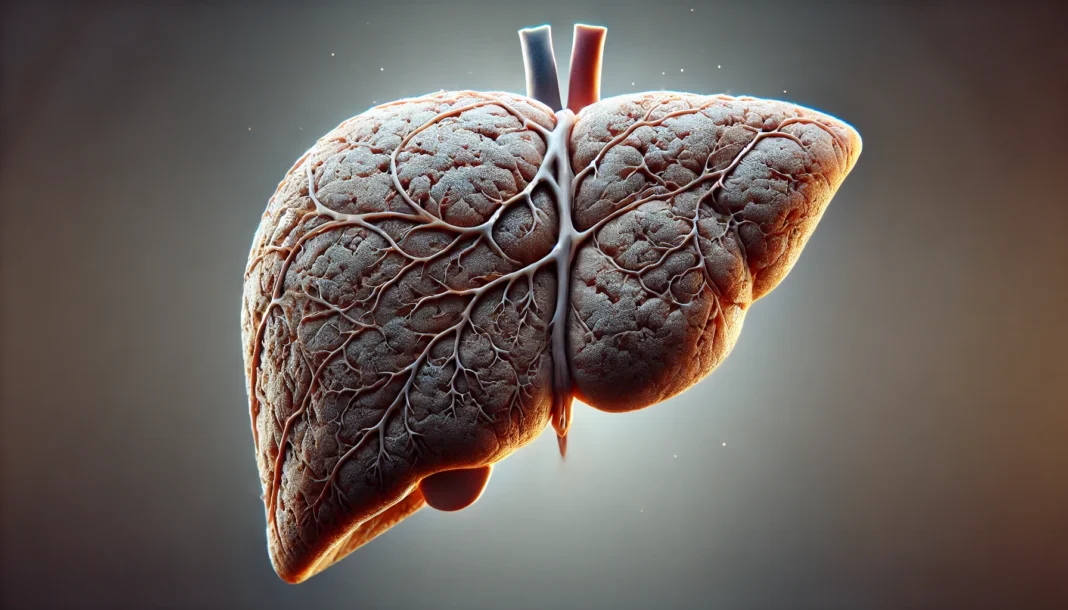
Liver fibrosis is a progressive condition that results from chronic liver injury and can lead to severe complications if left untreated. The liver, a crucial organ responsible for detoxification, metabolism, and immune function, can suffer from long-term damage due to various causes, leading to scarring known as fibrosis. Understanding what causes liver fibrosis, recognizing liver fibrosis symptoms, and identifying liver fibrosis stages is essential for early intervention and effective management. This article explores the fundamental aspects of hepatic fibrosis, including its stages, signs, and available treatment options, providing a comprehensive guide for those seeking to understand this serious condition.
You may also like: The Best Liver Detox Supplements: How to Choose Safe and Effective Support for Your Liver
What Causes Liver Fibrosis?
Liver fibrosis results from continuous injury to liver cells, prompting the activation of hepatic stellate cells, which produce excessive collagen and other extracellular matrix components. Over time, this leads to scarring, which disrupts the normal architecture and function of the liver. One of the most common causes of liver fibrosis is chronic hepatitis infection, particularly hepatitis B and C. These viral infections lead to persistent inflammation, progressively damaging liver tissue.
Another major contributor to liver fibrosis is excessive alcohol consumption. Alcoholic liver disease (ALD) is a well-documented condition that arises from prolonged and heavy alcohol intake, leading to liver inflammation, fat accumulation, and eventual fibrosis. Non-alcoholic fatty liver disease (NAFLD) and its more severe form, non-alcoholic steatohepatitis (NASH), are also significant causes, particularly in individuals with metabolic syndrome, obesity, or diabetes. NAFLD-induced fibrosis is increasing due to rising obesity rates worldwide.
Other causes of liver fibrosis include autoimmune liver diseases such as primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC), which lead to chronic bile duct damage. Additionally, genetic disorders like Wilson’s disease and hemochromatosis, which result in excessive accumulation of copper and iron in the liver, respectively, can lead to fibrosis. Drug-induced liver injury, exposure to toxins, and parasitic infections, such as schistosomiasis, also contribute to fibrosis development.

Recognizing Liver Fibrosis Symptoms
One of the challenges in diagnosing liver fibrosis early is the often subtle or absent symptoms in the initial stages. Many individuals remain asymptomatic until the condition progresses to more advanced stages. However, some hepatic fibrosis symptoms can emerge as liver function begins to decline.
Fatigue is one of the most commonly reported symptoms of liver fibrosis. Patients often experience unexplained tiredness and weakness due to metabolic changes and impaired detoxification processes in the liver. Another early symptom can be mild discomfort or pain in the upper right abdomen, where the liver is located. This discomfort arises from inflammation and liver enlargement.
