The complexities of eating disorders are often obscured by societal misconceptions and generalizations, yet their effects can be profound and life-altering. Among these conditions, anorexia nervosa stands out for its dangerous physiological and psychological ramifications. When viewed through the lens of the DSM-5, or the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, the diagnostic criteria for anorexia nervosa present a structured, clinically validated framework that helps healthcare professionals identify, understand, and treat the disorder. As discussions about mental health and nutrition become more integrated, understanding the anorexia nervosa DSM-5 criteria offers a vital opportunity to identify early signs of starving and to foster healthier eating habits that support both physical health and emotional resilience.
You may also like: How to Stop Emotional Eating and Regain Control: Mindful Nutrition Strategies That Support a Healthier Lifestyle

A Look Into the DSM-5 and Its Role in Eating Disorder Diagnosis
The DSM-5 is the authoritative guide used by clinicians and researchers to diagnose mental disorders. Published by the American Psychiatric Association, it provides standardized criteria for diagnosing a wide range of mental health conditions, including the spectrum of eating disorders. These include anorexia nervosa, bulimia nervosa, binge-eating disorder, and avoidant/restrictive food intake disorder (ARFID). The DSM-5 eating disorders criteria serve as the foundation upon which assessments, treatments, and insurance coverage decisions are often based. Understanding the specificity and rationale behind these classifications is crucial for professionals and the public alike.
What are the main eating disorders according to DSM-5? This question not only aids in the comprehension of clinical terminology but also enhances the broader public’s awareness of behaviors that might otherwise be dismissed as mere quirks or personal habits. For anorexia nervosa specifically, the DSM-5 outlines a triad of diagnostic components: restriction of energy intake relative to requirements, intense fear of gaining weight or becoming fat, and a disturbance in the way one’s body weight or shape is experienced. These anorexia diagnostic criteria are vital in distinguishing the disorder from simple dieting or temporary weight loss.

Unpacking the Anorexia Nervosa DSM-5 Criteria
Each element of the anorexia nervosa DSM-5 criteria captures a different dimension of the disorder, and their interplay offers a multidimensional view of how anorexia develops and persists. The first criterion—restriction of energy intake—manifests in significantly low body weight in relation to age, sex, developmental trajectory, and physical health. This restriction is not accidental; it stems from a deliberate effort to control body size, often fueled by distorted beliefs about weight and self-worth. As such, the criteria for anorexia are not simply about how much a person eats, but why and how they make those choices.
The second diagnostic requirement is the intense fear of gaining weight, even when underweight. This fear can manifest through obsessive calorie counting, rigid exercise routines, or refusal to eat in social settings. It is not merely a fear but a deeply entrenched phobia that influences decision-making and daily functioning. This psychological element reinforces the fact that anorexia is not just a physical condition; it is a mental illness that requires therapeutic intervention.
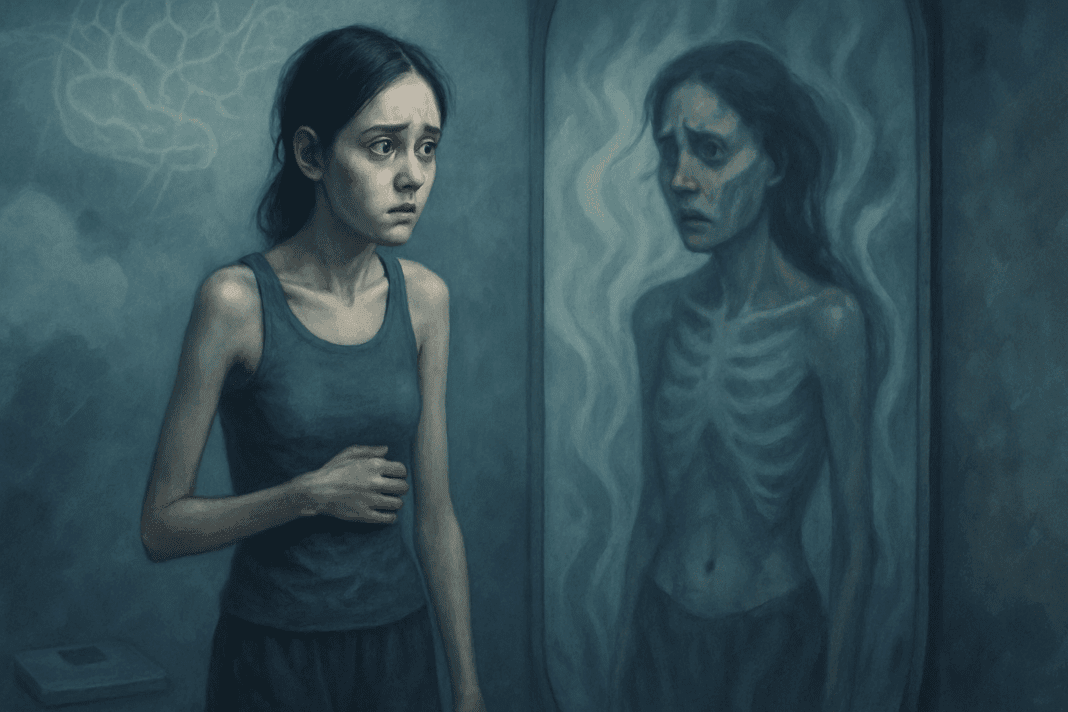
The third aspect—the distorted perception of one’s body—is perhaps the most insidious. Individuals diagnosed with anorexia nervosa are often described as possessing a profound disconnect between their actual body size and their perceived body image. Even when confronted with emaciated physiques, they may still see themselves as overweight. This body image distortion complicates recovery, as the person may not recognize the urgency of their condition. Understanding this component of the anorexia nervosa DSM criteria is essential for clinicians, caregivers, and support systems aiming to foster meaningful change.

