurring mental health conditions complicate the treatment of eating disorders in teens?
Many teens with eating disorders also struggle with other mental health conditions, such as anxiety, depression, or post-traumatic stress disorder. These co-occurring conditions can complicate diagnosis and treatment, often masking the symptoms of the eating disorder or exacerbating the disordered behaviors. For example, a teen with anxiety may use food restriction as a way to exert control, while one with depression may engage in binge eating for emotional regulation. Treating eating disorders in adolescence thus requires a comprehensive approach that addresses both the eating disorder and any underlying psychiatric issues. An integrated care model is critical for effective, long-term recovery.
5. How can siblings be included in the recovery process for eating disorders in children or teens?
Siblings can play a supportive and constructive role in the recovery journey, but they may also experience confusion, resentment, or emotional distress themselves. Educating siblings about the nature of eating disorders in children and teens can foster empathy and reduce stigma within the family. Family therapy sessions that include siblings can provide a platform for honest dialogue and mutual understanding. Encouraging siblings to express their feelings while also equipping them with strategies to support their brother or sister can strengthen the family unit. Ultimately, inclusive family dynamics often promote better outcomes in the recovery process.
6. What are some lesser-known risk factors for eating disorders in adolescence?
While genetics, trauma, and social pressure are commonly recognized risk factors, others are less obvious but equally important. Perfectionism, for instance, is a significant psychological trait often present in teens with restrictive eating behaviors. Another emerging risk factor is gut-brain axis disruption, where gastrointestinal issues such as IBS may correlate with heightened anxiety around food. Additionally, teens who have experienced early puberty or have chronic illnesses may be at increased risk due to feelings of bodily difference or medical dietary restrictions. Understanding these nuanced contributors can help professionals and caregivers better address the roots of eating disorders in teens.
7. Can boys and nonbinary teens experience eating disorders differently than girls?
Absolutely. While eating disorders and teenage girls remain the most documented demographic, boys and nonbinary teens often present differently and are frequently underdiagnosed. For example, boys may prioritize muscle gain over weight loss, leading to disorders like muscle dysmorphia or compulsive exercise. Nonbinary teens might struggle with body image issues tied to gender dysphoria, which can manifest through disordered eating aimed at altering body shape. Because diagnostic criteria have historically been centered around female presentations, eating disorders in teens outside this norm may go unrecognized unless healthcare providers adopt a more inclusive lens. Greater awareness and gender-sensitive screening tools are essential for equitable care.
8. What strategies can educators use to support students showing signs of childhood eating disorders?
Educators are in a unique position to notice early behavioral changes, particularly in children and younger teens. When a student displays sudden shifts in eating habits, energy levels, or social interactions, it may signal the presence of childhood eating disorders. Teachers can support these students by maintaining open communication with school counselors and parents, ensuring the student feels safe and not stigmatized. Integrating media literacy and body positivity into health education curricula can also proactively counteract harmful messaging. Above all, teachers should model inclusive, respectful language around food and bodies to create a supportive classroom environment.
9. How do cultural backgrounds influence the presentation and treatment of eating disorders in teens?
Cultural values and norms play a significant role in how eating disorders in teens are experienced and treated. In some cultures, thinness may not be idealized, yet food-related shame or rigid family expectations can still contribute to disordered eating patterns. Stigma around mental health may also discourage teens from seeking help, particularly in communities where emotional expression is discouraged. Treatment models must therefore be culturally responsive, incorporating an understanding of familial structures, beliefs, and dietary customs. Addressing eating disorders in children from diverse backgrounds requires nuanced, culturally informed interventions to ensure accessibility and effectiveness.
10. What can recovery look like for a teen who has struggled with an eating disorder long-term?
Recovery from teenage eating disorders is rarely linear, especially for those who have struggled for years without diagnosis or treatment. The process often involves phases of relapse and renewal, and success may not always be defined by weight restoration alone. True recovery also means rebuilding a healthy relationship with food, developing emotional resilience, and regaining trust in one’s body. Teens in long-term recovery often benefit from peer support networks and continued therapy into young adulthood. With early intervention, tailored treatment, and family support, even those with long-standing eating disorders in adolescence can achieve meaningful, lasting change.
Conclusion: Creating a Culture of Support for Teens
Eating disorders in adolescence are complex and multifactorial, reflecting a delicate interplay between biological predispositions, psychological stressors, and socio-cultural influences. As the prevalence of these conditions continues to rise, particularly among eating disorders and teenage girls, it is imperative that we adopt a comprehensive and compassionate approach to prevention, treatment, and recovery. Mindful nutrition stands out as a particularly promising strategy, offering teens a way to reconnect with their bodies, cultivate self-compassion, and foster long-term wellness.
To address the growing challenge of eating disorders in teens, we must engage families, schools, healthcare providers, and communities in a unified effort. Early recognition, multidisciplinary care, and an environment that supports emotional honesty and body diversity are essential components of this effort. Just as childhood eating disorders affect more than just the individual, recovery too is a collective journey, one that is made stronger through empathy, education, and connection.
By prioritizing mental health literacy, dismantling stigma, and promoting holistic approaches such as mindful nutrition, we can better support the health and resilience of our youth. In doing so, we help lay the foundation for a healthier lifestyle—not just in adolescence, but across the entire life span. The time to act is now, with both urgency and hope, for the sake of the next generation and the world they will shape.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.