As fibrosis advances, individuals may develop signs of impaired liver function, such as jaundice, characterized by yellowing of the skin and eyes due to bilirubin buildup. Other indicators include dark urine, pale stools, and persistent itching caused by bile salt accumulation in the skin. Swelling in the legs (edema) and abdomen (ascites) may occur due to reduced protein production by the liver, leading to fluid retention.
Gastrointestinal symptoms, including nausea, loss of appetite, and unexplained weight loss, can also indicate liver dysfunction. In some cases, easy bruising and prolonged bleeding times arise due to decreased production of clotting factors. Advanced liver fibrosis symptoms include cognitive issues like confusion and memory impairment, known as hepatic encephalopathy, which occurs when toxins accumulate in the bloodstream due to impaired liver filtration.
Stages of Liver Fibrosis
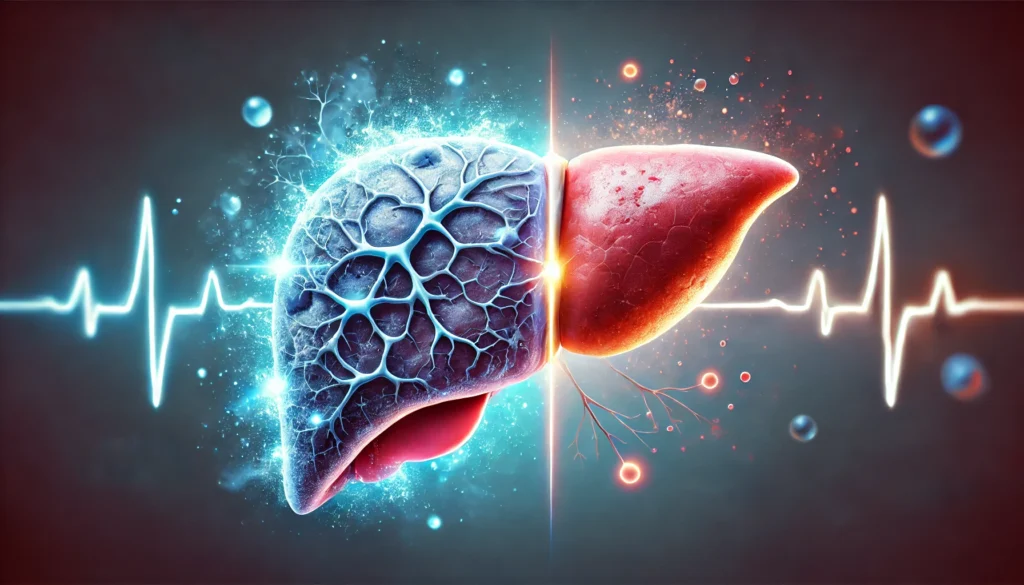
Liver fibrosis stages are classified using various scoring systems, with the METAVIR system being one of the most commonly used. This system categorizes fibrosis from stage 0 (no fibrosis) to stage 4 (cirrhosis). Understanding these stages is crucial for assessing disease progression and determining appropriate treatment strategies.
Stage 1 Liver Fibrosis: In stage 1 liver fibrosis, minimal scarring is present, and fibrosis is still reversible. At this stage, the liver remains functional, and symptoms are rare. Early intervention, such as lifestyle modifications and treating underlying conditions, can prevent further progression.
Stage 2 Liver Fibrosis: At stage 2 fibrosis, more significant scarring occurs, but liver function remains largely intact. While symptoms may still be mild or absent, medical evaluation and lifestyle adjustments become essential to slow disease progression. Dietary changes, weight management, and alcohol avoidance can help prevent further damage.
Stage 3 Liver Fibrosis: Stage 3 hepatic fibrosis, also referred to as bridging fibrosis, signifies substantial scarring between liver structures. This stage is concerning as it indicates a high risk of progression to cirrhosis. Individuals may begin experiencing more pronounced symptoms, such as fatigue, digestive issues, and fluid retention. Medical treatment and close monitoring are necessary at this stage to prevent further deterioration.
Stage 4 Liver Fibrosis (Cirrhosis): Stage 4 fibrosis, also known as f4 liver cirrhosis, represents end-stage liver disease. At this point, extensive scarring disrupts normal liver function, leading to complications such as portal hypertension, liver failure, and an increased risk of liver cancer. Symptoms at this stage include severe jaundice, ascites, encephalopathy, and variceal bleeding. Liver transplantation may be the only viable treatment option for patients with decompensated cirrhosis.
Is Liver Fibrosis Curable?