Recognizing the Signs of Starving: Beyond the Physical Symptoms
Early identification of starving symptoms plays a pivotal role in the prevention and intervention of anorexia nervosa. These signs are not limited to obvious weight loss but often include subtle physical, emotional, and behavioral indicators. Cold intolerance, brittle nails, dry skin, dizziness, and fainting spells are among the more noticeable physical symptoms. However, emotional and psychological cues—such as irritability, social withdrawal, and preoccupation with food or weight—are equally significant.
When considering how to get anorexia—or more accurately, how individuals fall into anorexic behaviors—it’s crucial to recognize that no one sets out with the intent to develop a life-threatening disorder. More often than not, these behaviors evolve from a desire for control, perfectionism, or coping with stress. As the condition progresses, the signs of starving may be misinterpreted as dedication or self-discipline, particularly in cultures that idolize thinness. By understanding the anorexia DSM-5 criteria in tandem with these early signs, loved ones and clinicians can better discern when a dietary choice crosses the threshold into disordered behavior.
Is Anorexia a Mental Illness? Understanding the Psychological Depth
One of the most important clarifications to make is that anorexia nervosa is indeed a mental illness, as classified in the DSM-5. It intertwines emotional dysregulation, obsessive-compulsive traits, anxiety, and in many cases, trauma. For those who ask, “Is anorexia a mental illness?” the answer is unequivocally yes. This recognition shifts the conversation from one of blame or superficial understanding to one of empathy and clinical seriousness.
As a mental illness, anorexia affects not only a person’s relationship with food but also their cognitive functioning, emotional stability, and interpersonal relationships. Treatment therefore must go beyond nutritional rehabilitation. Therapeutic interventions, such as cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and family-based therapy (FBT), are essential in addressing the underlying psychological patterns that maintain the disorder. Understanding the diagnostic criteria for anorexia nervosa is a foundational step in crafting comprehensive treatment plans that prioritize both mental and physical health.
The Role of ARFID and the Broader Spectrum of Eating Disorders
While anorexia nervosa is often the most recognized eating disorder, the DSM-5 also highlights conditions like avoidant/restrictive food intake disorder (ARFID). The inclusion of ARFID DSM-5 criteria marks a significant evolution in how restrictive eating patterns are understood. Unlike anorexia, individuals with ARFID do not exhibit body image distortions or a fear of gaining weight. Instead, their restrictive eating is often linked to sensory sensitivities, fear of choking, or lack of interest in food. Despite these differences, ARFID can lead to significant weight loss, malnutrition, and psychosocial impairment.
Understanding what are the 4 eating disorder DSM-5 categories—anorexia nervosa, bulimia nervosa, binge-eating disorder, and ARFID—enables a more nuanced approach to diagnosis and care. Each condition presents unique challenges, but they all share a common thread: a disrupted relationship with food that negatively impacts health and well-being. Awareness of the broader spectrum of eating disorders, including eating disorder DSM-V updates, reduces stigma and increases the likelihood of accurate diagnosis and timely intervention.
Exploring the Diagnostic Challenges and Cultural Influences
Despite the detailed DSM-5 eating disorders criteria, diagnosing these conditions is not always straightforward. Cultural, ethnic, and gender-based factors can obscure symptoms or result in misdiagnosis. For example, eating disorders are often underdiagnosed in men, people of color, and older adults due to prevailing stereotypes that associate these disorders primarily with young, white women. These diagnostic blind spots highlight the importance of culturally competent care and a deeper understanding of how criteria anorexia manifests across diverse populations.
