Introduction: Why a Holistic Lens Matters in Eating Disorder Recovery
Anorexia nervosa is one of the most complex and devastating psychiatric conditions, affecting not only the physical health of individuals but also deeply entwining itself within emotional, psychological, and social layers of life. Addressing anorexia requires more than a singular focus—it demands an integrative approach that treats both body and mind. For years, treatment centered almost exclusively around nutritional rehabilitation and psychotherapy. However, as our understanding of the condition has grown, so has the recognition that medications—specifically anorexia medication and other drugs for eating disorders—can play an essential role in a comprehensive recovery plan.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle
This evolution in treatment strategy underscores a broader shift in mental health care: one that prioritizes individualized, multifaceted support over one-size-fits-all solutions. Within this framework, the use of anorexia nervosa medication is not seen as a standalone cure but as part of a network of interventions that may include cognitive behavioral therapy (CBT), nutritional counseling, lifestyle restructuring, and community-based support. This article explores how drugs to treat anorexia are woven into the broader tapestry of holistic recovery. It also evaluates current evidence, clarifies misconceptions, and considers practical and ethical implications for individuals and care teams navigating this difficult terrain.
Understanding the nature, application, and limitations of anorexia nervosa drugs is a vital step toward demystifying their role in recovery. By exploring their use through the lens of science, lived experience, and holistic health philosophy, we can foster a more inclusive and effective approach to treatment—one that respects the individual’s journey and offers medically sound, evidence-based care grounded in compassion.
The Clinical Landscape of Anorexia Nervosa and Its Challenges
Before exploring anorexia medication in depth, it is crucial to understand the condition itself. Anorexia nervosa is not merely a refusal to eat or a desire to lose weight—it is a psychiatric disorder marked by a distorted body image, intense fear of gaining weight, and severe food restriction. These behaviors often stem from a complex interplay of genetic, psychological, social, and environmental factors, making treatment inherently challenging.
The chronic nature of anorexia nervosa and its alarmingly high mortality rate—one of the highest among psychiatric illnesses—demand an urgent and nuanced approach. Sufferers may resist treatment, hide symptoms, or present comorbid conditions such as anxiety, depression, or obsessive-compulsive disorder, all of which can complicate therapeutic interventions. The body’s physical decline—marked by malnutrition, organ damage, and hormonal imbalances—further limits the brain’s capacity to fully engage in cognitive therapies.
This intersection of physical deterioration and psychological rigidity means that interventions often require more than nutritional support alone. Drugs for eating disorders may be introduced not to eliminate symptoms in isolation, but to create a foundation on which other treatments can build. Whether targeting co-occurring mental health disorders or stabilizing neurochemical imbalances, anorexia nervosa medication can enhance responsiveness to therapy and facilitate deeper emotional healing.
In the past, reluctance to use medication in eating disorder treatment stemmed from a belief that pharmacological intervention might encourage avoidance of deeper psychological work. Today, however, clinical evidence supports a more balanced view—one where drug treatment for anorexia serves as a bridge rather than a barrier to lasting recovery.
Types of Anorexia Medication and Their Therapeutic Roles
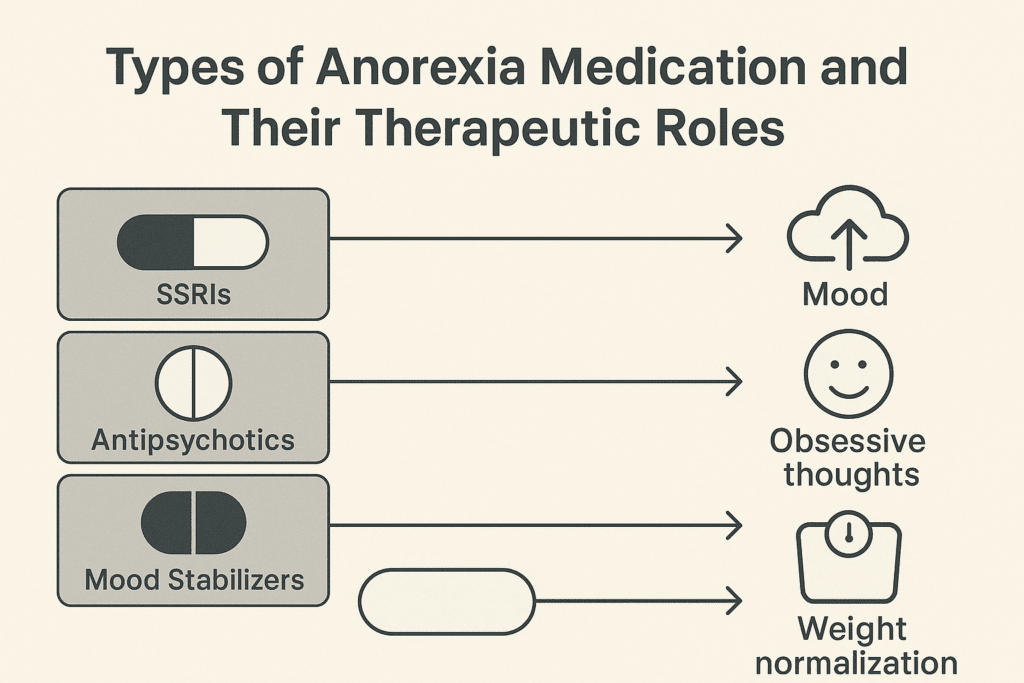
The phrase “anorexia medication” encompasses a range of pharmacological agents used to treat either core symptoms or related conditions such as anxiety and depression. No drug is currently FDA-approved specifically for anorexia nervosa itself, but several medications have shown promise in supporting recovery when used judiciously and in conjunction with psychotherapy.
Selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine, are among the most commonly prescribed drugs for eating disorders. While their efficacy in underweight anorexic patients is limited, they can be more helpful once a patient has regained some weight. SSRIs may alleviate anxiety, stabilize mood, and reduce obsessive thinking patterns, particularly in individuals who also struggle with depression or obsessive-compulsive traits.
Atypical antipsychotics, like olanzapine, have been studied for their potential to reduce distorted body image and food-related anxiety. These drugs may promote modest weight gain and decrease intrusive, distressing thoughts about body shape and size. Unlike older antipsychotic medications, atypical options tend to have fewer extrapyramidal side effects, making them more suitable for longer-term use in sensitive populations.
Mood stabilizers and anti-anxiety medications are also occasionally used as part of a broader treatment plan. For example, low-dose benzodiazepines might be administered prior to meals to ease anticipatory anxiety, although they are not recommended for long-term use due to risks of dependency. In cases of severe comorbid depression, medications such as mirtazapine—an antidepressant with appetite-stimulating properties—may offer dual benefits.
Although the search for drugs to treat anorexia specifically continues, the current pharmacological toolkit offers significant support for managing symptoms and enhancing therapeutic engagement. When viewed as part of a coordinated care plan, anorexia nervosa drugs can become vital contributors to a more stable and sustainable recovery process.
The Role of Medication Within a Holistic Treatment Framework
Holistic treatment for anorexia recognizes that true recovery is about more than weight restoration—it involves healing the mind, redefining self-worth, and creating sustainable lifestyle changes. In this model, drug treatment for anorexia is not a standalone solution but one piece of a much larger puzzle.
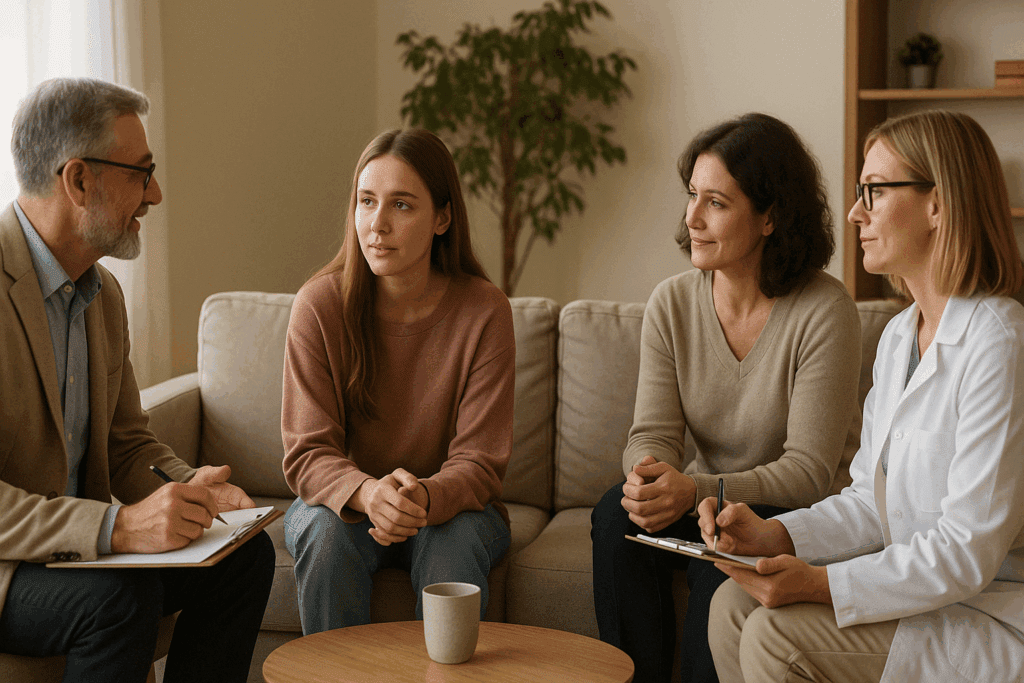
Therapeutic alliances play a foundational role. The decision to begin anorexia nervosa medication should be collaborative, involving the patient, psychiatrist, therapist, dietitian, and where appropriate, family members. This collective approach ensures that the medication supports rather than overshadows other aspects of care. For instance, while SSRIs might reduce intrusive thoughts, cognitive behavioral therapy remains essential for restructuring beliefs about food, body image, and control.