A common question among patients is whether liver fibrosis is curable. The answer depends on the stage at which fibrosis is diagnosed and the underlying cause. In early stages, liver fibrosis can be reversed with appropriate intervention. For instance, antiviral therapy can halt and even regress fibrosis in patients with hepatitis B or C. Similarly, lifestyle modifications, including weight loss and dietary improvements, can significantly reduce fibrosis in NAFLD patients.
However, once fibrosis progresses to cirrhosis, the damage becomes largely irreversible. While certain medications and treatments can slow disease progression and manage symptoms, complete reversal of f4 cirrhosis is unlikely. This underscores the importance of early detection and intervention to prevent severe liver damage.
Treatment Options for Liver Fibrosis
The treatment of liver fibrosis focuses on addressing the underlying cause, preventing progression, and, where possible, reversing damage. Antiviral medications are critical for patients with hepatitis-related fibrosis, while alcohol cessation is paramount for individuals with alcoholic liver disease. Weight loss, dietary changes, and insulin resistance management are essential in cases of metabolic-associated liver disease.
Emerging therapies, including antifibrotic agents, are being explored for their potential to reduce liver scarring. Some experimental drugs target fibrogenesis pathways to inhibit excessive collagen production. In advanced cases, liver transplantation remains the ultimate treatment option for those with irreversible liver failure.

Frequently Asked Questions (FAQ) About Liver Fibrosis
1. What causes liver fibrosis, and can it be prevented?
Liver fibrosis is primarily caused by chronic liver damage due to conditions such as viral hepatitis (hepatitis B and C), excessive alcohol consumption, non-alcoholic fatty liver disease (NAFLD), and autoimmune liver disorders. The process begins when the liver attempts to repair itself by producing excess collagen, leading to scarring. While liver fibrosis cannot always be prevented, adopting a liver-friendly lifestyle can significantly reduce the risk. Maintaining a healthy weight, avoiding excessive alcohol, getting vaccinated against hepatitis, and managing metabolic conditions like diabetes are essential preventive measures. Early detection and intervention are crucial to slowing its progression and preventing more severe stages of hepatic fibrosis.
2. What are the early liver fibrosis symptoms?
In its early stages, liver fibrosis symptoms are often subtle or completely absent, making early detection challenging. As the condition progresses, individuals may experience fatigue, mild discomfort in the upper right abdomen, and unexplained weight loss. Some people also develop signs of liver dysfunction, such as jaundice (yellowing of the skin and eyes) or easy bruising due to impaired clotting function. Advanced cases may lead to swelling in the legs and abdomen, which can indicate worsening liver damage. Regular liver function tests and imaging studies can help identify fibrosis before noticeable symptoms develop.
3. What are the different liver fibrosis stages, and how do they affect health?
Liver fibrosis is classified into five stages, ranging from F0 (no fibrosis) to F4 (cirrhosis). Stage 1 liver fibrosis involves minimal scarring with no significant impact on liver function. Stage 2 liver fibrosis shows moderate scarring but still allows the liver to function relatively well. Stage 3 fibrosis represents severe scarring with impaired liver function, and stage 4 fibrosis, also known as F4 cirrhosis, indicates extensive scarring leading to liver failure. As fibrosis progresses, the risk of complications such as liver cancer and portal hypertension increases. Early diagnosis and treatment can slow or even halt the disease’s advancement.
4. How does stage 3 liver fibrosis differ from earlier stages?
Stage 3 liver fibrosis is a critical turning point in disease progression. Unlike stage 1 or stage 2 fibrosis, where the liver can still function efficiently, stage three liver fibrosis involves substantial scarring that disrupts normal liver function. At this stage, blood flow within the liver may be impaired, leading to complications such as portal hypertension (increased pressure in the liver’s blood vessels). Individuals with stage 3 hepatic fibrosis may start experiencing noticeable symptoms like fatigue, fluid retention, and digestive issues. Medical intervention, lifestyle modifications, and strict monitoring are essential to preventing further deterioration.
5. Is liver fibrosis curable, or can it only be managed?
The reversibility of liver fibrosis depends on its stage and underlying cause. In the early stages (stage 1 or stage 2 fibrosis), removing the trigger—such as treating hepatitis or stopping alcohol use—can allow the liver to heal and fibrosis to regress. However, stage 3 hepatic fibrosis and stage 4 hepatic fibrosis are much harder to reverse, and cirrhosis (F4 cirrhosis) is generally considered permanent. Although a complete cure is not always possible, medical treatments, dietary adjustments, and lifestyle changes can significantly slow progression and improve liver function.