Moreover, societal norms around diet culture, fitness, and body aesthetics often mask early warning signs. Terms like “clean eating” or “wellness obsession” can cloak restrictive eating behaviors that align with anorexia DSM-5 criteria. This blurring of lines between health-consciousness and disordered eating underscores the necessity of clinical evaluation that prioritizes mental health perspectives. As eating disorder diagnosis becomes more sophisticated, it’s critical to educate the public about the risks of seemingly benign behaviors that may signal deeper concerns.
How Starvation Affects the Brain and Body: Scientific Insights
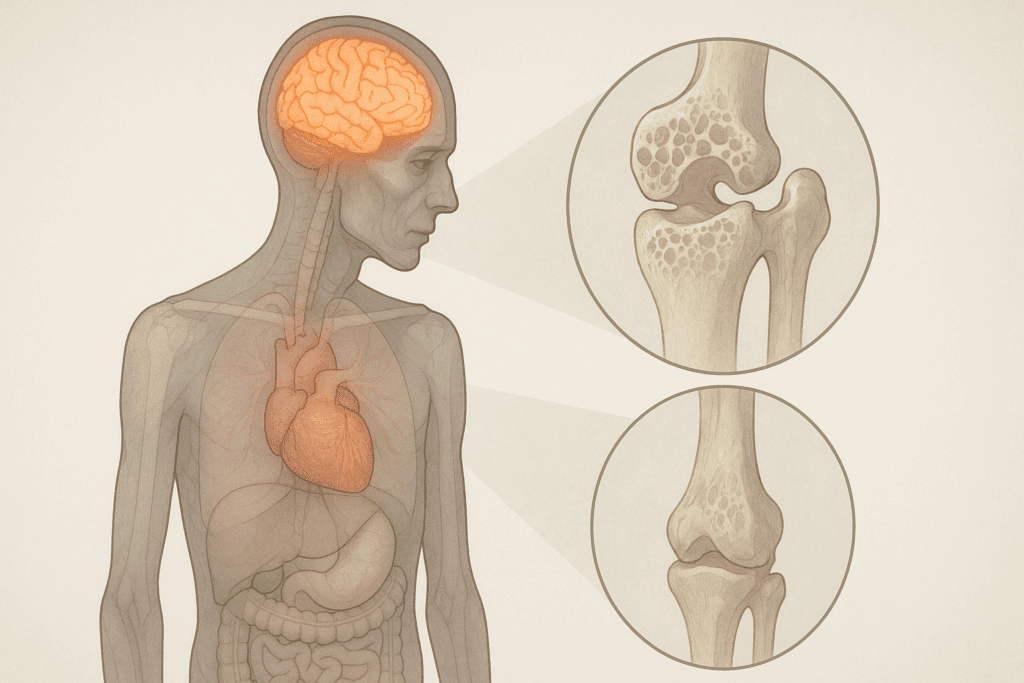
The physiological consequences of prolonged starvation reach far beyond weight loss. The human body responds to caloric deprivation with a series of adaptive but ultimately harmful changes. As the body tries to conserve energy, metabolic rate decreases, heart rate slows, and temperature regulation is impaired. These are often seen as signs of starving and can signal critical danger to those observing from the outside.
From a neurological standpoint, starvation alters brain function. Studies have shown reductions in gray matter volume, impaired executive function, and decreased connectivity in regions related to reward processing and emotion regulation. These changes support the argument that anorexia is not merely a behavioral choice but a neurobiologically reinforced illness. By exploring these scientific dimensions, we deepen our comprehension of why early intervention—guided by a clear understanding of anorexia nervosa DSM-5 criteria—is vital.

Reframing Recovery: From Diagnosis to Empowerment
While the DSM V anorexia nervosa classification provides the clinical foundation for diagnosis, the journey toward recovery is deeply personal and multifaceted. Recovery involves nutritional rehabilitation, psychological therapy, medical monitoring, and most importantly, a renewed relationship with food and self-image. It is not enough to meet the criteria for anorexia and receive a diagnosis; true healing requires support systems that honor the complexity of each individual’s experience.
Patients diagnosed with anorexia nervosa are often described as possessing a heightened sense of discipline, control, or sensitivity. These traits, when redirected through therapy and support, can become strengths rather than vulnerabilities. Eating disorder diagnostic criteria should not serve as labels of limitation but as tools that enable insight, awareness, and compassionate intervention. When treatment is individualized and holistic, it becomes possible not only to address disordered behaviors but also to cultivate resilience and emotional well-being.