Nutrition therapy also forms a cornerstone of holistic care. As nourishment improves, the brain begins to function more optimally, increasing the effectiveness of both psychotherapy and pharmacological treatments. For this reason, medications may be more beneficial once the patient has reached a minimally healthy weight, allowing their body to properly metabolize the drug and their mind to process therapeutic insights.
Moreover, mindfulness-based interventions, such as yoga, guided meditation, and breathwork, can complement the use of drugs for eating disorders by helping individuals reconnect with their bodies in nonjudgmental ways. These practices can reduce stress, increase body awareness, and foster a sense of calm that supports long-term healing.
By weaving anorexia medication into a tapestry of psychosocial support, nutritional guidance, and lifestyle therapies, practitioners can create a recovery plan that acknowledges the multifaceted nature of eating disorders. This synergy not only promotes greater treatment adherence but also honors the complexity of each person’s journey toward wellness.
Risks, Limitations, and Ethical Considerations of Pharmacological Interventions
While anorexia nervosa drugs offer promising support, they are not without limitations or risks. One major concern lies in the physiological state of individuals with anorexia. Severe malnutrition can alter how the body processes medication, leading to unpredictable responses or increased sensitivity to side effects. For this reason, clinicians must approach drug treatment for anorexia with careful titration, close monitoring, and a readiness to adjust or discontinue medications if adverse effects arise.
Another challenge involves the psychological implications of medication use. Some individuals perceive taking anorexia medication as a sign of failure or weakness, which can hinder compliance and reinforce feelings of shame. It is essential that care teams frame pharmacological treatment as a tool—not a crutch—in the recovery process. By demystifying and destigmatizing the use of medications, practitioners can foster a more empowered, choice-driven path to healing.
Additionally, the absence of FDA-approved drugs specifically for anorexia means that most prescriptions are off-label. While this is a common and legal practice in psychiatry, it places added responsibility on providers to ensure that decisions are evidence-based, well-documented, and tailored to the individual’s clinical profile. Ethical concerns also arise around informed consent, particularly when working with adolescents or individuals whose decision-making capacity may be compromised by the illness.
From a systemic perspective, access to medication—and to the professionals qualified to prescribe and monitor it—can be limited by geographic, financial, or insurance-related barriers. Advocating for more inclusive, equitable mental health services is a vital step toward ensuring that everyone with an eating disorder can access the full range of treatment options, including medication when appropriate.
Ultimately, anorexia nervosa medication must be approached with clinical vigilance, ethical clarity, and a deep respect for the individual’s autonomy. Only then can it truly fulfill its role as a supportive element in a broader, holistic path to recovery.

Emerging Research and Future Directions in Anorexia Medication
The field of psychopharmacology is constantly evolving, and anorexia research is no exception. While no single drug has emerged as a definitive solution, ongoing studies are exploring novel compounds and combinations that may improve outcomes for individuals struggling with this disorder. Advances in neurobiology are shedding new light on the ways that starvation impacts brain function and emotional regulation, offering valuable insights into how drugs for eating disorders might be more effectively tailored.
One promising area of investigation involves the use of ketamine, a medication originally developed as an anesthetic and now repurposed for treatment-resistant depression. Preliminary studies suggest that ketamine’s rapid-acting effects on mood and cognition could offer benefits for individuals with anorexia, particularly those who experience profound anhedonia and emotional numbness. However, these applications remain experimental and must be approached with caution.