6. What are the key liver fibrosis signs that indicate disease progression?
While liver fibrosis signs may be mild in early stages, more severe indicators appear as the condition advances. Common warning signs include persistent fatigue, abdominal discomfort, jaundice, and swelling in the legs and abdomen. People with advanced fibrosis may develop spider-like blood vessels on their skin, dark urine, or pale stools due to bile flow disruption. If fibrosis progresses to cirrhosis, complications such as confusion (hepatic encephalopathy) and gastrointestinal bleeding may arise. Regular monitoring through blood tests and imaging scans is crucial for assessing disease progression.
7. How is liver fibrosis diagnosed, and what tests are used?
Doctors use a combination of blood tests, imaging techniques, and sometimes liver biopsy to diagnose fibrosis. Blood tests measure liver enzymes and fibrosis markers to detect inflammation and scarring. Non-invasive imaging tests like FibroScan and MRI elastography assess liver stiffness, helping determine the fibrosis stage. In cases where precise evaluation is needed, a liver biopsy may be performed to directly analyze tissue samples. Early diagnosis is key to managing liver fibrosis effectively and preventing irreversible damage.
8. What are the risks of stage 4 liver fibrosis (F4 cirrhosis)?
Stage 4 fibrosis, or F4 cirrhosis, represents the most advanced form of liver fibrosis, where extensive scarring impairs liver function. At this stage, the liver struggles to perform essential tasks such as detoxification, protein synthesis, and bile production. Individuals with F4 liver cirrhosis face increased risks of liver failure, ascites (fluid buildup in the abdomen), esophageal varices (enlarged veins prone to bleeding), and liver cancer. Regular medical supervision, medication, and, in severe cases, a liver transplant may be required for survival.
9. Can lifestyle changes help slow the progression of liver fibrosis?
Yes, lifestyle changes play a crucial role in managing liver fibrosis and preventing further damage. Reducing alcohol consumption, following a balanced diet rich in fruits, vegetables, and lean proteins, and maintaining a healthy weight can help protect liver function. Managing conditions like diabetes and high cholesterol is equally important since metabolic disorders contribute to fibrosis progression. Regular physical activity and avoiding unnecessary medications or toxins that strain the liver can also make a significant difference. In many cases, adopting these habits can slow the disease and improve overall well-being.
10. Are there any promising treatments or research advancements for liver fibrosis?
Ongoing research is exploring new treatments to halt or reverse liver fibrosis. Scientists are investigating antifibrotic drugs that target liver scarring at a molecular level. Clinical trials are also examining the role of stem cell therapy in regenerating liver tissue. Additionally, researchers are studying compounds like ursodeoxycholic acid and antioxidants that may protect liver cells from further damage. While no universal cure currently exists, advancements in gene therapy and immunotherapy hold promise for future treatments. Patients should stay informed about emerging therapies and consult their doctors about potential participation in clinical trials.
Conclusion: Protecting Your Liver and Managing Fibrosis
Liver fibrosis is a progressive condition that can lead to serious health consequences if not detected and managed early. Understanding what causes liver fibrosis, recognizing liver fibrosis signs, and being aware of different liver fibrosis stages are crucial steps toward effective prevention and treatment. While early-stage fibrosis can be reversed through lifestyle changes and medical interventions, advanced fibrosis requires careful management to prevent complications. By prioritizing liver health, seeking regular medical evaluations, and adopting a liver-friendly lifestyle, individuals can reduce their risk of severe liver disease and maintain optimal well-being.
chronic liver disease, hepatic scarring, liver fibrosis progression, managing liver health, fatty liver disease treatment, alcohol-induced liver damage, metabolic liver disease, liver detoxification, non-alcoholic fatty liver, viral hepatitis complications, primary biliary cholangitis, liver health strategies, liver disease prevention, hepatic function support, liver-friendly diet, cirrhosis risk factors, advanced liver disease, portal hypertension symptoms, hepatic encephalopathy, liver transplant eligibility
Further Reading:
LIVER FIBROSIS: Pathophysiology and Clinical Implications
Liver fibrosis – from bench to bedside
Molecular and cellular mechanisms of liver fibrosis and its regression
Disclaimer
The information contained in this article is provided for general informational purposes only and is not intended to serve as medical, legal, or professional advice. While NewsHealthWatch strives to present accurate, up-to-date, and reliable content, no warranty or guarantee, expressed or implied, is made regarding the completeness, accuracy, or adequacy of the information provided. Readers are strongly advised to seek the guidance of a qualified healthcare provider or other relevant professionals before acting on any information contained in this article. NewsHealthWatch, its authors, editors, and contributors expressly disclaim any liability for any damages, losses, or consequences arising directly or indirectly from the use, interpretation, or reliance on any information presented herein. The views and opinions expressed in this article are those of the author(s) and do not necessarily reflect the official policies or positions of NewsHealthWatch.