Fostering Healthier Eating Habits Through Early Awareness
An integral aspect of prevention is education. Understanding the anorexia nervosa criteria empowers individuals to reflect on their own behaviors and those of loved ones. Conversations around food and body image should be grounded in empathy and evidence rather than judgment or fear. Encouraging mindful eating practices—such as intuitive eating, body neutrality, and nutritional education—can reduce the risk of disordered patterns taking root.
Moreover, addressing the influence of social media, diet culture, and perfectionism is critical. When young people are taught to value their bodies for function rather than appearance and are provided with accurate information about nutrition, the foundation for mental wellness is strengthened. Recognizing starving symptoms early on is not a matter of policing eating habits but of promoting self-awareness and support-seeking behavior. These shifts are essential in cultivating a culture where mental health and nutrition are seen as interdependent, not separate spheres.
Frequently Asked Questions: Understanding DSM-5 Anorexia Criteria and Starvation Symptoms
What makes anorexia nervosa so difficult to diagnose early, even with DSM-5 guidelines? Despite the detailed anorexia nervosa DSM-5 criteria, early diagnosis remains challenging due to how covert the behaviors can be. Individuals often mask restrictive eating with socially acceptable habits like clean eating or fitness routines, which don’t initially raise concerns. Moreover, the criteria for anorexia, while comprehensive, may not fully capture the cultural and individual nuances that affect how symptoms manifest. Subthreshold symptoms, where someone meets some but not all anorexia diagnostic criteria, may go unnoticed for years. This makes it essential for clinicians and caregivers to look beyond strict definitions and remain attuned to subtle behavioral shifts and emotional cues.
Are there any gender differences in how anorexia nervosa appears and is diagnosed using DSM-5 criteria? Yes, gender plays a significant role in both presentation and recognition. While DSM-5 anorexia criteria apply universally, males are less likely to be diagnosed due to societal misconceptions and stigma. For instance, muscle dysmorphia in men may align with some behaviors seen in anorexia nervosa but can be miscategorized as athletic discipline. Males may not verbalize the same fear of gaining weight but may engage in extreme caloric restriction and excessive exercise, still meeting DSM-5 eating disorders criteria. Because those diagnosed with anorexia nervosa are often described as possessing high self-control and perfectionistic traits, these patterns may be overlooked in men due to gender bias.
What role does technology and social media play in triggering behaviors aligned with anorexia nervosa criteria? Digital platforms increasingly expose users to curated images and diet-centric content, which can reinforce disordered thinking patterns. Algorithms on platforms like Instagram and TikTok often promote weight loss tips or body transformation challenges that align disturbingly well with how to go anorexic content. These influences can normalize behaviors that match anorexia DSM-5 criteria without individuals realizing they are engaging in disordered eating. The reinforcement loops created by social validation can exacerbate symptoms that meet the diagnostic criteria for anorexia nervosa. This makes digital literacy and mindful media consumption critical preventive strategies, especially among adolescents.
Can a person fluctuate between eating disorders defined in DSM-5, such as from anorexia to bulimia nervosa? Absolutely, eating disorders are fluid and may evolve over time. Someone initially diagnosed under anorexia nervosa DSM-5 criteria might later meet bulimia nervosa DSM-5 benchmarks if their behaviors change. This is particularly common in recovery or relapse phases where the individual struggles with bingeing episodes but still harbors the same cognitive distortions about weight and food. The DSM-5 eating disorders classification acknowledges that crossover diagnoses are common, especially when stress, trauma, or ineffective treatment is involved. Clinicians must therefore re-evaluate patients regularly to ensure an accurate eating disorder diagnosis.
How does ARFID differ from traditional anorexia, and why is its DSM-5 inclusion important? Avoidant/Restrictive Food Intake Disorder (ARFID), as outlined in ARFID DSM-5 criteria, differs fundamentally from anorexia in that it is not rooted in body image distortion or fear of weight gain. Instead, ARFID often stems from sensory sensitivities, trauma, or a fear of adverse reactions to food. Including ARFID in the DSM-5 eating disorders list broadens the understanding of restrictive eating beyond the stereotypical image of thinness. Someone with ARFID might show signs of starving but without the psychological drivers typical of anorexia. Its recognition ensures these individuals receive a legitimate eating disorder diagnosis and proper treatment without being dismissed due to normal weight or lack of body dysmorphia.