Another area of research focuses on the gut-brain axis and its role in mood and appetite regulation. Emerging evidence suggests that certain probiotics, prebiotics, and microbiome-focused interventions could enhance the effectiveness of traditional anorexia nervosa drugs by restoring gut health and improving neurochemical balance. Though still in early stages, these developments reflect the growing integration of nutritional science and mental health care.
Pharmacogenetics—the study of how genes affect a person’s response to drugs—also holds promise for the future of anorexia treatment. By identifying genetic markers that predict responsiveness or sensitivity to specific medications, clinicians may one day be able to craft personalized treatment plans with greater precision and fewer side effects.
As science continues to unravel the complexities of anorexia nervosa, the role of medication will likely expand in both scope and sophistication. While we are not yet at a point where drugs to treat anorexia can replace the need for comprehensive care, they are increasingly recognized as essential components of an integrated recovery model that values both medical innovation and human-centered healing.
Frequently Asked Questions: Understanding Anorexia Medication in a Holistic Recovery Framework
1. Can anorexia nervosa medication help with long-term recovery even after physical symptoms have stabilized? Yes, anorexia nervosa medication can continue to play a supportive role even after a patient has reached physical stabilization. Although the primary goal of early intervention is often nutritional restoration, long-term use of medication can assist in maintaining emotional regulation, reducing the likelihood of relapse, and addressing persistent psychological symptoms. Some individuals continue to experience intense anxiety, perfectionistic thinking, or obsessive-compulsive behaviors even when weight has normalized. In these cases, ongoing drug treatment for anorexia may offer cognitive and emotional balance that supports sustained recovery. It is important to work closely with a healthcare provider to evaluate whether prolonged use of anorexia nervosa drugs remains beneficial based on progress and symptom evolution.
2. How do clinicians determine which anorexia medication is most appropriate for each individual? Choosing the right medication for someone with anorexia involves careful consideration of multiple variables, including symptom profile, comorbid conditions, nutritional status, age, and previous responses to psychiatric medications. Clinicians often start with a low dose and adjust gradually, especially since malnutrition can alter drug metabolism. The decision process also involves balancing benefits against potential risks, particularly in the case of off-label drug use. For example, an individual with significant obsessive thought patterns may respond better to certain SSRIs, while someone with acute anxiety before meals might benefit from short-term anxiolytics. Ultimately, prescribing drugs for eating disorders is a nuanced process that requires a customized approach rooted in clinical expertise and patient feedback.
3. Are there innovative therapies that might enhance the effectiveness of drugs to treat anorexia? Yes, a number of complementary and emerging therapies are being explored to enhance the effectiveness of drugs to treat anorexia. For example, transcranial magnetic stimulation (TMS), a non-invasive brain stimulation technique, has shown promise when combined with anorexia nervosa medication. There’s also growing interest in combining pharmacological treatment with somatic therapies, such as trauma-informed yoga or neurofeedback, to target the nervous system more holistically. These adjunct treatments may help regulate physiological responses to stress, improve interoceptive awareness, and bolster the mood-stabilizing effects of medication. Integrating body-based practices with anorexia nervosa drugs offers a promising direction for individuals who have not fully responded to traditional interventions alone.
4. Why are some patients resistant to taking anorexia medication, and how can providers address this? Resistance to anorexia medication can stem from various psychological, emotional, and cultural factors. Some individuals fear losing control or believe that taking medication signifies weakness, while others may worry about side effects or weight gain. In certain cases, internalized stigma or past negative experiences with psychiatric drugs can fuel hesitation. Providers can help reduce resistance by engaging in open, nonjudgmental dialogue and emphasizing that drug treatment for anorexia is one piece of a multifaceted recovery plan. Framing medication as a tool for emotional clarity or distress reduction—not a standalone fix—can help build trust and promote a sense of agency in the healing process.
5. How do anorexia nervosa drugs affect cognitive function and decision-making in recovery? Cognitive distortions and impaired decision-making are hallmark features of anorexia nervosa. Certain medications, particularly SSRIs and atypical antipsychotics, have demonstrated the ability to improve these cognitive disruptions over time. By enhancing neurotransmitter function, anorexia medication may reduce rigid thinking patterns, promote flexibility, and help patients engage more effectively in therapy. This is especially relevant in the later stages of treatment when patients begin making choices about food, exercise, and lifestyle. Improved cognitive clarity, fostered by the use of anorexia nervosa drugs, can empower individuals to make healthier decisions that align with recovery goals.