Is it possible to meet all DSM V anorexia nervosa criteria but still appear physically healthy? Yes, weight is only one of many variables. While anorexia nervosa DSM-5 criteria emphasize low body weight, they also stress psychological symptoms like fear of gaining weight and body image distortion. Atypical anorexia describes individuals who meet all other criteria anorexia conditions except for being underweight. These individuals may show classic signs of starving internally—such as electrolyte imbalance, low energy, and hormonal disruptions—without looking visibly ill. This underscores the importance of understanding anorexia nervosa criteria beyond superficial appearances.
What psychological traits are common in those diagnosed with anorexia nervosa, and how do they complicate recovery? People e diagnosed with anorexia nervosa are often described as possessing traits like perfectionism, high anxiety, and obsessive tendencies. These characteristics may initially serve them well in school or work but can drive rigid thinking around food and control. Recovery becomes more difficult because these traits make it hard for individuals to accept flexibility or relinquish control. Even when nutritional status improves, the psychological aspects rooted in the anorexia nervosa DSM-5 criteria often require long-term therapeutic work. Addressing these traits is just as critical as restoring physical health for sustainable recovery.
How do clinicians address the risk of patients researching how to get anorexia or maintain disordered behaviors? Unfortunately, some individuals seek out online communities that glamorize or instruct on how to get anorexia, creating a dangerous echo chamber. Clinicians must navigate this by discussing internet use openly during assessments and helping patients understand how these communities can reinforce harmful beliefs. While anorexia diagnostic criteria help identify behavioral patterns, ongoing therapy must address underlying reasons why someone would pursue these behaviors. Educating patients on the long-term damage of starvation symptoms—including cognitive decline and fertility issues—can be a deterrent. Creating a therapeutic alliance built on trust and honesty is essential to counteract harmful online influences.
What are some lesser-known long-term consequences of chronic starvation associated with anorexia nervosa? Beyond the immediate signs of starving, long-term consequences can include osteoporosis, chronic digestive issues, and irreversible cardiac damage. Cognitive impairments such as poor memory, slowed processing, and diminished decision-making capacity can persist even after weight is restored. These are not always evident in the initial anorexia nervosa DSM criteria but are crucial to address in treatment planning. Starving symptoms also have epigenetic effects, potentially influencing future offspring’s health. This highlights why early and sustained intervention—guided by a clear understanding of DSM 5 anorexia—is critical.
How can families support a loved one who meets anorexia DSM 5 criteria without reinforcing the disorder? Families often struggle to walk the line between concern and control. The best approach is education—understanding the anorexia nervosa DSM-5 criteria allows families to identify warning signs and offer support without judgment. Rather than focusing on food intake alone, it’s more productive to explore the emotions and fears driving the behavior. Creating a consistent, compassionate environment without ultimatums is vital. Long-term recovery is bolstered when families are engaged in therapy, helping reframe narratives around food and identity that may have contributed to meeting the anorexia dsm 5 criteria in the first place.
Reflecting on the DSM-5 Criteria for Anorexia Nervosa: A Pathway to Mental Wellness and Healthy Nutrition
The anorexia nervosa DSM-5 criteria are far more than a clinical checklist—they are a window into a deeply complex, emotionally charged, and potentially life-threatening condition. When viewed through a holistic lens, the criteria offer not only a means of diagnosis but a pathway toward understanding the psychological and physiological mechanisms that sustain disordered eating. Identifying the early signs of starving, especially when they coexist with perfectionism, body dissatisfaction, or anxiety, can prevent the progression of anorexia into its more severe forms.
By examining the full scope of DSM-5 eating disorders—from ARFID to bulimia nervosa—clinicians and the public alike are better equipped to recognize the diversity and complexity of these conditions. Whether considering how to go anorexic from a misguided place of control, or questioning why someone resists treatment, education and empathy remain the strongest tools we have. Clarifying that anorexia is a mental illness, not a choice, dissolves stigma and creates space for healing.
Ultimately, this knowledge must lead to action. Encouraging early intervention, advocating for compassionate care, and nurturing healthier relationships with food and body image are foundational steps in supporting those affected by eating disorders. As we deepen our understanding of eating disorder diagnosis through the DSM-5 and beyond, we create a more informed, empathetic, and health-conscious society—one that values both the science of nutrition and the soul of human experience.
Was this article helpful? Don’t let it stop with you. Share it right now with someone who needs to see it—whether it’s a friend, a colleague, or your whole network. And if staying ahead on this topic matters to you, subscribe to this publication for the most up-to-date information. You’ll get the latest insights delivered straight to you—no searching, no missing out.