6. Can drug treatment for anorexia help mitigate the impact of trauma in individuals with co-occurring PTSD? Yes, for individuals with a history of trauma or post-traumatic stress disorder (PTSD), drug treatment for anorexia can offer essential support. Many people with eating disorders use food restriction as a coping mechanism to manage the emotional aftermath of trauma. Anorexia nervosa medication—particularly medications that target both mood and anxiety—can help create psychological safety and reduce hyperarousal, allowing trauma work to begin more effectively in therapy. While medications are not a substitute for trauma-focused interventions such as EMDR or somatic experiencing, they can stabilize emotional reactivity and improve sleep, concentration, and tolerance for distress. This multifaceted strategy helps integrate trauma healing into the broader arc of eating disorder recovery.
7. What role do social and cultural factors play in how people respond to drugs for eating disorders? Social and cultural context significantly shapes how individuals perceive and respond to drugs for eating disorders. Cultural stigma around psychiatric medication, differing beliefs about mental illness, and family dynamics can all influence whether someone is open to using anorexia medication. Additionally, disparities in access to mental health care may affect the quality of treatment and medication adherence. Clinicians who practice cultural humility and acknowledge the lived experiences of their patients are better positioned to build rapport and foster medication compliance. Tailoring drug treatment for anorexia to account for cultural identity, language, and health literacy enhances both the ethical integrity and clinical effectiveness of care.
8. Are there risks of dependency or long-term side effects from anorexia nervosa drugs? While many anorexia nervosa drugs are considered safe for long-term use, there are important considerations regarding dependency and side effects. Benzodiazepines, for example, are not recommended for extended use due to the risk of tolerance, withdrawal, and dependency. Other medications, like atypical antipsychotics, may carry metabolic side effects such as increased cholesterol or insulin resistance. Regular monitoring through lab work and psychiatric evaluations is essential to minimize risk and adapt the treatment plan as needed. An informed and balanced approach to anorexia medication includes transparent discussions about side effects, lifestyle integration, and regular reassessment to ensure that benefits continue to outweigh any potential harms.
9. How might future innovations in neuroscience impact the development of drugs to treat anorexia? Advancements in neuroscience are likely to transform how we understand and develop drugs to treat anorexia. Researchers are beginning to map neural circuits involved in reward, habit formation, and interoception—all of which are disrupted in anorexia nervosa. This growing knowledge base may pave the way for more targeted treatments, such as medications that act on the dopamine or oxytocin systems to recalibrate emotional and bodily awareness. In the future, it’s plausible that personalized medicine—based on genetic profiles or brain imaging—will guide the selection of anorexia nervosa medication, increasing both efficacy and safety. These innovations promise to expand treatment possibilities while respecting the individuality of each patient’s recovery journey.
10. What are the most important factors in balancing medication with non-drug interventions in eating disorder recovery? The key to balancing anorexia medication with non-drug interventions lies in maintaining an integrated and person-centered care plan. Medication can reduce distressing symptoms and enhance participation in therapy, but it should never replace the therapeutic alliance, nutritional support, and lifestyle changes necessary for lasting healing. Timing is also important—some drugs for eating disorders work best after partial weight restoration, while others can help address acute distress in early stages. Clear communication among care team members and consistent reassessment of goals ensures that drug treatment for anorexia complements rather than overshadows other modalities. This holistic strategy promotes synergy between pharmacological and non-pharmacological approaches, cultivating a deeper, more sustainable recovery.
Conclusion: Rethinking Recovery with Compassionate, Evidence-Based Care
In the journey toward healing from anorexia nervosa, there is no single road, no universal timetable, and no magic pill. Recovery is as nuanced and personal as the individuals who undertake it. Yet, what emerges clearly from the growing body of research and lived experience is that medication, when used responsibly and in harmony with other treatments, can be a powerful ally. The role of anorexia medication in a holistic framework is not to overshadow therapy, nutrition, or mindfulness practices, but to support them—to offer stability, enhance resilience, and increase the effectiveness of therapeutic work.
Drugs for eating disorders are not a panacea, nor should they be viewed with suspicion or fear. They are tools, backed by evolving science and guided by ethical practice, that can open new doors for those whose lives have been narrowed by the grips of this disorder. By embracing an integrative approach—one that blends anorexia nervosa drugs with emotional support, nutritional care, and lifestyle interventions—we offer a more compassionate and comprehensive path forward.
As we move toward more personalized and inclusive treatment strategies, it becomes increasingly important to advocate for access, education, and empathy. Whether through innovative research, clinical best practices, or community advocacy, the goal remains the same: to help individuals not just survive anorexia, but to reclaim their lives with dignity, vitality, and hope.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.
Further Reading:
The Impact of Anorexia Nervosa and the Basis for Non-Pharmacological Interventions